
The Mindful Compassion Program Integrated with Body-Mind-Spirit Empowerment for Reducing Depression in Lung Cancer Patient-Caregiver Dyads
Fei-Hsiu Hsiao1, 2, Chao-Chi Ho3, Chong-Jen Yu4, 5, Jin-Yuan Shih3, Zhong-Zhe Lin5, 6, Feng-Ying Huang7, Yu-Ting Chen8, 9, and Chia-Chen Hsieh10
1School of Nursing, College of Medicine, National Taiwan University, Taipei, Taiwan; 2Department of Nursing, National Taiwan University Hospital, Taipei, Taiwan; 3Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan; 4National Taiwan University, Hospital Hsinchu Branch, Taiwan; 5Department of Internal Medicine, National Taiwan University College of Medicine, Taipei, Taiwan; 6Department of Medical Oncology, National Taiwan University Cancer Center, Taipei, Taiwan; 7Department of Education, College of Education, National Taipei University of Education, Taipei, Taiwan; 8School of Nursing, College of Medicine, Chang Gung University, Taoyuan City, Taiwan; 9Department of Psychiatry, New Taipei Municipal TuCheng Hospital, New Taipei City, Taiwan; 10School of Nursing, College of Nursing, Taipei Medical University, Taiwan
https://doi.org/10.5093/pi2025a1
Received 22 April 2024, Accepted 30 September 2024
Abstract
Objective: This study compared the long-term effects of a mindful compassion program on improving depression in lung cancer patients, both in patient-caregiver dyads and in patient-only groups, and examined the moderating roles of anxiety and quality of life (QOL). Method: Participants consisted of 56 dyads, who were randomly assigned to either the dyadic or patient-only groups. Data collection included various assessments at different time points: baseline (T0), end of intervention (T1), and follow-up at the 5th month (T2), 8th month (T3), and 14th month (T4). Results: Patients in the dyadic group experienced a significant reduction in depressive symptoms. The dyadic intervention was particularly beneficial for younger patients and those with higher baseline QOL symptom distress. Improvements in patients’ mindfulness and self-compassion contributed to reduced depression by enhancing general health and lowering anxiety. Additionally, caregivers’ self-compassion played a role in reducing patients’ depression by improving patients’ QOL functioning and decreasing anxiety. Conclusions: Mindfulness and compassion interventions, whether provided dyadically or individually, can be tailored to each patient’s specific condition.
Keywords
Dyadic depression program, Depressive symptoms, Anxiety, Mindfulness awareness, Self-compassionCite this article as: Hsiao, F., Ho, C., Yu, C., Shih, J., Lin, Z., Huang, F., Chen, Y., & Hsieh, C. (2025). The Mindful Compassion Program Integrated with Body-Mind-Spirit Empowerment for Reducing Depression in Lung Cancer Patient-Caregiver Dyads. Psychosocial Intervention, 34(1), 1 - 9. https://doi.org/10.5093/pi2025a1
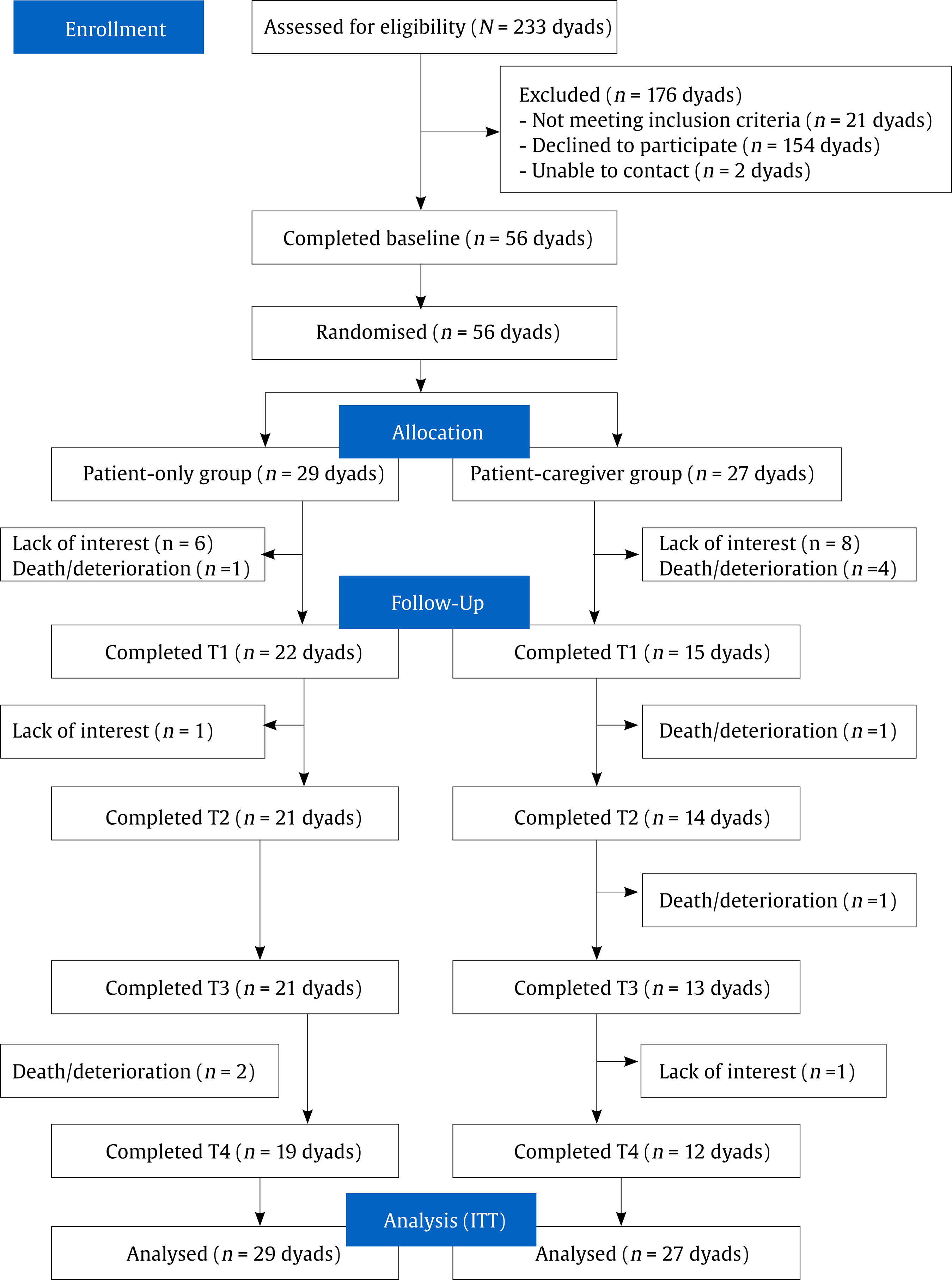
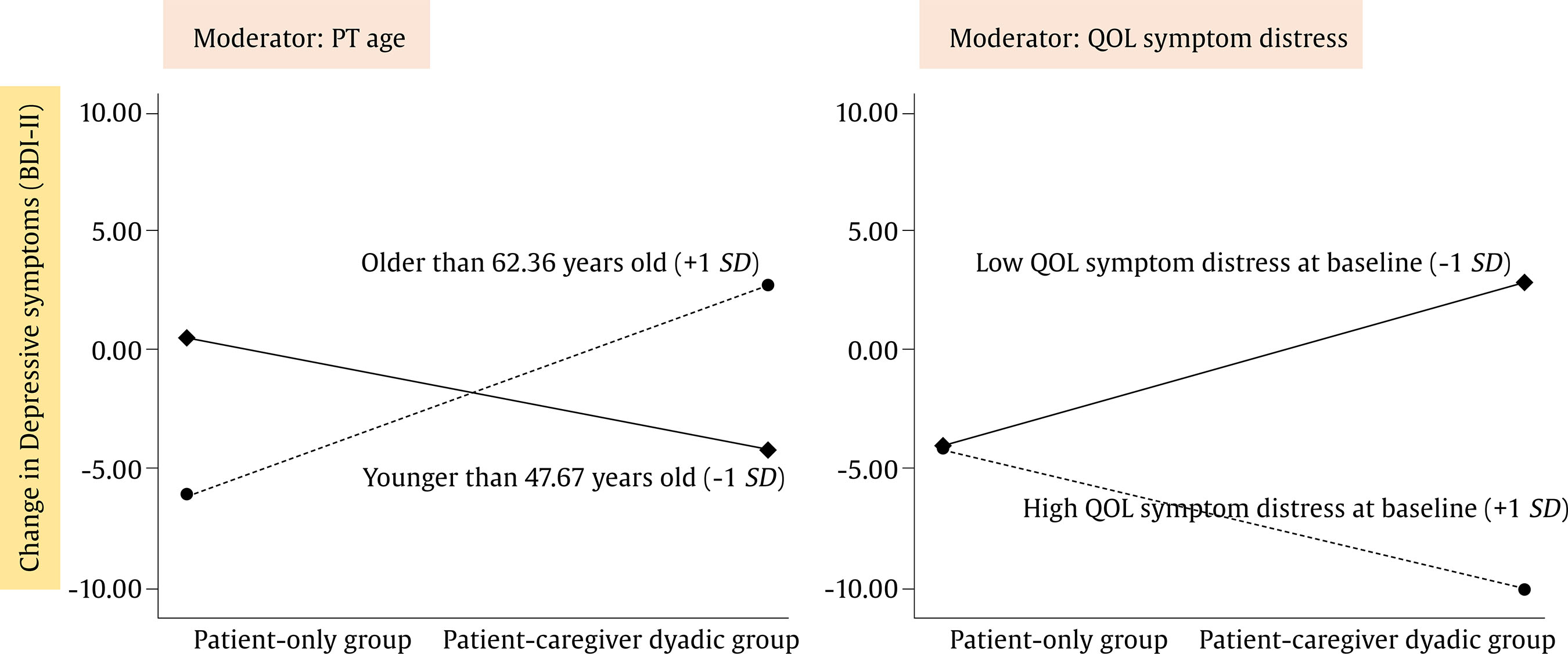
Correspondence: cchsieh1116@gmail.com (C-C Hsieh).Lung cancer is the most common type of cancer and the leading cause of cancer-related death globally (Vijayvergia et al., 2015). Depressive symptoms in lung cancer patients are associated with poor quality of life, elevated levels of inflammation biomarkers and cortisol, and worse progression-free survival rates (Andersen et al., 2023; Zeng et al., 2024). The review study found that approximately 40% of caregivers of cancer patients exhibit clinical levels of depression that impact their quality of life (Bedaso et al., 2022). Both lung cancer patients and their families experienced significant depression and anxiety for at least one year after diagnosis (Aubin et al., 2022). Depression and intimacy issues have been observed between lung cancer patients and their primary caregivers (Li et al., 2022). Enhancing the emotional regulation skills of cancer caregivers could reduce their own depression and mitigate the psychological burden on patients (Baudry et al., 2024). Evidence suggests that patient-caregiver dyadic interventions can improve their emotional distress and quality of life (Badr et al., 2019). However, in the study by Badr et al. (2015) some lung cancer patients reported discomfort discussing illness-related issues in the presence of their loved ones during the dyadic psychosocial program. It remains unclear whether including family caregivers in dyadic interventions yields better outcomes than the patient-only interventions, and for whom these dyadic interventions are most effective. The meta-analysis on depression programs for lung cancer patients found that effective interventions must incorporate both psychotherapy and psychoeducation