
Barriers Identification as Intervention to Engage Breast Cancer Survivors in Physical Activity
[La identificación de barreras como intervención para involucrar a supervivientes de cáncer de mama en actividades físicas]
Nathalie Andréa, Marine Pillauda, Aurélien Davousta, and Louis Laurencelleb
aCentre de Recherche sur la Cognition et l’Apprentissage, Poitiers, France; bUniversité du Québec à Trois-Rivières, Canada
https://doi.org/10.5093/pi2018a9
Received 11 November 2017, Accepted 22 December 2017
Abstract
This study was designed to demonstrate the advantage of adding cancer barriers to components of decision-making in the transtheoretical model (TTM). In study 1, questionnaires were completed by 139 breast cancer survivors including decisional balance, cancer-related barriers and stages of readiness. In study 2, efficiency of directly tackling cancer-related barriers through motivational-style conversation was tested in a quasi-experimental design. From study 1, all decisionmaking variables were related to stages of readiness, but cancer-related barriers were the sole predictors of engagement in physical activity. Out of the three groups of study 2, only the group with motivational-style conversation displayed a significant progress for engagement in physical activity. Demonstrating that cancer-related barriers predict stage of change above the effects of the two components of decisional balance provides a validation of positions that put cancer-related barriers as uniquely related to stages of change, and suggests that adding them in decision making variables in TTM’s model can provide a genuinely new contribution to the understanding of physical activity adherence. Regarding implication for cancer survivors, these results suggest that in order to stimulate progress in early stages of change, a greater emphasis may be needed on reducing cancer-related barriers.
Resumen
Este estudio fue diseñado para demostrar la ventajas de tener en cuenta las barreras relacionadas con el cáncer en el proceso de toma de decisiones en el modelo transteórico. En el estudio 1 los cuestionarios fueron respondidos por 139 supervivientes de cáncer de mama, en ellos se incluyó el equilibrio decisional, las barreras relacionadas con el cáncer y las etapas de preparación. En el estudio 2 la eficacia de abordar las barreras relacionadas con el cáncer a través de conversaciones de tipo motivacional se puso a prueba con un diseño cuasi-experimental. En el estudio 1 todas las variables de toma de decisiones se relacionaron con las etapas de preparación, pero las barreras relacionadas con el cáncer fueron los únicos predictores de la participación en la actividad física. De los tres grupos del estudio 2, sólo el grupo con conversación de tipo motivacional mostró un progreso significativo para la participación en la actividad física. Demostrar que las barreras relacionadas con el cáncer predicen la etapa de cambio sobre los efectos de los dos componentes del equilibrio decisional proporciona apoyo a la idea de que las barreras relacionadas con el cáncer se encuentran relacionadas con las etapas de cambio y sugiere que su incorporación al proceso de toma de decisiones en el modelo transteórico puede proporcionar una contribución nueva y significativa a la comprensión de la adherencia a la actividad física. Con respecto a las implicaciones para supervivientes de cáncer, estos resultados sugieren que para estimular el progreso en las primeras etapas de cambio, puede ser necesario un mayor énfasis en la reducción de las barreras relacionadas con el cáncer.
Keywords
Decision making, Oncology nursing, Patient compliance, Physical activity, Barriers to change.
Palabras clave
Toma de decisiones, Enfermería oncológica, Cumplimiento del paciente, Actividad física.
Correspondence: nathalie.andre@univ-poitiers.fr (N. André).
