Psychosocial Profiles of Adults with ADHD: A Comparative Study of Prison and Outpatient Psychiatric Samples
[Perfiles psicosociales de adultos con TDAH: un estudio comparativo con muestras reclusa y cl├şnica]
Trinidad García1, Celestino Rodríguez1, Javier Rodríguez1, Asunción Fernández-Suárez1, Vanesa Richarte2, and J. Antoni Ramos-Quiroga2
1University of Oviedo, Spain; 2Hospital Universitari Vall dÔÇÖHebron, Barcelona, Spain
https://doi.org/10.5093/ejpalc2018a14
Received 12 April 2018, Accepted 5 November 2018
Abstract
This study aimed to describe and compare the educational, social, and family profiles of adults with and without ADHD from two different settings: a prison and an outpatient psychiatric setting. A total of 542 participants, aged between 17 and 69 years, took part in the study. The participants consisted of four groups: a prison sample with ADHD (n = 69) and without ADHD (n = 183), and an outpatient psychiatric sample with ADHD (n = 218) and without ADHD (n = 72). The results showed that, firstly, there were some statistically significant differences between the groups in academic history, social and family situation, and the adoption of risk behaviors during adolescence and early adulthood. Secondly, some of these differences were related to diagnosis (ADHD versus non-ADHD) while others were related to the sample being examined (prison versus psychiatric). The findings from the study showed the presence of significant implications in social, family, educational, and employment achievements both for adults with ADHD (both prison and psychiatric samples) and for adults without ADHD.
Resumen
Este estudio tiene como objetivo describir y comparar los perfiles educativos, sociales y familiares de un grupo de adultos con y sin TDAH de dos muestras diferentes: una de carcelarios y una población clínica. Formaron parte del estudio 542 participantes, con edades comprendidas entre los 17 y 69 años. La muestra se dividió en cuatro grupos, un grupo de carcelarios con TDAH (n = 69) y sin TDAH (n = 183) y un grupo clínico con TDAH (n = 218) y sin TDAH (n = 72). Los resultados apoyan la hipótesis inicial, que establece que, primero, hay diferencias estadísticamente significativas entre los grupos en cuanto a historial académico, situación social y familiar y la adopción de conductas de riesgo durante la adolescencia y la adultez temprana; en segundo lugar, algunas de las diferencias se relacionarán con el diagnóstico de TDAH, mientras que otras estarán más vinculadas a la población examinada. Los hallazgos del estudio mostraron la presencia de consecuencias significativas para los contextos sociales, familiares, educativos y laborales tanto en poblaciones adultas con TDAH (pacientes en carcelarios y clínicos) como aquellas sin TDAH.
Keywords
ADHD, Adults, Prison, Outpatient psychiatric patients, Legal consequencesPalabras clave
TDAH, Adultos, Carcelarios, Muestra cl├şnica, Consecuencias legalesCite this article as: García, T., Rodríguez, C., Rodríguez, J., Fernández-Suárez, A., Richarte, V., & Ramos-Quiroga, J. A. (2018). Psychosocial Profiles of Adults with ADHD: A Comparative Study of Prison and Outpatient Psychiatric Samples. The European Journal of Psychology Applied to Legal Context, 11(1), 41 - 49. https://doi.org/10.5093/ejpalc2018a14
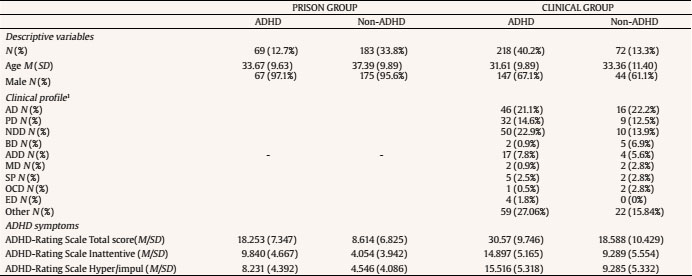
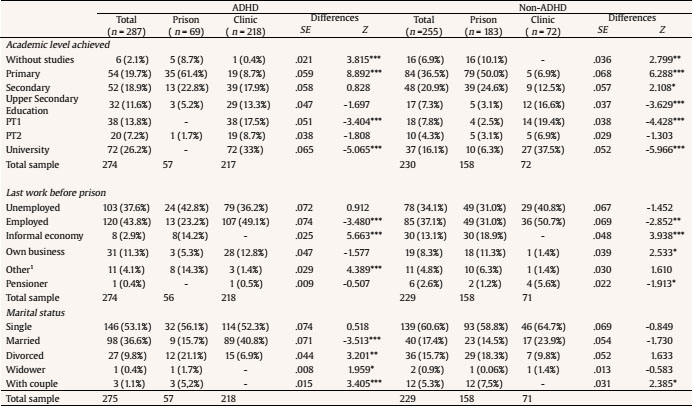
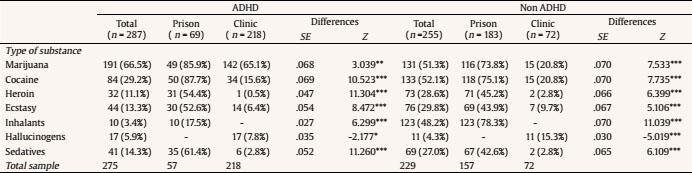
rodriguezcelestino@uniovi.es Correspondence: rodriguezcelestino@uniovi.es (C. Rodríguez).Attention deficit hyperactivity disorder (ADHD) is a neuro-developmental disorder characterized by inattention, hyperactivity, and impulsivity (Dupaul, Power, Anastopoulos, & Reid, 1998). While hyperactivity tends to decline with age, symptoms of inattention are more likely to persist into adulthood. The rate of ADHD persistence into adulthood is 65%, including a partial remission state (Biederman, Mick, & Faraone, 2000; Faraone, Biederman, & Mick, 2006). Adult ADHD is prevalent (observed in approximately 4.4% of adult populations) (Faraone & Biederman, 2005; Kessler et al., 2006), and causes substantial functional impairment (Barkley, Fischer, Smallish, & Fletcher, 2002; Murphy & Barkley, 1996). Adult ADHD is associated with psychiatric disorders such as mood disorder, anxiety disorder, and substance abuse, as well as antisocial and illegal behaviors (Barkley, Fischer, Smallish, & Fletcher, 2004; Biederman et al., 2010). Adult ADHD causes long-term health and economic burdens, including costs related to medical health, education, social services, and the criminal justice system (Biederman et al., 2006; Chorozoglou et al., 2015). Despite the consequences and clinical implications of adult ADHD, little clinical attention is paid to this population (Asherson et al., 2012). In fact, fewer than 20% of adults with ADHD are diagnosed or treated, and the majority of adult ADHD patients remain untreated or in states of partial remission for years (Epstein & Johnson, 2001; Estrada, Rodríguez, & Solano, 2012; Fayyad et al., 2007). If adult