to address the underlying causes of depressive symptoms, including physical symptoms and psychological distress (Hsieh & Hsiao, 2017). The integrative body-mind-spirit (BMS) therapy, developed by Chan (2001), emphasizes the interconnection between body, mind, and spirit and aims to transform clients’ suffering into growth experiences through holistic empowerment strategies. The physical-strength activities in this therapy include qi-gong exercises, diaphragmatic breathing, and guided imagery. The mind-strength activities involve discussing personal growth during the experiences of cancer and practicing forgiveness and self-love. The spiritual-strength activities focus on exploring life’s losses and gains, practicing letting go of attachments and desires, and learning to view death as a mentor in the search for life’s meaning. The meta-analysis by Li et al. (2022) indicated that integrative BMS therapy can improve physical health, depression/anxiety, and quality of life for both patients and caregivers. Hsiao et al. (2022) designed an intervention program that combined mindfulness training with integrative BMS group therapy. Mindfulness, which involves being aware of inner experiences in the present moment with non-judgment, helps individuals regulate their cognition more flexibly when faced with life adversities (Shapiro et al., 2006). The mindfulness practices included in the program helped lung cancer patients manage cognitive problems affecting respiratory distress, such as loss of breath control, fear of death, uncertainty about the future, and rumination on past events. The study found that mindfulness combined with BMS therapy alleviated depressive symptoms and general quality of life issues in lung cancer patients during a 14-month follow-up, compared to BMS alone (Hsiao et al., 2021). A meta-analysis on mindfulness for cancer patients found that improvements in depression and quality of life were more pronounced in female patients (Xunlin et al., 2020). Another meta-analysis on depression programs, which included psychoeducation with CBT or interpersonal therapy, showed that the effects did not last beyond 4 months (Hsieh & Hsiao, 2017). The combined mindfulness and BMS therapy demonstrated similar effects on depression and quality of life for both male and female lung cancer patients, with reduced depression effects lasting for 14 months. This study highlights that integrated mindfulness with BMS therapy can enhance physical and emotional well-being in lung cancer patients. Mindfulness combined with BMS therapy has not been developed within dyadic programs for lung cancer patients and caregivers, although a few dyadic mindfulness programs have been explored. A 3-month study with a non-RCT design found that an 8-week Mindfulness-Based Stress Reduction (MBSR) program, which included psychoeducation and mindfulness practices, did not produce significant improvements in anxiety and depression for 19 lung cancer patients and 16 caregivers (van den Hurk et al., 2015). However, participants reported that the MBSR program facilitated greater insight into their bodily sensations, acceptance of their illness, and improved communication with their families. Another 3-month study using an RCT design demonstrated that an 8-week MBSR program, combined with usual care (cancer treatment and supportive care), significantly improved anxiety, depression, quality of life, mindfulness skills, self-compassion, and rumination in 31 patients. Nevertheless, there were no significant changes in the partners’ outcomes (Schellekens et al., 2017). These studies (Schellekens et al., 2017; van den Hurk et al., 2015) suggest that while an MBSR group program with a dyadic approach may help improve anxiety, depression, and quality of life for lung cancer patients, the effects on family caregivers have been inconsistent. To address the limitation of the 3-month follow-up in these studies, further research is needed to explore the long-term depression effects of dyadic mindfulness programs for lung cancer patients and their caregivers. Meta-analyses (MacBeth & Gumley, 2012) and another study (Pinto-Gouveia et al., 2014) have indicated that higher levels of self-compassion are associated with lower levels of depression and anxiety in both non-clinical samples and cancer patients. An 8-month follow-up study (Hsieh et al., 2021) also demonstrated that self-compassion was linked to lower depressive symptoms among family caregivers of lung cancer patients. Additionally, Schellekens et al. (2017) found that mindfulness and self-compassion in lung cancer patients and their spouses were negatively related to psychological