Introduction
Although scientific evidence supports the role of physical activity (PA) as a safe and effective intervention for improving health-related quality of life (for a review, see Mishra et al., 2012; Irwin, 2009), the majority of cancer survivors do not comply with public health guidelines (Blanchard, Courneya, & Stein, 2008; Lynch et al., 2010), i.e. at least 150 minutes per week of moderate-intensity aerobic PA throughout the week or at least 75 minutes of vigorous-intensity aerobic PA throughout the week, or an equivalent combination of moderate and vigorous activity (World Health Organization [WHO], 2010). Yet, breast cancer survivors who are active after treatment have a lower risk of cancer recurrence, co-morbidities and death from all causes, compared with those who are less active (Lahart et al., 2015; Gonçalves et al., 2014). As reported by Ellis, Butow, Tattersall, Dunn and Houssami (2001) and Gattellari, Voigt, Butow, & Tattersall (2002), being diagnosed with a life-threatening disease such as cancer could affect decision-making, and many patients struggle with complex and difficult treatment decisions. In the transtheoretical model (TTM) of behavior change, which is one of the most widely used models in cancer research (Duijts, Faber, Oldenburg, van Beurden, & Aaronson 2011; Duijts, van Egmond, Gits, van der Beek, & Bleiker, 2017; Husebo, Dyrstad, Soreide, & Bru, 2013; Spark, Reeves, Fjeldsoe, & Eakin, 2013), the decision-making variables − representing the pros and cons of changing − have been found to have systematic relationships across the stages of change for health related behaviors (Adams & White, 2002; Marshall & Biddle, 2001; Spencer, Adams, Malone, Roy, & Yost, 2006). Every considering behavior change experience an internal conflict regarding the pros and cons of change. This internal conflict must be resolved for a patient to make a decision to change his/her behavior (Prochaska, 2008). Applied to PA behavior, decisional balance concerns the favorable and unfavorable consequences of taking up PA as a lifestyle. In TTM’s literature, cons are defined as one’s belief in the tangible and/or psychological cons of the advised behavior, or as barriers that slow down or halt completion of an ongoing health behavior. Among the reported cons in cancer research, lack of social support, lack of interest and/or motivation, time for family, appear in most studies (Blaney et al., 2010; Brunet, Taran, Burke, & Sabiston, 2013; Rogers, Courneya, Shah, Dunnington, & Hopkins-Price, 2007). Benefits (pros) are commonly defined as one’s belief in the efficacy of the advised action to reduce risk or to increase the impact of the given behavior on health. Among pros reported in breast cancer research, body image, reconditioning, communication, and affective well-being stand prominently (Brunet et al., 2013). The individual weighs the benefits of the behavior change versus its disadvantages (Prochaska, Redding, & Evers, 1997) and an increased decisional balance score indicates a higher motivational readiness to make a behavior change (Boog, 2008). A meta-analysis carried out by Husebo et al. (2013) on the relationships between the TTM and PA adherence reported that the TTM framework includes aspects that predict PA adherence in cancer patients, and thus contributes to the understanding of motivational factors of change in PA behavior with this population. However, in a randomized controlled trial of home-based exercise adherence in recently treated breast cancer survivors, Pinto, Rabin and Dunsiger (2009) reported no significant relation between decisional balance and home-based exercise program. Other studies confirmed the presence of an additional set of PA determinants specifically related to the women’s health status (Courneya, Jones, Mackey, & Fairy., 2006; Miedema et al., 2008; Milne, Guilfoyle, Gordon, Wallman, & Courneya, 2007; Rogers, McAuley, Courneya, & Verhulst, 2008). A recent review on cancer population reported the necessity to identify predictors of greater importance of PA behavior than PA stage of change or decisional balance (Loprinzi, Cardinal, Winters-Stone, Smit, & Loprinzi, 2012). For instance, Charlier et al. (2013) recently reported that cancer-related barriers and self-efficacy in overcoming these barriers were important cancer-related determinants and suggested that interventions be tailored to the experienced symptoms of the women. To the best of the authors’ knowledge, identifying cancer-related barriers as “active ingredients” in decision-making to PA in TTM’s model has never been reported and never been tested in any interventional study with breast cancer survivors. Barriers to a behavior change, defined as those that prevent individuals from initiating a health behavior (e.g., PA), is an important construct, which is contained within almost all major social cognitive models of human behavior. In this perspective, the most distinctive determinant related to adoption of health behavior is reported to be perceived barriers (Rogers et al., 2007, 2011; Bozionelos & Bennett, 1999; Courneya & Friedenreich, 1999). Barriers generally reported in this vein by cancer survivors, like experienced nausea, fatigue, lack of energy, and pain, contribute to directly hinder in taking up PA as a routine (Blaney et al., 2010; Courneya & Friedenreich, 1999; Lewis & Lynch, 1993). According to social cognitive researchers, perceived barriers are recognized as being predictive of decision to change (Arroyave et al., 2008; Walsh, 2006), and as explaining additional variance in both readiness to PA and actual performance of the PA behavior (Rogers et al., 2011; Bozionelos & Bennett, 1999). TTM constructs have previously been applied to the study of PA with cancer survivors but few studies have examined the contribution of cancer- related barriers in decision to change (Bandura, 1997; Benisovich, Rossi, Norman, & Nigg, 1998; McAuley & Mihalko, 1998). Even if overcoming barriers is an effective construct target for facilitating change (Blaney et al., 2010; Loprinzi et al., 2012; Rogers et al., 2011), a question remains: What is the contribution of cancer-related barriers in engagement in regular PA relative to decisional balance? In other words, because adoption of PA is a difficult challenge for healthy adults and is likely to be even more difficult after receiving a cancer diagnosis, and because TTM’s main goal is to explain how health behavior change occurs, a focus is needed on the contribution of cancer-related barriers in order to better respond to TTM’s fundamental principle of stage transition in cancer population. Hence, the aim of our two studies was to determine the contribution of cancer related-barriers to the components of decision-making in Transtheoretical Model (TTM) (Bozionelos & Bennett, 