ADHD were to be successfully diagnosed and treated, then these individuals’ progression to further functional impairment could be prevented (Ramos-Quiroga et al., 2012). Recent studies have continued to demonstrate significantly higher functional impairment in adults with ADHD compared to controls (Brown, Flood, Sarocco, Atkins, & Khachatryan; Suhr, Cook, & Morgan, 2017; Szuromi, Bitter, & Czobor, 2013). Further, the severity of ADHD symptoms has been found to be significantly correlated with the degree of impairment in quality of life (Gjervan, Torgersen, Rasmussen, & Nordahl, 2014). Previous research suggests that ADHD symptoms during childhood and adolescence may affect academic, social, and family functioning, and may also be related to the adoption of high-risk behaviors, such as drug consumption and legal problems. Unsurprisingly, high rates of neurodevelopmental disorders and difficulties, including ADHD, have previously been reported for incarcerated male, adult offenders (Ali, Ghosh, Strydom, & Hassiotis, 2016; McCarthy et al., 2016). Young et al. (2011) found that in an English sample 24% of the prison population had a childhood history of ADHD. In a Spanish prison population, based on information obtained from retrospective questionnaires, Rodriguez et al. (2015) found a ADHD prevalence rate of 25%. Despite these findings, research into the psychosocial profiles of incarcerated offenders with ADHD is still lacking. In a recent study McCarthy et al. (2016) examined a sample of 87 prisoners, finding differences in the psychosocial profiles of those who had a neurodevelopmental disorder (including ADHD, autism spectrum disorder – ASD –, and intellectual disability – ID), and those without any neurodevelopmental disorders. People in the neurodevelopmental disorder group were younger than those without any disorders. They were also more likely to be single, and a higher proportion of them had been unemployed and homeless prior to imprisonment. The group with neurodevelopmental disorder also had lower educational qualifications, which may be related to their higher rates of unemployment. However, the fact that over 80% of them had a previous history of conviction or imprisonment may be the most outstanding finding in this context. Results from this study were similar to those found by Ginsberg, Hirvikoski, and Lindefors (2010) and by Hassiotis et al. (2011), among others, which suggests that, if they are not tackled in time, ADHD symptoms have the potential to foster social disadvantage and exclusion, limit employment opportunities and lead to the adoption of risky behaviors, which may end up being the perfect scenario for further legal problems. However, social and academic difficulties are not exclusive to ADHD or the prison population. There is a good deal of evidence for the relationship between mental illness and impaired functioning in various everyday life contexts (Armijo, 2017; Breslau et al., 2011; Hammar & Årdal, 2009; Liebke et al., 2017; Llorca-Mestre, Malonda-Vidal, & Samper-García, 2017). It is no coincidence that, despite the changes made in recent years in some of the criteria for mental disorders, the DSM-5 (American Psychiatric Association, 2013) establishes that clinically significant impairment in social, academic, or work functioning must be present as a fundamental criterion for most of the mental illnesses. Very common mental disorders, such as anxiety, depression, and some personality disorders, are associated with significant disability and poorer quality of life, as well as impaired social and family functioning (Armijo, 2017; Breslau et al., 2011; Hammar & Årdal, 2009; Liebke et al., 2017). Strong associations between premarital mental disorders and separation and divorce have been reported, with phobias, severe depression, and alcohol abuse being the most commonly associated conditions (Breslau et al., 2011; Sánchez, Sobral, & Seijo, 2017). In the case of depression, it is common that patients with severe depressive symptoms have significant difficulties performing at an acceptable level at work, in some cases finding it impossible. Many also have problems fully participating in social and/or family life (Hammar & Årdal, 2009). Several studies suggest that adolescents with mental health problems perform less well in school and attain lower qualifications than other young people without these conditions (Fletcher, 2010; Hunt, Eisenberg, & Kilbourne, 2010; McLeod, Uemura, & Rohrman, 2012). However, recent studies suggest that behavioral problems, such as ADHD, disruptive behavior disorders, and oppositional/defiant behaviors, play the most important role in this context (Duncan et al., 2007; McLeod et al., 2012; Sayal, Washbrook, & Propper, 2015). McLeod et al. (2012) reported a significant relationship between problems of attention, delinquency, and diminished academic achievement, finding no association with depression. The role of anxiety has been substantially reported. However, this questions the influence of internalizing and externalizing