distress and could buffer their partners’ distress. These findings suggest that dyadic self-compassion training could have positive effects on both lung cancer patients and their partners by reducing depression. The moderating analysis indicates that lung cancer patients with higher levels of depression may benefit more from dyadic Mindfulness-Based Stress Reduction (MBSR) interventions (Schellekens et al., 2017; van den Hurk et al., 2015). Future research should identify the moderators related to clinical features and depressive levels within a dyadic mindfulness and compassion program for lung cancer patients and their caregivers. Additionally, the mechanisms through which mindfulness and compassion impact depression need further exploration. Previous studies have reported that MBSR can positively affect anxiety, depression, and quality of life. A meta-analysis including two studies on cancer patients (primarily breast cancer) demonstrated that psychotherapy’s effects on reducing depression are associated with improvements in quality of life (Kolovos et al., 2016). The mindfulness-to-meaning theory suggests potential mechanisms by which mindfulness practices enhance positive emotional regulation, thereby improving depression, quality of life, and meaning in life (Garland et al., 2015; Garland et al., 2017). According to this theory, mindfulness can reduce individuals’ focus on threats and decrease anxiety arousal. Mindfulness enhances metacognitive awareness and promotes decentering from cancer threats, leading to better stress reappraisal, active coping, savoring daily life, and positive emotions. Therefore, mindfulness practices may reduce the impact of anxiety related to cancer threats and improve quality of life, which in turn could reduce depression in lung cancer patients. Gilbert et al.’s (2017) emotional regulation model suggests that cultivating self-compassion and receiving compassion from others can significantly impact emotional regulation, particularly in mitigating automatic threat responses like anger and anxiety. They propose that self-compassion enables individuals to better manage their psychological and emotional needs, enhancing their empathy and ability to savor the present moment. This approach is also thought to positively affect perceptions of compassion received from others, potentially leading to better emotional regulation. For lung cancer patients and their caregivers, self-compassion training might improve emotional regulation and overall quality of life. The effectiveness of such training in reducing depression, especially whether it is more beneficial for patients alone or for both patients and caregivers together, needs further investigation. Mediating analyses are suggested to explore how self-compassion or mindfulness might impact depression through quality of life or reduced anxiety. This 14-month study aims to examine: (1) the long-term effects of a dyadic mindfulness compassion group program on reducing depressive symptoms in patients and caregivers; (2) the moderating effects of clinical features and baseline psychological distress on the outcomes of the dyadic intervention; and (3) how patients’ anxiety symptoms, quality of life, and caregiver stress mediate the effects of mindfulness or self-compassion on depressive symptoms in both patients and caregivers. Participants This study with 14-month follow ups adopts the randomized controlled trial (RCT) design. The patients who were diagnosed as non-small cell lung cancer, aged at least 20 years old were recruited from outpatient department of divisions of surgery and oncology at the general hospital. Their family caregivers were also invited to participate in this study when they were identified by the patient as the primary family caregiver and who are aged at least 20 years old. A total of 233 potential participants were contacted, 21 did not meet the inclusion criteria, 2 were unable to be contacted, and 154 declined to participate. The primary reasons for declining included lack of interest in the research program, time constraints, and personal reasons. In the end, as indicated in Figure 1, the 56 couples (n = 29 in the control group, n = 27 in the intervention group) completed baseline assessments (T0), 37 couples (66.1%) at T1, 35 couples (62.5%) at T2, 34 couples (60.7%) at T3, and 31 (55.4%) couples participated at T4. Attrition was due to patient’s death or disease progression (n = 9) and no time to participate in the group or completing follow ups (n = 16). There were no differences in the attrition between groups (p > .05). Participating dyads who dropped out before T4 were similar to those