1999; Friedenreich & Courneya, 1996). The importance of these cancer-related determinants in explaining PA in breast cancer survivors remains unclear for two main reasons: first, barriers often are confounded with cons and second, the decision-making to engage in regular PA seems dependent of barriers (Rogers et al., 2011). Our hypotheses were that cancer-related barriers could explain level of engagement in PA more than decisional balance (study 1), and that overcoming cancer-related barriers could facilitate engagement in regular PA (study 2). Study 1 Method Population and procedures. This study was carried out in accordance with the recommendations of the ethics committee of the University hospital of Poitiers, and the protocol was approved by it. Participants came from a sample of 139 women aged from 24 to 80 years (M = 57.53, SD = 12.40), recruited through their appointment notices at three different clinical centers. In each center and at the end of the appointment, the oncologists informed participants about a study on breast cancer and PA, which consisted of 15 minute interview on cancer recurrence prevention and gave an information note. Interested women phoned the research office, the entire study was explained, and eligibility determined, i.e. at least one year post-diagnosis of breast cancer and without metastatic cancer. If interested, women were sent an informed consent form, and an appointment was made for the baseline interview. At the interview (in the participant’s home or setting of choice), written consent was obtained for each respondent according to a university-based protocol. Approximatively two hundred information notes were distributed during one month and 71% of breast cancer women positively replied. This sample was fairly representative of the population with 16% of women aged less than 50 years, 43% of women aged from 50 to 64 years, and 40% of women aged over 65 year (Ferlay et al., 2013). Measures. The following measures were performed in order to conduct the research: Decisional balance. Based on the Marcus, Rakowski, and Rossi (1992) decisional balance scale revised by Plotnikoff, Blanchard, Hotz, and Rhodes (2001), we adapted the scale to PA and breast cancer survivor population, in French. After examining the advantages and disadvantages of exercising with this population, four pros were completed by the participants, including relaxation (I feel better after exercising), social network (PA allows me to come out of isolation), body image (PA is a good way to regain confidence in my image) and reconditioning (Regular PA is one way for me to improve my shape). Concerning cons, four items were formulated including lack of time (If I was exercising, I would have less time for my other personal activities), availability for family (I would have less time to devote to my family if I practiced PA), lack of interest (PA does not interest me), and lack of social support (If I was practicing a PA, my family would be worried about me). Participants responded to each item on a 5-point Likert-type scale ranging from 1 (not important) to 5 (extremely important). Cronbach alpha of the two subscales were .82 for pros and .79 for cons, and close to those of Plotnikoff et al. (2001) .85 and .79, respectively. Cancer-related barriers. Based on Social cognitive theory (SCT)’s variables (Blaney et al., 2010; Rogers et al., 2011), we retained experienced fatigue, experienced side-effects (hair loss, scars), depression, and lack of information. Four cancer-related barriers items were then formulated, for instance: I am too tired to practice regular PA, which represents consequences of treatment that prevents exercising regularly (Bozionelos & Bennett, 1999). We decided to incorporate the guidelines on moderate-intensity PA only because if a barrier appears in moderate-intensity PA, it will remain present in vigorous-intensity PA and in order to avoid discouragement in a sample of inactive or sedentary women. Participants rated on a 5-point scale ranging from 1 (not important) to 5 (extremely important). Cronbach alpha for this set of items was .85, compared to .62 (Bozionelos & Bennett, 1999). In accordance with recommendations of Beaton, Bombardier, Guillement, and Ferraz (2000), the translation process of these two questionnaires included initial translation, synthesis of translations, back-translation, revision by an expert committee, and a test of the pre-final version. Stages of readiness. Stage of readiness for PA behavior was assessed using the Stage of Exercise Change Questionnaire (Reed, Velicer, & Prochaska, 1997). This scale consists of five items that represent the five stages of change (i.e. precontemplation, contemplation, preparation, action, and maintenance). A five-question algorithm was used to sort patients into their appropriate stage of change. Level of engagement in PA. Level of engagement in PA was measured using the NASA/JSC Physical Activity Scale that discriminates level of PA from 0 (I don’t practice regular physical activity) to 7 (I run more than 10 miles [16 km] per week, or walk 14-20 miles per week, or spend 4-6h per week in comparable physical activity such as indoor biking, swimming, cycling, or playing tennis). From 0 to 2, participants are considered as inactive; from 3 to 5, participants are considered as active but under the ACSM recommendations; from 6 to 7, participants are considered fully active (Jackson et al., 1990). Previous research has established the scale’s validity for women aged from 20 to 64 (Jackson et al., 1996). Analyses. Correlation and regression analyses were conducted on all variables involved in decision-making, stages of readiness, and level of engagement in PA. In addition, one-way MANOVA and ANOVAS were used to test for stage differences on these three key constructs of decision-making. Standard regression analyses were performed in order to ascertain the additional contribution of cancer-related barriers to the variance of level of engagement. Results Descriptive statistics. The participants were predominantly married (54%) and 42% were retired. The mean number of months since diagnosis was 20.81 ±10.01, with participants mainly receiving chemotherapy alone (70%). Details of the demographic and medical profile of the participants are given in Table 1. The mean scores for pros, cons, and cancer-related barriers were 3.77 (SD = 0.93), 1.98 (SD = 0.80), and 2.60 (SD = 1.13), respectively. For this sample, internal consistencies (α) were 0.89 for pros, 0.74 for the cons, and 0.74 for cancer-related barriers subscale, α levels being deemed fair considering the small number of scale components. Among breast cancer survivors, 49.6% were in precontemplation, 25.2% in contemplation, 7.2% in preparation, and 18.0% in action/maintenance stages.