disorders on academic performance (Mazzone et al., 2007). What seems almost indisputable is the relationship between ADHD symptoms and social, academic, and family performance, and risky behavior. There is no evidence however, about whether the poor functioning linked to ADHD is the same in mental health and prison settings. This research is important, since there is a need to improve recognition and understanding of neurodevelopmental and mental disorders within both the criminal justice system and society in general. This will help improve clinical interventions as well as prison healthcare and reintegration programs (Alfaro-Beracoechea, Puente, da Costa, Ruvalcaba, & Páez, 2018). Aims This study aimed to describe and compare the educational, social, and family profile of adults with and without ADHD from two different settings: a prison population and an outpatient psychiatric setting. In particular, this study sought to determine whether there are differences in the psychosocial profile between adults with ADHD from two different settings (psychiatric and prison), and with controls (non-ADHD groups) from the same two settings. The psychosocial variables of interest were: a) academic history (educational failing, repeating school years, academic level achieved), social situation (last work situation before prison, marital status), and family context (family history of substance abuse and mental health problems); and b) adoption of risky behavior during adolescence and adulthood, mainly drug consumption and (for participants from the outpatient psychiatric setting only) having a criminal record. Participants The sample of 542 participants were aged between 18 and 69 years old (M = 34.04, SD = 10.35 years). Of the total sample, 433 (80%) were men and 109 (20%) were women. Participants were divided into four groups based on two criteria: ADHD diagnosis (ADHD/non-ADHD) and type of setting (prison/psychiatric outpatient). In order to verify the diagnosis of ADHD and to assign the participants to each group, the ADHD-IV scale (Dupaul et al., 1998) was administered. The main characteristics of the four groups are shown in Table 1. The differences in mean ages between the four groups were statistically significant (F3, 532 = 10.949, p < .001, η2 = .058) and post hoc analyses revealed significant group differences with Bonferroni correction (p < 05/6 = .008) between the control groups (non-ADHD) of both the psychiatric and prison samples (p < .008), and between the ADHD group of the psychiatric sample and the control group of prisoners (p < .008) (Table 1). There were also statistically significant differences in gender distribution, with a higher number of men in all of the groups. Differences in the proportion of men and women were statistically significant for the ADHD prison group (c2 = 61.232, p < .001), the non-ADHD prison group (c2 = 152.399, p < .001), and the ADHD psychiatric group (c2 = 24.495, p < .001); while these differences were not significant in the non-ADHD psychiatric group (p = .059). Participants in the groups with ADHD had higher total scores on the ADHD-Rating Scale IV (Dupaul et al., 1998) than the prison group without ADHD. The analysis of homogeneity of variance (Levene test) showed that the error variance of the dependent variable (ADHD score) is not equal between the groups, F(3, 521) = 12.778, p < .001. The group with the highest scores on the scale was the ADHD group in the psychiatric setting. These differences were statistically significant, F(3, 525) = 197,913, p < .001, η2 = .533. Post hoc multiple comparisons with T3 Dunnett revealed significant group differences between the ADHD psychiatric group and the other three groups (p < .001), and between the prison ADHD group and the control group of prisoners (p < .001). Given the difference in mean ages between the groups, this analysis was repeated with age as a covariate. Age did not have a statistically significant effect (p = .763) on ADHD symptoms. The group from the psychiatric outpatients setting (both with and without ADHD) scored significantly higher on the ADHD scale than the group from the prison setting. This finding may be due to the comorbidity of some ADHD symptoms with symptoms of other mental disorders. This aspect could also explain the absence of differences between the ADHD prison group and the non-ADHD outpatient group. Measures - For participants in the prison setting information on their family, academic, and social history was obtained via the Penitentiary History Sheet (Estrada et al., 2012). For the participants in the psychiatric outpatient setting, information on the same variables was obtained by means of each patient’s clinical history as obtained by administration of the Conners Adult ADHD Diagnostic Interview for DSM-IV (CAADID-part I) (Epstein & Johnson, 2001). The CAADID is a semi-structured interview that collects information related to a patient’s development, from childhood and adolescence to adulthood. It comprises questions related to school, family, and psychiatric