who completed T4 in most patients’ and caregivers’ baseline characteristics and main outcome variables assessed at baseline (p > .05). However, caregivers with an undergraduate degree or above were more likely to complete all research assessments than those with a high school education and below (p = .01). Caregivers with a job were more likely to complete all research assessments than those without a job (p = .005). Table 1 showed the baseline characteristics for intervention and control group separately. Lung cancer patients and caregivers in both groups showed no statistically significant differences in their baseline characteristics (all p > .05). Additionally, there were no significant differences between groups in any of the outcome measures at baseline (all p > .05). Table 1 Demographic and Clinical Characteristics for LC Patients and Caregivers at Baseline   Note. 2Multiple response. Procedure Upon approval from the institutional review board of the study hospital, research assistants initiated patient recruitment within the surgery and oncology outpatient departments. Caregivers were then invited through the patients if the caregivers did not come with them. Prior to participation, all individuals provided written informed consent following a comprehensive explanation of the study’s objectives and ethical considerations by a research assistant. After the participants completed the baseline measurements (T0), they were randomly allocated to one of two groups: the experimental group, which engaged in a 2-month, 120-minute weekly session of Body-Mind-Spirit (BMS) therapy combined with mindfulness and compassion group therapy for both patients and caregivers; or the control group, where patients participated in the same 2-month BMS with mindfulness compassion group therapy (120 minutes weekly), while caregivers received informational materials at home. Assessments of their conditions were conducted at the conclusion of the 2-month intervention (T1), as well as at the fifth month (T2), eighth month (T3), and fourteenth month (T4) intervals thereafter. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol for this study has received approval from the Institutional Review Board of the National Taiwan University Hospital (REC No: 201812074RINA). Intervention The intervention program was conducted in a group format, lasting 120 minutes per week for 2 months, for both the experimental and control groups. The only difference between the groups was that, in the experimental group, patients and their caregivers participated together as a dyadic group. In contrast, in the control group, only the patients attended the sessions, while their caregivers received information at home. The intervention consisted of several components: education and symptom management, holistic body-mind-spirit (BMS) empowerment skills, mindfulness, and compassion-focused skills. According to our previous study integrating mindfulness with BMS for lung cancer patients (Hsiao et al., 2021), the educational content covered disease and treatment information, side effect management, and health behaviors (such as healthy eating, regular exercise, smoking cessation, and sleep hygiene). The BMS activities included body work (body movements through qi-gong exercises with focusing on the present moment), mind work (discussing personal and family growth related to living with lung cancer, practices of forgiveness, self-love, and love for significant others), and the spiritual work (exploring the nature of life and death, the meanings of loss and gain, practicing detachment and letting go of desires, searching for meaning in life). The structured mindfulness skills encompassed the concept of mindfulness (lectures on awareness, non-judgment, non-reactivity, acceptance, and letting go), mindful breathing (focused on breathing in the present moment with inner strength, such as courage and appreciation), body scan, and seated mindful nature meditation. The compassion-focused skills, based on the therapy developed by Gilbert and Choden (2014), included creating a warm and encouraging tone in one’s mind, listening to self-love letters with a compassionate voice, performing a compassionate hand touch on the chest, engaging in self-compassion meditations, receiving compassion from others, and extending compassion to others. For the structure of each session, in the first hour, the group members began with a 15-minute qi-gong exercise. This was followed by approximately 30 minutes of practicing mindfulness and compassion-focused skills. The rest of the session was dedicated to educational content and symptom management, as well as discussing