Table 1
Demographic and medical profile of study participants 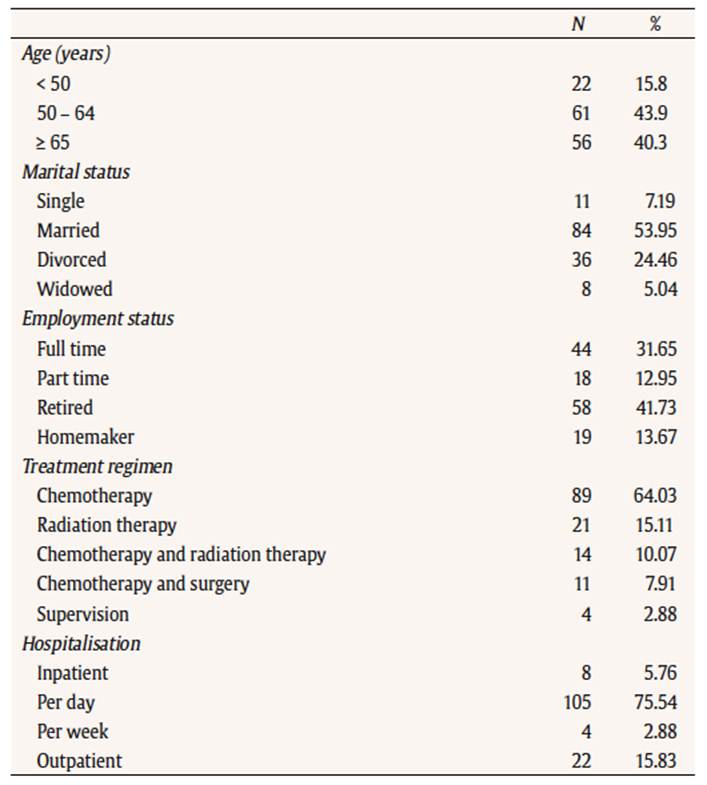
Analyses of variance and correlational analyses. A multivariate analysis of variance resulted in a significant effect of stages of readiness [F(9, 323) = 7.40, Wilk’s lambda = 0.634, p < .001] on decisional variables. The follow-up ANOVAS and outcomes of Tukey HSD test, presented in Table 3, show that for precontemplators, the score in pros is lower and the score in cons is higher comparatively to those of all the other stages. For cancer-related barriers, we observe a higher score in precontemplation and contemplation stages comparatively to action/maintenance stage.