history, social relationships and employment history, among others. - The ADHD Rating Scale-IV (Dupaul et al., 1998) was used to verify the diagnosis of ADHD and to assign the participants to the different groups. It is a self-report questionnaire consisting of 18 items referring to the symptoms of ADHD, according to DSM-IV. Each item is scored on a 0 to 3 scale: 0 = none (never or rarely), 1 = mild (sometimes), 2 = moderate (often), 3 = severe (very often). High scores are indicative of behavioral problems related to ADHD. This scale was recently validated for the adult Spanish population and demonstrates good psychometric properties, with high discriminative capacity in the differentiation of ADHD and its presentations (Ramos-Quiroga et al., 2012) (Table 1). Procedure Approval to conduct this project was obtained from the Research Ethics Committee of the University of Oviedo. The prison setting was a penitentiary center in northern Spain. The prisoners were part of the ordinary program (second grade of the Spanish Prison System). Participants in the psychiatric outpatient setting came from the clinical specialized services of a psychiatric hospital unit in the west of Spain. The psychiatric sample was accessed and selected from patients who came to the hospital requesting psychiatric assessment and treatment. All participants were volunteers who provided informed consent to take part in the study. Confidentiality of participants’ information was guaranteed (Williams, 2008). None of the participants in the prison group had a formal diagnosis of ADHD. The prison setting ADHD group was obtained by administering the ASRS scale (Ramos-Quiroga, Daigre et al., 2009). This scale establishes a cut-off point of 12 as a criterion for ADHD symptomatology in adults. Those participants from the prison setting who scored over 12 points were included in the ADHD group. Also, diagnosis of ADHD was verified with the ADHD Rating Scale-IV. Only if the prisoners met the criteria of both scales were they included in the prison setting ADHD group. Participants from the psychiatric outpatient setting with ADHD and other clinical disorders had previously been diagnosed by specialized services. However, in order to verify the diagnosis of ADHD and to assign participants to each group, the ADHD Rating Scale-IV (Dupaul et al., 1998) was also administered to these participants. Data Analysis The information about participants’ academic history, social, and family records was organized in different groups of variables. (1) Academic history and social records: academic failure (failed school years and course repetitions), academic level achieved (from “without studies” to “University”), current or last work performed before prison (“unemployed, employed, informal economy, own business, pensioner, or other”), and marital status (“single, married, divorced, widower, with couple”). (2) Family records: family substance abuse and history of mental health problems. Both questions had two response options (presence = yes, or absence = no) . The type of substance or mental illness was not included in the analyses. (3) Participants’ risk behaviors: substance abuse (frequency by type of substance; “marijuana, cocaine, to sedatives, heroin, ecstasy, inhalants, hallucinogens, and other”), and criminal record (having been tried on at least one occasion - presence = yes, or absence = no). This last variable was only reported in the case of the psychiatric sample. In keeping with the main objectives of the study, data were analyzed as follows. For differences in academic, social, family, and criminal records between pairs of groups (first comparison: ADHD groups from clinical and prison populations; second comparison: non-ADHD groups from clinical and prison population), given the (qualitative) nature of the variables and the study objectives, frequencies and percentages were used. The χ2 test - or Fisher’s exact test - for categorical variables were used. The Z statistic was used to analyze the differences in percentages. The level of statistical significance was set at p < .05. Academic and Social Factors One result which stands out as statistically significant in participants’ academic profiles is the difference in percentages of subjects with ADHD who had failed school years. In the prison group the percentage was 87.5% compared to the clinical group’s 72.4% (SE = .064, Z = 2.333, p = .019). Results for the non-ADHD groups were different, with a 76.9% of prisoners having experienced academic failure in comparison to 83.3% in the clinical population. These differences were not statistically significant (p = .302). The differences in history of repeating school year were not statistically significant. Within the ADHD group, 75% of prisoners had repeated a year, compared to 65.1% of the clinical population (p = .161). In the non-ADHD groups, 65.3% of the prison group had repeated at least one school year, in contrast to 61.6% of the clinical sample (p = .605). Differences in the participants’ educational level achieved