homework related to BMS empowerment strategies. At the end of the session, participants were introduced to the weekly BMS homework and encouraged to practice qi-gong, mindfulness, and compassion skills (such as mindfulness breathing and meditations) using our mobile app. The participants could use the group LINE app for real-time consultations regarding physical or psychological distress, free sharing, and mutual support. Measures Patients only: European Organization for Research and Treatment of Cancer Core Cancer Quality of Life Questionnaire (EORTC QLQ-C30) and its lung and breast cancer specific complementary measure (EORTC QLQ-LC13). Caregivers only: Kingston Caregiver Stress Scale (KCSS). Patients & Caregivers: BDI-II depression scale, Mindful attention awareness scale, Self-compassion scale, and State-Trait Anxiety Inventory (STAI). Main Outcome Variable Beck Depression Inventory (BDI) consists of 21 item sets, each with a series of four statements. The scores of the 21-item BDI-II scale (Beck et al., 1961) range from 0 to 63. The internal consistency reliability of the BDI-II was good in the current study (α = .95). Predictor Variables The 15-item Mindful attention awareness scale (MAAS) measures the frequency of individual’s open (or receptive) awareness and attention to what is occurring in the present moment, and assesses to what extent individual uses mindfulness in day-to-day life (Carlson & Brown, 2005). The 13-item self-compassion scale (SC) consists of an engagement subscale assessing the individual’s ability of being sensitive to their own distress/suffering and engagement with suffering, and an actions subscale assessing the individual’s ability to be motivated to alleviate and prevent distress (Gilbert et al., 2017). Each item is rated on a 10-point Likert scale ranging from 1 (never) to 10 (always). Both MAAS and SC can be summed for a total score, with higher scores indicating higher mindfulness awareness and self-compassion. In the current study, the internal consistency reliability estimates were adequate for both MAAS (α = .88) and SC (α = .76). Mediator Variables The 20-item State-Trait Anxiety Inventory (STAI) developed by Spielberger (1970) measures state anxiety. The sum score has a range from 20 to 80, with higher scores indicating greater anxiety. The STAI showed good reliability in the current study (α = .96). The 30-item EORTC QLQ-C30 and 13-item EORTC QLQ-LC13 were used to measure QOL in cancer patients in clinical trials (Aaronson, 1993). The QLQ-C30 combines five functional scales (physical, role, cognitive, emotional, and social), three symptom scales (fatigue, pain, and nausea/vomiting), and global health status. The QLQ-LC13 includes lung cancer-associated symptoms (cough, hemoptysis, dyspnea, and site-specific pain), treatment-related side effects (sore mouth, dysphagia, peripheral neuropathy, and alopecia), and pain medication. Higher scores for the functioning scale indicate better functioning, whereas higher scores for symptom scales represent higher/worse symptom distress. The subscale of QOL showed acceptable internal consistency, with ranging from α = .73 to .95. Kingston Caregiver Stress Scale (KCSS) developed by Sadak et al. (2017) measures subjective stress related to caregiving issues, family issues, and financial issues. The internal consistency reliability of KCSS was good in the current study (α = .92). Data Analysis Data were analyzed for lung cancer patients and their caregivers separately, using IBM SPSS version 25. Missing data were assessed at the scale level, and the analysis confirmed that missing data were missing completely at random (MCAR), χ2(11) = 10.34, p = .500. Therefore, we utilized all available data points for parameter estimation without imputing the missing values. This approach ensures efficient and unbiased estimates under the MCAR assumption. Descriptive statistics were used to analyze sample characteristics and dropout rates. Baseline differences between groups and between those that completed the study versus dropped out were analyzed using two-tailed t-tests and chi-square tests. The generalized estimating equation (GEE) with the autoregressive, AR (1), correlation structure was used to estimate the effects of intervention on patients’ and caregivers’ depressive levels over 14 weeks of follow-up. A significant effect of time indicates that there are significant changes in outcomes over time overall (across both groups). A significant interaction effect of time and group tested the significant differences in primary outcome between groups during 14 months. All potential moderators were measured at baseline. We