Table 2
Pearson r among study 1 variables (n = 139)* 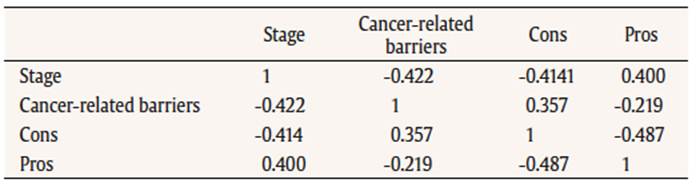
Table 3
Mean (SD) of occurrences of self-reported barriers, and decisional balance scores by stages of exercise behavior change. 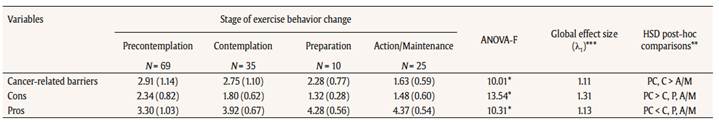
Regression analyses. Pearson’s r levels among the decisional variables ranged from 0.36 to 0.49, as shown in Table 2. To check directly the separate impact of cancer-related barriers on level of engagement, regression analyses were performed, first using pros and cons as the independent variables, and then adding the cancer-related barriers variable. The regression of level of engagement on predictors pros (β = 0.260, p = 0.003) and cons (β = -0.287, p = 0.001) was significant [R2 = 0.223, F(2, 136) = 19.55, p < 0.001. Adding the barriers variable (β = -0.302, p < 0.001) to the pros (β = 0.202, p = 0.004) and cons (β = -0.189, p = 0.030) brought up the explained variance to R2 = 0,302 [F(3, 135) = 19.51, p < 0001], the increment in independent explained variance controlled by cancer-related barriers being highly significant (ΔR² = 0.079, F(1, 135) = 11.58, p < 001]. A further, quasi equivalent analysis, this time through the partial correlation method, gave rP (Barriers, Stage | Cons, Pros) = - 0.318 (p < 0.001), rP (Cons, Stage | Barriers, Pros) = - 0.185, (p ≈ 0.030), rP (Pros, Stage | Barriers, Cons) = 0.245, (p ≈ 0.004), pros and barriers standing out as distinct predictors of engagement. Notwithstanding their redundancy, these results also highlight the distinct and prominent importance of the barriers variable as a moderator of commitment for action. Study 2 The study 1 was aimed at examining the relevance of adding breast cancer-related barriers to decisional balance of the TTM in order to provide evidence of incremental validity of barriers in the understanding of behavior change. Study 2 was set up to check the effectiveness of an eight-week intervention program, during remission period, developed to increase the willingness to adopt PA in sedentary breast cancer survivors. Based on the literature and results of study 1, interventions should focus mainly on pros and cancer-related barriers. Indeed, Skinner et al. (1997) demonstrated that precontemplators may need more benefits-enhancing than cons-reducing interventions. This position is held also by several authors who mentioned that twice as much emphasis should be placed on helping patients appreciate the pros of changing than on decreasing the cons (Prochaska, 2008; Marcus et al., 1992; Plotnikoff et al., 2001; Prochaska et al., 1994). For Rosenstock et al. (1988), interventions designed to increase pros can be applied for people who accept their susceptibility to cancer and fear the consequences of the disease while also believing that there are few cures for cancer. Moreover, according to Janis and Mann (1977), decisional balance provides best results when the decision maker meets all criteria of vigilant information processing. Ever since the initial surge of anxiety from the diagnosis and surgery, women are aware of their vulnerability and the decision maker’s balance sheet is accompanied by arousal of vigilant interest in finding a more desirable course of action. Moreover, results of the foregoing study have stressed the probable importance of barriers as a key determinant for engagement in PA in breast cancer survivors. Consequently, we hypothesized that an intervention aimed at reducing cancer-related barriers and emphasizing pros should facilitate the transition in pre-action stages. MethodResearch design. This study was carried out in accordance with the recommendations of the ethics committee of the University hospital of Poitiers, and its protocol approved by said committee. This quasi-experimental study was designed to take place during routine service appointments. It was conducted in the post-treatment period of breast cancer management service supported by a range of health professionals (health care trainers and nurses) to improve patients’ self-management and quality of life. Health professionals provide individualised care to the patient and make themselves available to work together with her. On average, new patients referred to the clinic are discharged after two months according to their self-management ability. After patients had completed their first appointment and agreed to participate in the study, written consent was obtained for each respondent, in compliance with a university-based protocol. Once patients had signed the consent forms, they were invited into a private room in the clinic for baseline data collection by completing self-reported questionnaires. Two months later, the same set of questionnaires was collected from the patients when they returned back to the service for further consultation. Participants. Forty-five participants in breast cancer remission were recruited in post-treatment period (two months), aged from 54 to 82 years (M = 68.6, SD = 6.2). Thirty-two participants were assigned by the oncologist, as follows: they were included if they were (a) in post-treatment, (b) sedentary (i.e. PA: 0 and < 1 time per week), and if they had (c) no intention to engage in a regular PA program. Once included in the study, they were randomly assigned to the Inactive (n =16) or Inactive + Barriers Educational Session (BES) (n = 16) group by picking an envelope with the appointment for the next 16 sessions. Participants opened the envelope after leaving the session to ensure single-blinding of the researcher. A third group, composed of 13 participants, was recruited with the same criteria except for the (c) condition, since they had decided to start an adapted PA program composed of walking and water aerobics (see Figure 1).