are sharper (Table 2). In the prison population, both with and without ADHD, there is a statistically significantly higher percentage of participants with no schooling, as well as a higher percentage of participants who had only completed primary or secondary education (p < .001). The percentage of prisoners completing further or higher education is statistically significantly lower than the clinical sample (p < .001). This difference is present in high school, university, and professional training. In addition, none of the inmates with ADHD had studied at university, and only 6.3% in the non-ADHD group had achieved access to this stage of education. There were no statistically significant differences in the social context variables in relation to the last work performed or in the rates of unemployment (in the case of prisoners, this refers to their situation before imprisonment). However, there were differences in the source of income in the group who were employed, with a higher proportion of prisoners (with and without ADHD) earning money from the informal economy and from subsidies or other social assistance in comparison to the clinical sample with and without ADHD (Table 2). Lastly, some differences in marital status between the ADHD and non-ADHD groups were found. In the ADHD group, a statistically significantly higher percentage of prisoners were divorced (p < .01). The percentage of married people in this group was also significantly lower. No statistically significant differences between the prison and clinical population were found in the non-ADHD group (Table 2). Family Factors In the ADHD group (n = 273), a total of 136 participants (49.8%) reported a family history of substance abuse, while in the non-ADHD group, with a total of 225 subjects, this percentage was 52.4%. The difference was not statistically significant (p = .559). A higher percentage of participants whose families had a history of substance abuse was found in the prison population with ADHD. Of the total sample of 57 inmates with ADHD, 41 (71.9%) reported substance use by their family, in comparison to 95 participants (43.9%) – from a total of 216 – in the clinical sample. These differences were statistically significant (SE = .744, Z = 3.753, p ≤ .001). In the non-ADHD group, 27 participants from the prison sample reported family problems with drugs (47.3%, n = 57), in contrast to 67 from the clinical sample (30.7%, n = 218). These differences were statistically significant (SE = .072, Z = 3.835, p ≤ .001). Significant differences were also found in the variable: history of family mental health problems. In the ADHD groups, a total of 94 participants (34.18%) answered yes to this question. In the prison group, comprising 158 people, a total of 96 (60.7%) answered yes to this question in comparison to 22 participants (32.8%) from a total of 57 in the clinical group (ES = .705, Z = 2.357, p ≤ .001). Furthermore, in the non-ADHD group, the proportion of family mental health problems was 41.9% (107 from 225 participants). The percentage of mental health problems in the family was higher in the clinical sample (44 participants from a sample of 67 reported these problems, 65.6%) compared to the prison sample, where 63 participants (39.8%) from a population of 158 also reported these problems (SE = .072, Z = -3.543, p ≤ .001). High Risk Behaviors Analysis of risk behavior habits revealed that there were statistically significant differences in substance abuse for all of the types of drugs analyzed, with higher percentages in prisoners in both ADHD and non-ADHD groups (Table 3). Finally, looking at criminal records in the psychiatric outpatients sample only, 20 participants in the ADHD group from a total 218 (9.2%) reported having a criminal record, while 21 participants from 72 in the non-ADHD group (29.2%) answered yes to this question. These differences were statistically significant (SE = .047, Z = -4.221, p ≤ .001). ADHD is a chronic disorder with onset during childhood, the symptoms of which may persist over time. It is important to note that an individual’s personality is mostly created during that period, and it is considered to be a relatively stable cognitive, emotional, and behavioral pattern. The stability and chronic nature of ADHD suggest at least a theoretical association between this disorder and personality development and consolidation, both adaptive and maladaptive (Martínez-Ortega et al., 2010). Personality, along with social, work, and family functioning patterns, is also affected by other clinical conditions, such as depression, anxiety, and some major clinical disorders (Armijo, 2017; Breslau et al., 2011; Hammar & Årdal, 2009; Liebke et al., 2017). The consequences of ADHD, particularly in adults, have not been studied in depth, hence the limitations of previous research on this topic. The present study attempts to take a retrospective perspective to examine academic history, social, and family situations, and risky behavior in a sample of adults with and without ADHD, looking