examined moderators of intervention effects on the primary outcome of depression using PROCESS macro model 1, conducting a separate model for each potential moderator variable. Significant moderator effects were explored by comparing simple slopes for the association between predictor (PT-only vs. patient-caregiver dyadic group) and primary outcome of depression, and testing if they were significantly different from zero. To advance understanding of how and why interventions work, we also examined mediators of intervention, using PROCESS macro model 4 (Hayes, 2017). Mediation models tested that the effect on depression and meaning in life by the change in mindfulness or self-compassion was mediated by the change in the potential mediators (anxiety, quality of life or caregiver stress). Bootstrapping with 5,000 resamples was used to calculate a confidence interval (CI) around the indirect effect. An indirect effect is considered significant if the CI does not include zero. There were no significant differences between groups in the effects on patients’ depression, Wald’s χ2(4) = 5.227, p = .265, or caregivers’ depression, Wald’s χ2(4) = 1.946, p = .746. Within the patient-caregiver dyadic group, reductions in patients’ depressive symptoms over time were observed, Wald’s χ2(4) = 10.435, p = .034. However, there were no significant within-group differences observed in caregivers’ depression, either in the patient-caregiver dyadic group or in the patient-only group. As shown in Figure 2, moderator analyses were further performed to explore which subgroups of patients and caregivers benefit most (or least) from patient-caregiver dyadic or patient only program. The association between treatment groups and change in patients’ depressive symptoms was found to be moderated by age (B = 0.943, t = 2.556, SE = 0.369, p = .017) and QOL symptom distress at baseline (B = -0.686, t = -2.507, SE = 0.274, p = .019). As shown in Figure 2, simple slopes revealed that the effect of patient-caregiver dyadic intervention on patients’ depressive symptoms was in favor of patients who were younger and had more QOL symptom distress at baseline. As noted, caregivers’ factors did not play any moderator role. Possible mechanisms for effectiveness of the mindfulness compassion with BMS program were further assessed. As shown in Figure 3, change in the patients’ anxiety significantly mediated the effect of the patients’ mindfulness on their depressive symptom (effect = -2.570, Boot SE = 1.315, 95% Boot CI [-5.459, -0.266]). Change in the patients’ anxiety also significantly mediated the effect of the caregivers’ self-compassion on the patients’ depressive symptom (effect = -0.192, Boot SE = 0.113, 95% Boot CI [-0.486, -0.043]). The mediation paths revealed that the changes in the patients’ mindfulness and caregivers’ self-compassion over 14 months reduced patients’ anxiety, in turn, decreased patients’ depressive symptom. Figure 3 Mediation Effects. Unstandardized Path Coefficients and SE in brackets.  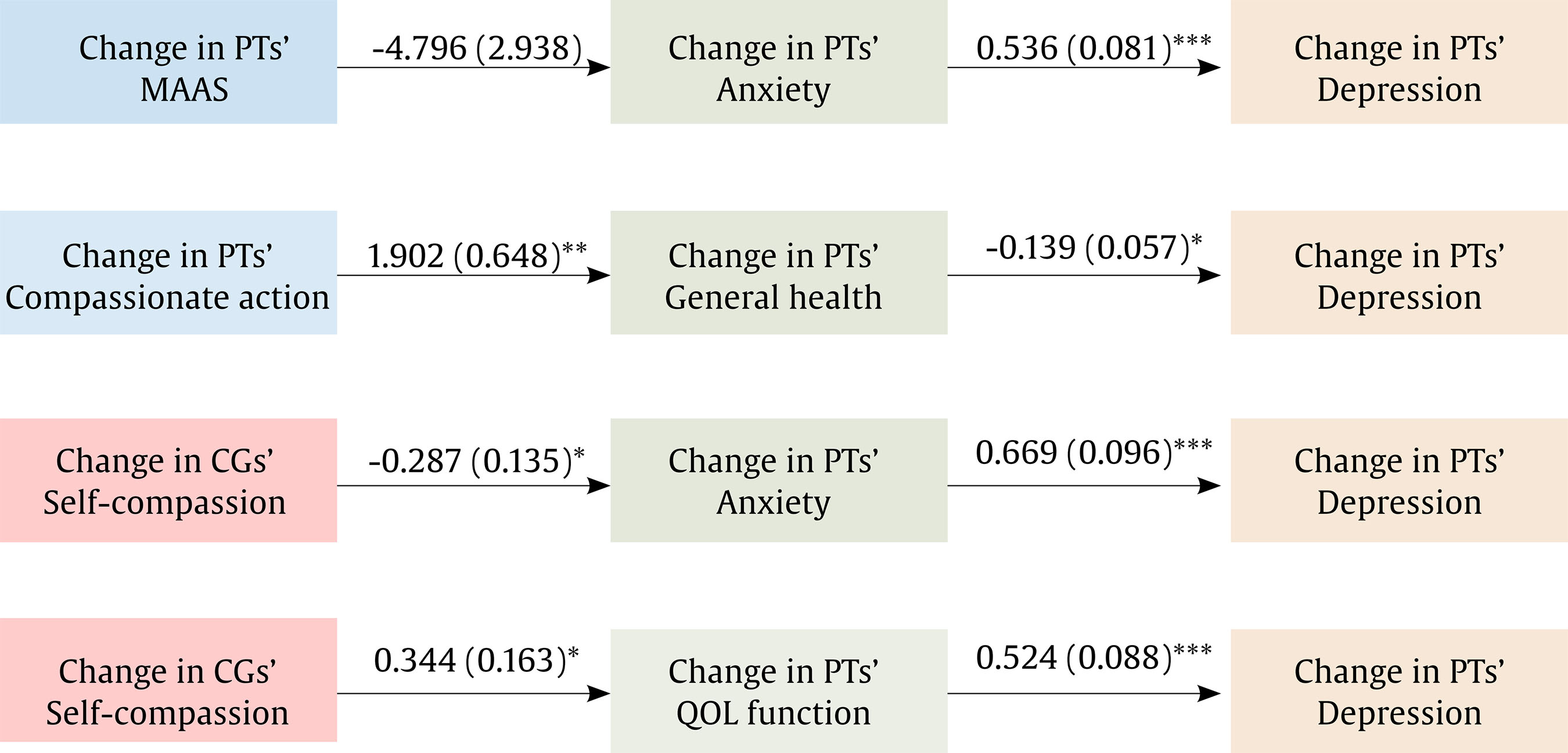 *p < .05, **p < .01, ***p < .001. The effect of the patients’ compassionate action on their depressive symptoms was mediated through change in general health (effect = -0.265, Boot SE = 0.156, 95% Boot CI [-0.598, -0.002]). Change in the patients’ compassionate action was positively related to their general health, which in turn was related to fewer depressive symptoms. Furthermore, change in the patients’ QOL function significantly mediated the effect of the caregivers’ self-compassion on the patients’ depressive symptom (effect = -0.180, Boot SE = 0.088, 95% Boot CI [-0.389, -0.047]). The results revealed that change in the caregivers’ self-compassion positively affected patients’ QOL function, in turn, reducing patients’ depressive symptom. Sensitivity Analysis and Power Calculation To validate the robustness of our findings, we conducted a sensitivity analysis comparing results derived from the original data to those obtained through multiple imputation. This analysis, which examined between-group differences and within-group differences over time in BDI scores, consistently supported our primary findings. Additionally, a power analysis was conducted to ensure the study was adequately powered to detect differences in BDI scores over time using a GEE model. Based on a meta-analysis by Cillessen et al. (2019) which reported small to medium effect sizes for mindfulness-based interventions in cancer populations, we calculated that a total sample size of 56 participants (27 in the study group and 29 in the control group) would provide a power of 0.95 at a significance level of .05. This 