The central aspect of this study being to assess the impact of alleviating perceived barriers for participants through our BES intervention, comparison of this group with the Inactive group was the main statistical issue. As the intervention was targeted to reduce barriers while enhancing the pros of exercising, the hoped-for effect size (Cohen, 1988) was near the high range, say d ≈ 1, which for a α-level of 0.05, required n ≈ 16 per group. A posteriori data calculations showed this speculative sample size to be adequate, the obtained d estimates ranging from 0.971 to 1.660, as shown in Table 5. Interventions. Therapeutic patient education (TPE) was organized for all participants of this study and focused mainly on benefits from practicing regular PA (as suggested by Prochaska et al., 1997). TPE is defined as helping patients acquire or maintain the competences they need to manage their life with a chronic disease as well as possible (Fillion et al., 2008). The sessions were conducted as follows. As part of the therapeutic education sessions taught at the hospital, a health professional gave classes on benefits of regular PA for all participants during 10 minutes by engaging them in conversation exploring the reasons for change (pros) that were most important to them. Then, according to the group to which they belonged, participants had the opportunity either to read some brochure on benefits of PA and to discuss with the health professional, or to follow barriers educational sessions (BES) exploring the cancer-related barriers that were problematical for them in order to reconsider their future engagement in regular PA. Participants carried out two 20 minute sessions per week during eight weeks. Measures. Participants completed a questionnaire of demographic information and items assessing PA level, treatment therapy, and endured side effects. The decisional balance questionnaire, the cancer-related barriers, and engagement in PA scales were completed by all participants. Data analysis. As a precursor to the primary analyses, analyses of variance on change scores (post minus pre intervention) was used to assess for differences between groups, notably with respect to change in engagement in PA; specific test (with the LSD t procedure) compared the Inactive + BES group with its control, the Inactive women group. Due to awkward, non-normal distribution of the engagement and of the other variables, we resorted to a permutation version (Monte Carlo) of ANOVA to estimate F and t probabilities, based on 106 permutation runs. To test for predictors of engagement in PA of cancer survivors, multiple linear regression models were run for all groups and then separately for each group. Here again, we used change scores (post - pre) in engagement as the dependent variable, as well as in the other variables acting as predictors. Results Baseline characteristics and BCP eligibility. There were no significant differences between the groups on baseline demographics, treatment duration, therapy type, visit frequency, and side effects (see Table 4).
Table 4
Comparison between the DB group, the Active group and the Inactive group in relation to the variables studied in the pre-treatment measurement 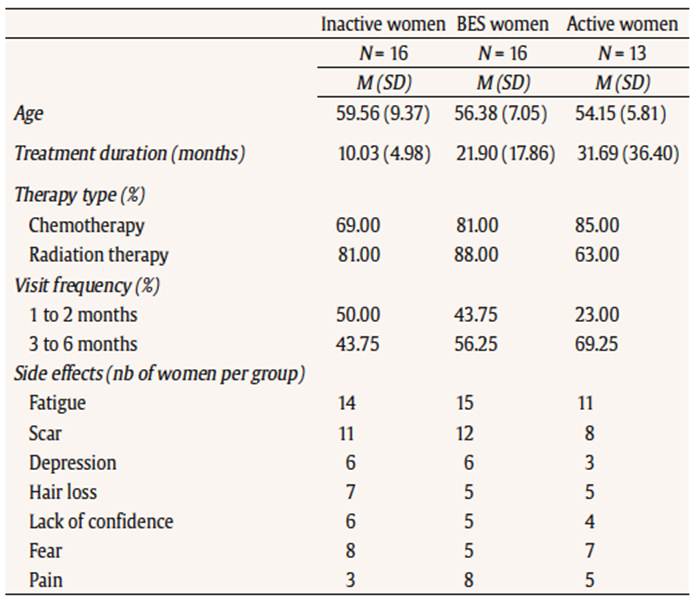
Changes in engagement in PA. We focused on change in engagement in PA from pre-intervention to post-intervention (two months). Between group effects indicate that there was a significant interaction effect for the difference in PA between BES, Active and Control (Inactive) groups [F(2, 42) = 11.531, p < .0001]. For the BES group, intervention session was associated with a strong and significant increase of engagement in PA (mean change = 1.25, SD = 1.18, Cohen’s d = 1.62). For the Control group, engagement in PA was low and kept unchanged (mean change = 0.06, SD = 0.25, d = 0.24), and for the Active group, engagement kept high with a moderate increase (mean change = 0.15, SD = 0.38, d = 0.40; see Table 4). Moreover, the change in engagement was significantly higher for the BES as compared to the Control group, assorted to a high effect size (t = 4.48, df = 30, p < 0.0001, d = 1.58). All predictor variables showed also an appropriate and significant contribution (see Table 5), most of all the barriers variable (t = -4.695, df = 30, p < 0.0001, d = -1.66), the principal objet theme of the TPE intervention.