at two different samples: a prison and a clinical population. Our results support our initial hypothesis, which states that there will be some statistically significant differences between groups in terms of academic history, social, and family situation, and the adoption of risky behaviors during adolescence and early adulthood; some of the differences will be related to the diagnosis of ADHD whereas others will be linked to the population being examined. Academic and Social Profile The results indicated a general tendency to academic failure in all sub-samples (with and without ADHD, clinical vs. prison population). The high percentage of failures and repeated school years in all the groups is notable, over 70% and 60% respectively in the general sample. It is also worth noting that prisoners with ADHD had the highest proportion of failed school years, followed by those in the clinical sample without ADHD, with percentages of failure over 80% in both sub-samples. The results also showed that there is a higher proportion of uneducated people (or those with only the most basic qualifications) in the sample of prisoners than in the clinical samples. It is worth noting that none of the participants with ADHD in the prison group had university level education, in comparison to 6.5% of prisoners without ADHD who did. This is in line with previous studies which found a relationship between ADHD and other clinical disorders, and academic failure (Armijo, 2017; Breslau et al., 2011; Hammar & Årdal, 2009; Hunt et al., 2010; Liebke et al., 2017; McCarthy et al., 2016; McLeod et al., 2012). However, it is the prison population with ADHD which demonstrated the most significant impairment in this context. A study conducted by (Ginsberg et al., 2010) may contribute to understand this finding. The authors reported poorer executive functions in a sample of inmates with ADHD, also when controlling for estimated IQ, compared with psychiatric outpatients with ADHD and controls. Considering the implications of executive functions for the regulation of the behavior (Férriz, Sobral, & Gómez-Fraguela, 2018; García, González-Castro, Areces, Cueli, & Rodríguez, 2014), it stands to reason that there would be more significant impairments in prisoners with ADHD. It is interesting since it is in this group where we found the highest proportion of divorcees, higher than the divorce rates reported by the ADHD group in the clinical sample. Finally, some differences regarding subjects’ work situations before prison were found. A proportion of prisoners – regardless of the presence of ADHD symptoms – were in receipt of subsidies and earned money via the informal economy than in the clinical sample. This finding may be related to findings about educational levels and also the fact of going to prison, since the “informal economy” label covers a multitude of ways of earning money. All these findings support the relationship between ADHD symptoms and significant impairment to patient quality of life (Gjervan et al., 2014), a relationship that is even more important in the case of people in prison (Ginsberg et al., 2010; González, Vélez-Pastrana, Ruiz Varcárcel, Levin, & Albizu-García, 2015; Hennessey, Stein, Rosengard, Rose, & Clarke, 2010). Family History: Substance Abuse and Mental Health Problems Results indicated that there were no differences related to the diagnosis of ADHD and family history of substance abuse, but rather that it was related to the condition of being in prison. A higher frequency of drug abuse in families (i.e., parents, siblings, and partners) was found in this group in comparison to those in the clinical sample. This was expected considering the implications of substance abuse in families for both adults and children (Lander, Howsare, & Byrne, 2013). As these authors state, the use and abuse of drugs affects the whole family system, leading to emotional and behavioral patterns, which frequently result in poor outcomes for children and adults. In addition, the impact will vary depending on an individual’s gender and role in the family. Again, it is important to point out that frequency of family drug abuse was reported by inmates with ADHD. If an adolescent child is identified as having trouble with drugs, this will affect the family differently than if a parent has the problem. In our study, family histories of substance abuse are primarily linked to parents (Ibabe, Arnoso, & Elgorriaga, 2014). Consequences of adult drug abuse for children include unmet developmental needs, impaired attachment, economic hardship, legal problems, emotional distress, and even violence, as well as an increased risk of developing a substance use disorder (SUD) themselves (Lander et al., 2013; Martínez-Catena, & Redondo, 2017; Zimi & Juki, 2012). On the other hand, our results indicated that the likelihood of finding a history of mental health problems is higher in the clinical group, whether they have ADHD or not, in comparison to the prison group. It is important to note at this point that we are talking