14-month study found that a dyadic mindful compassion BMS program is more likely to reduce lung cancer patients’ depression than a patient-only program. The study suggested that a patient-caregiver dyadic mindfulness compassion BMS program might be a better approach for lung cancer patients. Similarly, the previous study (Schellekens et al., 2017) also found that 8-week MBSR combined with cancer-supportive care reduced lung cancer patients’ depression. This previous study and our present study both found that there were no changes in caregivers’ depression after the mindfulness program. The findings on caregivers might suggest that the current dyadic mindfulness compassion BMS program has a limited effect on improving caregivers’ depression. Previous studies have indicated that lung cancer patients with higher levels of depression benefit more from dyadic MBSR interventions (Schellekens et al., 2017; van den Hurk et al., 2015). However, our study’s moderator analyses revealed that the effect of the patient-caregiver dyadic intervention on depressive symptoms was more pronounced in younger patients and those with greater QOL symptom distress at baseline. These findings suggest that younger lung cancer patients or those with more severe symptom distress might particularly benefit from having their family caregivers participate in a mindfulness compassion program. Bade et al. (2015) found that a dyadic psychosocial program improved advanced lung cancer patients’ self-efficacy in managing cancer symptoms, depression, and anxiety. Based on our study’s findings, younger lung cancer patients or those with more severe symptoms might gain more self-efficacy in managing their symptom distress through a dyadic mindfulness compassion program, which could subsequently alleviate their depressive symptoms. Mediator analysis found that increases in patients’ mindfulness awareness over 14 months reduced their anxiety, which in turn decreased depressive symptoms. These results suggest that mindfulness awareness can mitigate lung cancer patients’ anxious responses to the threat posed by their disease. This finding supported the mindfulness-to-meaning theory suggesting potential mechanisms by which mindfulness practices enhance positive emotional regulation, subsequently improving depression (Garland et al., 2015; Garland et al., 2017). Garland et al. (2017) demonstrated that present-moment mindfulness awareness reduces people’s focus on threats, thereby decreasing hypervigilance and anxious arousal from threats. Additionally, decentering from threats enhances metacognitive awareness, leading to a positive reappraisal of stress, active coping, savoring daily life, and experiencing positive emotions. Shapiro et al. (2006) noted that present-moment mindfulness fosters cognitive flexibility when confronting life adversities. Cheung and Ng (2019) found that focusing on nonjudgmental awareness and attention in the present moment can reduce depression by enhancing awareness and acceptance of negative emotions and encouraging the use of positive emotional regulation strategies among adults. Based on these studies and the mindfulness-to-meaning theory, increased mindfulness awareness over 14 months may decrease lung cancer patients’ anxiety responses to cancer threats and foster more positive views of the stress associated with living with cancer. Consequently, depressive-related symptoms such as low mood and rumination could be reduced. This study found that changes in patients’ compassionate actions over 14 months were positively related to their general health, which in turn was associated with fewer depressive symptoms. Compassionate actions in lung cancer patients measured their motivation to alleviate and prevent distress. The finding supported Gilbert et al.’s (2017) emotional regulation model, suggesting that cultivating self-compassion mitigates automatic threat responses, and enhances their recognition, acceptance, and management of life’s adversities (Gilbert et al., 2017). Previous studies have found associations between cancer patients’ mindfulness awareness and self-compassion with depressive symptoms (van der Donk et al., 2020) and quality of life (Garcia et al., 2021). These results suggest that mindfulness and self-compassion can serve as personal resources for cancer patients, helping them cope with life’s adversities. In this study, the impact of compassionate actions on lung cancer patients’ general health suggests that they likely utilized their personal resources to take action and improve their health, which in turn reduced their depressive symptoms. This study found that an increase in caregivers’ self-compassion over 14 months reduced patients’ anxiety and improved their quality of life, which in turn reduced patients’ depressive symptoms. In this study, caregivers’ self-compassion was measured by their ability to emotionally connect with and empathize with suffering, and to take contentment-focused actions to relieve that suffering. Finlay-Jones (2017) demonstrated that self-compassion facilitates an individual’s capacity for kindness towards themselves and aids in positively reappraising and coping with stress. Schellekens et al. (2017) found that lung cancer patients’ spouses’ self-compassion could buffer their partners’ psychological distress. The findings of our study suggest that enhancing caregivers’ self-compassion and positive emotional regulation can reduce patients’ depressive symptoms by alleviating patients’ emotional distress (anxiety) and improving their overall health (quality of life). In conclusion, mindfulness compassion provided dyadically or individually, can be appropriately tailored to patients’ age and levels of physical distress. The impacts of patients’ mindfulness awareness and compassionate actions on their anxiety levels and general health could explain the reduction in depression. Additionally, caregivers’ positive emotional regulation through self-compassion can reduce patients’ depressive symptoms by alleviating their anxiety and improving their quality of life. Limitations and Future Research Our sample consisted primarily of advanced lung cancer patients receiving targeted therapy. Generalizing findings to lung cancer patients with early-stage may be limited. Additionally, the study lacked an appropriate comparison condition. Both groups received similar interventions, with the dyadic group both patients and caregivers participating together, while the control group consisted of patients only, and caregivers received information at home. This design makes it challenging to assess comparative effectiveness. Nevertheless, this study could demonstrate who could benefit more from a dyadic depression program. Furthermore, due to the patient-caregiver dyadic approach and the physical burdens in advanced lung cancer patients, maintaining participant retention over time is likely to be a challenge. For the implications of this study, integrating mindfulness and compassion with Body-Mind-Spirit (BMS) could be applied in clinical practice to address the needs of advanced lung cancer patients and their caregivers. This comprehensive intervention includes education, symptom management, holistic BMS empowerment skills, mindfulness, and compassion-focused techniques. Clinical professionals can utilize this intervention to manage the significant physical symptom burden associated with advanced lung cancer, reduce the impact of anxiety and depression on physical symptoms, empower individuals through BMS strength activities and compassionate actions for themselves and their loved ones, and enhance their ability to cope with stress positively. The intervention starts with a 15-minute qi-gong exercise, which can help patients feel more energetic and engage in mindfulness, compassion-breathing, and meditation. Providing a mobile app for practicing qi-gong, mindfulness, and compassion skills at home, along with a group LINE app for real-time consultations and mutual support, can enhance group learning and support. While some caregivers are not able to participate in a dyadic program, those caring for younger patients or experiencing high levels of symptom distress are encouraged to join. Additionally, future development and testing of an online dyadic program could benefit advanced lung cancer patients and caregivers who are unable to attend in-person sessions. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Hsiao, F. H., Ho, C. C., Yu, C. J., Shih, J. Y., Lin, Z. Z., Huang, F. Y., Chen, Y. T., Hsieh, C. C. (2025). The mindful compassion program integrated with body-mind-spirit empowerment for reducing depression in lung cancer patient-caregiver dyads. Psychosocial Intervention, 34(1), 1-9. https://doi.org/10.5093/pi2025a1 Funding This study was supported by the Ministry of Science and Technology under Grant (NSC 108-2314-B-002-215-MY3). |
Cite this article as: Hsiao, F., Ho, C., Yu, C., Shih, J., Lin, Z., Huang, F., Chen, Y., & Hsieh, C. (2025). The Mindful Compassion Program Integrated with Body-Mind-Spirit Empowerment for Reducing Depression in Lung Cancer Patient-Caregiver Dyads. Psychosocial Intervention, 34(1), 1 - 9. https://doi.org/10.5093/pi2025a1
Correspondence: cchsieh1116@gmail.com (C-C Hsieh).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