Table 5
Means and standard deviation comparisons for decisional balance, cancer-related barriers, stages of change and engagement in exercise 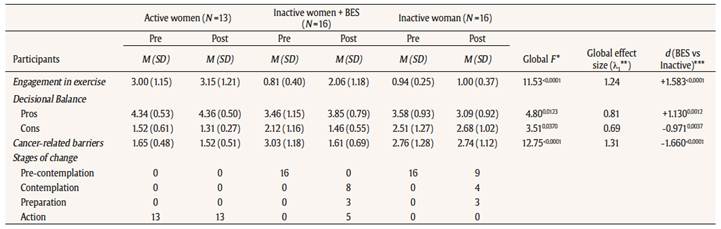
Predictors of change in engagement. A regression model was run for all groups combined in order to determine predictors of engagement in PA, calculations again being based on change scores. The regression obtained a R2 = 0,424 (F = 10.07, p < 0.001) with the reduction in barriers as the only and important predictor (βBarr = -0.682, p < 0.001), the other two being wiped out (βCons = 0.071, βPros = -0.014). Out of curiosity and despite their respective small sizes, regression models were also tried on each of the three groups, the only significant result appearing with the BES group [R2 = 0.350 (F = 2.15, p ≈ 0.147), specifically with βBarr = -0.613, p ≈ 0.047), suggesting that breast cancer survivors who followed BES were more decided to engage in PA. Nowhere did the differences in pros or cons contribute a fair part of variance sustaining engagement. Concisely, change in cancer-related barriers after 2 months of BES was the sole and significant predictor of change in engagement. DiscussionThe aim of these two studies was to verify the usefulness of cancer-related barriers in decision-making with breast cancer survivors when using TTM as a theoretical framework. To our knowledge, the studies were the first to examine readiness to change following a motivationally based intervention that focused on cancer-related barriers with women in breast cancer post-treatment. Primary results provide support for the distinctiveness between these two decisional variables, i.e. decisional balance and cancer-related barriers. First, the results for decisional balance mostly reflect previous findings in other studies summarized by Prochaska et al. (1994). For the pros, the expected significant increase between precontemplation and contemplation could be observed, indicating that the pros of exercising become more relevant to people contemplating it. Pros were not significantly different across contemplation, preparation, action, and maintenance (Keller, Nigg, Jäkle, Baum, & Basler, 1999). However, for cons, our results differ somewhat from previous studies. Whereas the cons were in general lower in action stage than in contemplation, confirming one of the basic assumptions about cons of behavior change, our results showed that cons were higher in precontemplation than in contemplation stages. Cons were associated to the lack of support of the family, lack of social support, lack of time and lack of interest. These are known to influence decision-making in cancer treatment (Van der Molen, 1999), to enhance the perceived stress of cancer survivors and to reduce motivation (Van der Molen, 1999; Chiquelho, Neves, Mendes, Relvas, & Sousa, 2011). This confirms that cons could be at least as important for success as increasing the awareness of the pros. For cancer-related barriers, the expected decrease between contemplation and preparation stages can be observed, indicating that barriers interfere with decision-making until individuals are willing to initiate a change. Among cancer-related barriers reported by cancer survivors, fatigue, depression, and side effects appear predominant. As reported by Mock et al. (2005), and Brawley, Culos-Reed, Angove, & Hoffman-Goetz (2003), fatigue and other side effects contribute to a reduced level of PA and appear as main perceived barriers. The second proof of distinctiveness stems from the regression analysis in study 1: it revealed that cancer-related barriers explained additional, unexplained variance in stages of readiness after controlling for pros and cons, supporting conceptions of cancer-related barriers as uniquely important to behavior change. These results provide the most stringent test yet conducted of whether cancer-related barriers explain stages of change above the effects of the decisional balance. The decisional balance represents some of the most studied decision-making variables in health research (Prochaska, 2008), and was shown to be a strong predictor of stages of change (Marshall & Biddle, 2001). Demonstrating that cancer-related barriers predict stage of change above the effects of the two standard components of decisional balance provides a validation of positions which see cancer-related barriers as uniquely related to stages of change, and suggests that adding them in decision making variables in TTM’s model can provide a genuinely new contribution to the understanding of PA adherence. In brief, interventional procedures for improving adherence to PA ought to take into account cancer-related barriers for three main reasons: (1) they provide a strong incremental validity to any model of behavior change, including TTM, complementing decisional balance; (2) they take into account cancer-specific symptoms and constraints, and (3) they are related both to stages of readiness and PA behavior. Until now, some studies exploring the transition from motivational phase (readiness to change) to a volitional phase (level of PA) failed to show a strong relationship between them (Vallance, Plotnikoff, Karvinen, Mackey, & Courneya, 