about many different clinical conditions in the present study, including severe mental illness such as bipolar disorder, or severe depression. Genetics, environmental exposure and their interactions – all have an important role in the development of these conditions, which are even more important in the case of the most severe disorders (Sanz-García, Dueñas, & Muro, 2010; Uher, 2014), hence the expected relationship found in our study. High Risk Behaviors Results from this study support the hypothesis that in the prison sample, both with and without ADHD, the condition of being in prison is associated with increased and aggravated the adoption of risk behaviors compared to the clinical group, mainly drug consumption in adolescence and adulthood, among others. Various studies show the existence of drug abuse in individuals with ADHD. Specifically, Sanz-García et al. (2010) state that prisoners with ADHD start using drugs earlier, in higher quantities, and with more frequent use of psychotropic drugs. Dual psychopathology (ADHD plus substance use disorder) occurs in more than half of adults with ADHD (Biederman, Wilens, Mick, Faraone, & Spencer, 1998; Sullivan & Levin, 2001). Other studies also support our results (Verdejo-García, Bechara, Recknor, & Pérez-García, 2007; Wilens, Biederman, & Mick, 1998). Verdejo-García et al. (2007) found that in a sample of adult patients who came to consultations as a result of ADHD, between 17 and 45% showed alcohol abuse, and between 9 and 30% also abused of other drugs. They also found that these patients had a higher risk of relapse after detox. More recently, Young et al. (2017) reported significantly higher levels of substance abuse among prisoners with ADHD (in comparison to those without ADHD symptoms), especially methadone and amphetamine use. Other studies suggest that some functional and structural alterations in the brains of ADHD subjects could explain this association (Andreu, Letosa, López, & Mínguez, 2015). There are structural and functional alterations in reward circuits in this population (Alcázar-Córcoles, Verdejo-García, Bouso-Saiz, & Bezos-Saldaña, 2010). Like Ramos-Quiroga, Sáez-Francàs et al. (2009), we might say that these alterations, like the regulation of impulsivity and executive function, are closely related to the symptoms of ADHD and that they could also be related to the association between this disorder and substance abuse. Finally, a higher proportion of criminal records was found in the group without ADHD in comparison to those who met the criteria for the disorder. Only 9% of the clinical sample with ADHD reported having legal problems, versus 29% in the clinical group without ADHD. While a higher percentage of criminal records may be expected in the comorbid group (ADHD plus other clinical condition), results from our study are in line with previous research, finding an association between mental illness and criminal behavior (Cuellar, Snowden, & Ewing, 2007). These authors examined a random sample of 6,624 people who used the mental health system in Los Angeles County between July 1993 and June 2001, and found that almost a quarter of those with serious mental illness were arrested at least once in a ten-year period; more than one-third of those were arrested for violent crimes, with drug crimes the second most common category. Interestingly, they also found that the seriousness of the offense varied according to the diagnosis; for instance, those diagnosed with schizophrenia or psychosis were more likely to be arrested for violent crimes, whereas those with other disorders, such as depression, were arrested for drug-related crimes. The composition of the sample itself, in terms of clinical conditions present in the groups with and without ADHD in our study, and even the severity of these conditions, may explain the differences found between the groups in this variable. Implications of Findings ADHD is a very common clinical condition in children, but also, importantly, in adults. However, current assessment tools and intervention programs seem to be more aimed at overcoming problems associated with the disorder as early as possible, which is tremendously important. Sometimes, however, we fall into the error of not paying attention to the part of the population that, although adult, may be suffering from the consequences of ADHD. Our study aimed to examine this specific population in two different contexts (prison, and the mental health system), in order to look more deeply into these consequences. Findings showed the presence of significant consequences in social, family, educational, and work contexts for both populations with ADHD in comparison to those without, although some sort of differential profiles were found between them. The group of prisoners with ADHD is especially vulnerable in this sense, exhibiting the highest levels of disorganization and impairment in their daily lives. This suggests the need to consider these particular issues when designing treatment programs for prison inmates with