2010; Adams & White, 2002). These results were reinforced in study 2 wherein breast cancer survivors following therapeutic education only based on benefits of regular PA were not inclined to form intention to change. Notwithstanding the moderate sample size attained, the large effect size measured supports the generalization of these results. Two explanations may be offered. On the one hand, as reported by Irwin (2009) and Schnoll et al. (2002), physical symptoms (e.g. fatigue) or emotional barriers (e.g. depression) can render decision making for PA more difficult for cancer survivors by limiting the activity of women after diagnosis and, then, enhance effectively weight gain, fatigue, deterioration of lean muscle mass and, overall reduction in physical functioning (van Vulpen, Peeters, Velthuis, van der Wall, & May, 2016; Brawley et al., 2003). Moreover, in precontemplation stage, Skinner, Champion, and Hanna (1997) observed that information concerning benefits of PA did not convince precontemplators to form an intention. Briefly, although participants could identify the benefits attached to PA, they quickly emphasized the limitations that fatigue had placed on them in regard to PA. Our results completed these previous studies by showing that participants will have little reason to become contemplators if some barriers are perceived to be incompatible with engagement in PA. As suggested by Blaney et al. (2010), the combination of fatigue and participants’ feeling of being physically ill-conditioned undoubtedly contributed to the decline in PA levels. Cancer-related barriers may serve to determine the uptake of health behaviors among patients with cancer. As supported by Blaney et al. (2010) and Rogers et al. (2011), overcoming barriers appears to be an effective target for facilitating PA adoption as well as an important, distinct moderator variable to be considered in a behavior control model. This strategy presents a challenge in order to reduce the negative impact of these barriers on interest and motivation to PA for breast cancer survivors. Consequently, it appears that cancer-related barriers (or impediments) are considered to be a major sociocognitive determinant that deserves to be clearly assessed in TTM. Summarily, overcoming cancer-related barriers appears to play an important role in the formation of intention by enhancing the control individuals feel towards their disease (Schnoll et al., 2002). This suggests that among facets of the cancer experience that prevent this population from engaging in and adhering to therapeutic PA, cancer-related barriers are a key construct. As long as these barriers persist, individuals cannot potentially upgrade their lifestyle with some success and engage themselves in a regular PA program. Limitation Some limitations of our two studies deserve to be addressed. First, 42% of the participants in study 1 were retired and can be considered as a unique group in terms of time to PA, as well as age-limiting factors (Charlier et al., 2013). It would be needed to check our results with younger women. Second, the number of participants in each group in study 2 could mitigate somewhat the generalization of these results, notwithstanding the strength of the reported effects: more studies, enrolling more participants and possibly using a multi-site design should be done to sanction or verify the validity of our conclusions. Implications Prochaska et al. (1997) reported that increasing the value of the pros might have a greater impact on behavior in increasing the motivation to change than reducing the value of the cons. We can challenge this allegation by considering also cancer-related barriers in behavior change. Indeed, increasing the pros and decreasing the cons should be the same process that involves heightening awareness of advantages and disadvantages of change, a process that may have been previously unrecognized. However, this process is required but is not sufficient for someone to engage in a new behavior. The person’s internal dilemma must be tackled and resolved to approach a decision to change, but decreasing cancer-related barriers is nonetheless required to trigger action. Consequently, in terms of clinical practice, the post-treatment period can be an interesting moment to engage a psychosocial intervention program. Breast cancer women are more sensitive to means intended to reduce risks of relapse, and PA training can help reduce effort and decrease fatigue at any level of work (American College of Sports Medicine, 2012). We targeted two 20 minute sessions per week during 8 weeks but a recent meta-analysis advised that “more may not be better” and the effects are stronger when mixed to PA (Bluethmann, Vernon, Petee Gabriel, Murphy, & Batholomew, 2015). We encourage future research to focus on specific behavioral change techniques rather than general behavioral counselling in order to better understand their effectiveness, and to target larger samples to generalize these effects, especially with vulnerable population. |
Correspondence: nathalie.andre@univ-poitiers.fr (N. André).
Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