ADHD, as well as more fluid communication and collaboration between prison and mental health services. The clinical sample cannot be overlooked, however. The incidence of family mental illness in this population is huge, which suggests the importance of resilience at the same time as calling for specific family – and environmentally based – programs in order to break this tendency (Arce, Fariña, & Novo, 2014). Finally, it is necessary to highlight once again the need for early and tailored diagnosis and intervention for ADHD, in order to prevent children and adolescents from suffering lasting consequences. In general terms, based on the participants’ reports, some problems could be related to the ADHD symptoms while others are more likely linked to factors found in prison populations. Firstly, regarding academic failure, there is a statistically significant higher percentage of participants with no schooling in the prison population, and some differences related to ADHD symptoms increase the risk. The same pattern occurs in terms of job and unemployed before prison, or differences in substance abuse, or mental health problems in the family with some influence of ADHD symptoms or diagnosis. On the other hand, some social variables like earning money from the informal economy and from subsidies or a higher percentage of divorce are more prevalent in the prison population. Also, participants in the prison setting reported more family problems with drugs and higher percentages in substance abuse of the different types of drugs. Limitations and Directions for Future Research It is necessary to acknowledge some limitations in the present study. First, it is important to note that the sample was not evenly distributed between genders, with a higher proportion of male participants, especially in the prison group. Although some studies have been carried out with female prisoners (Hennessey et al., 2010; Konstenius et al., 2015), which support some of our findings, it would be advisable to have more balanced groups for future research. Second, it would be useful to include a measure of the severity of the symptoms in the clinical sample, in order to test whether this variable could explain some of the differences found in our study (González-Castro, Rodríguez, Cueli, García, & Alvarez-García, 2015). Third, the prison ADHD group was identified from responses to the ASRS scales and their diagnosis was then confirmed with ADHD Rating Scale-IV. The fact that only self-report measures were used to verify the diagnosis of ADHD may be a limitation in the present study: there would be adults with ADHD symptoms and not with ADHD diagnosis. Fourth, the composition of the clinical sample of psychiatric outpatients may also have some implications. It is worth noting that no differences were found in ADHD symptoms between the ADHD prison group and the non-ADHD clinical group. This finding could be explained by the presence of comorbid disorders in the clinical group. In fact, the whole clinical sample (with and without ADHD) scored significantly higher than the other groups on the ADHD scale, which may be explained by comorbidity with other clinical disorders. Some of the clinical conditions reported by the outpatient participants included depressive symptoms, anxiety, obsessive-compulsive behavior, etc. Some of these conditions share characteristics or may lead to inattention or impulsiveness. Thus, a more detailed analysis of comorbidity and its implications for ADHD self-reported symptoms must be conducted in future studies. Finally, our results are limited to two regions in Spain, which raises questions of geographic generalizability. Although our results are in line with several previous international studies, it would be interesting for future research to examine a broader sample which would be more representative of the national context. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgments We would like to thank Dr Stephen Loew and Nigel Marsh for their contribution in the areas of language and style corrections. Cite this article as: García, T., Rodríguez, C., Rodríguez, J., Fernández-Suárez, A., Richarte, V., & Ramos-Quiroga, J., A. (2019). Psychosocial profiles of adults with ADHD: A comparative study of prison and outpatient psychiatric samples. The European Journal of Psychology Applied to Legal Context, 11, 41-49. https://doi.org/10.5093/ejpalc2018a14 Funding: This work was supported by the Regional Government of Asturias under Grant [FC-15-GRUPIN14-053]. References |
Cite this article as: García, T., Rodríguez, C., Rodríguez, J., Fernández-Suárez, A., Richarte, V., & Ramos-Quiroga, J. A. (2018). Psychosocial Profiles of Adults with ADHD: A Comparative Study of Prison and Outpatient Psychiatric Samples. The European Journal of Psychology Applied to Legal Context, 11(1), 41 - 49. https://doi.org/10.5093/ejpalc2018a14
rodriguezcelestino@uniovi.es Correspondence: rodriguezcelestino@uniovi.es (C. Rodríguez).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 CrossRef
CrossRef JATS
JATS