
Changes in Mental Health of Children and Young People in Residential Care: Outcomes and Associated Factors
[Los cambios en la salud mental de los ni├▒os y j├│venes en acogimiento residencial: resultados y factores asociados]
Carla González-García1, Elli Vassiliadis2, Juan M. Moreno-Manso3, Mavi Alcántara4, Jorge F. del Valle5, and Amaia Bravo5
1University of Cantabria, Santander, Spain; 2University of Palermo, Italy; 3Universidad de Extremadura, Badajoz, Spain; 4University of Murcia, Spain; 5University of Oviedo, Spain
https://doi.org/10.5093/pi2022a16
Received 11 March 2022, Accepted 3 October 2022
Abstract
Several studies have evidenced that children in out-of-home care (OOHC), including foster family care and residential care, reveal high levels of mental health disorders (ranging from 40% to 88%). This study examines the outcomes in mental health reported by key residential workers in a group of children and youth (N = 492) between 8-17 years old who were in residential child care (RCC) in Spain. The research also aims to explore the relationship between mental health outcomes and the provision of mental health services (i.e., receiving any mental health treatment) as well as the influence of child, family, and placement factors. The design of this study includes two measures: a baseline (T1) and a follow-up two years later (T2). The results indicated that 29.9% of young people enjoyed sustained mental health; 26% meaningful improvement in their mental health; 23.5% meaningful deterioration; and the remaining 20.5% showed no meaningful change. One of the main findings was that receiving mental health treatment had a significant impact on mental health outcomes. It is crucial to establish protocols and systematic detection tools to assess mental health and ensure detection and referral to proper treatment.
Resumen
La investigación en el ámbito de la protección a la infancia ha destacado la presencia de un alto porcentaje de niños, niñas y adolescentes (NNA) en acogimiento residencial y familiar con trastornos de salud mental (entre el 40% y el 88%). Este estudio tiene como objetivo examinar los cambios experimentados en la salud mental de los NNA durante el proceso de acogida según informan sus educadores de referencia en un grupo de 492 NNA entre 8-17 años que se encontraban en hogares de protección en España. El estudio también tiene como objetivo explorar la relación entre los resultados en salud mental y el tratamiento recibido desde diferentes servicios de salud mental, además de la influencia que puedan ejercer factores del NNA, su familia o el proceso de protección. El diseño del estudio se basa en dos medidas: línea base (T1) y seguimiento dos años después (T2). Los resultados indican que el 29.9% de los NNA mantenía una buena salud mental en las dos medidas, 26% manifestaron una mejora significativa partiendo de niveles clínicos, 23.5% manifestaron un deterioro significativo y el 20.5% no mostraron cambios significativos, manteniendo niveles clínicos en ambas medidas. Una de las principales conclusiones fue que estar recibiendo o no tratamiento en salud mental resultó ser un factor clave en la evolución de los NNA. Por tanto, resulta crucial establecer sistemas de detección de problemas de salud mental en esta población con el fin de derivar precozmente a tratamientos adecuados.
Keywords
Mental health, Residential child care, Mental health treatment, Mental health outcomesPalabras clave
Salud mental, Acogimiento residencial, Protecci├│n a la infancia, Tratamiento de salud mental, Resultados en salud mentalCite this article as: González-García, C., Vassiliadis, E., Moreno-Manso, J. M., Alcántara, M., del Valle, J. F., & Bravo, A. (2023). Changes in Mental Health of Children and Young People in Residential Care: Outcomes and Associated Factors. Psychosocial Intervention, 32(1), 11 - 19. https://doi.org/10.5093/pi2022a16
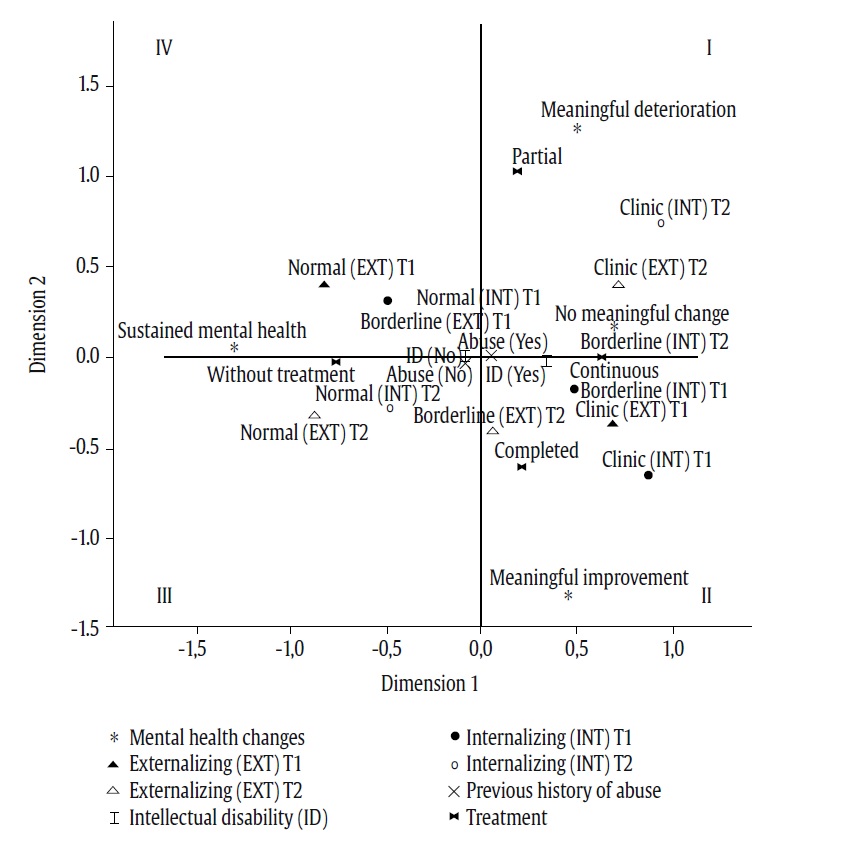
Correspondence: amaiabravo@uniovi.es (A. Bravo).Children and young people in out-of-home care (OOHC) present with high rates of mental health problems. This is particularly the case among those in residential child care, as shown in many countries such as USA, The Netherlands, United Kingdom, Germany, Spain, or France (Bronsard et al., 2011; Burns et al., 2004; Ford et al., 2007; Garland et al., 2001; González-Garcia et al., 2017; Jozefiak et al., 2016; Pecora et al., 2009; Schmid et al., 2008). Despite the disparity of rates, instruments applied, and location among these studies, rates of mental health problems range between 40 and 88% (Bronsard et al., 2011; Burns et al., 2004; González-García et al., 2017; Greger et al., 2015; Sempik et al., 2008). Several studies have revealed high levels of externalizing and internalizing problems (González-García et al., 2017; Schmid et al., 2008; Vanschoonlandt et al., 2013), as well as psychiatric problems in children and young people in child care (Havnen et al., 2012; Lehmann et al., 2013) and specifically in children in residential youth care (Jozefiak et al., 2016). Tarren-Sweeney (2008) reported that OOHC children (including residential, foster, and kinship care samples) manifest complex symptomatology that is not well represented in classification systems, i.e., psychopathology characterized by attachment difficulties, relationship insecurity, sexual behaviour, trauma-related anxiety, conduct problems and defiance, and inattention/hyperactivity, in addition to other kinds of mental health difficulties, such as self-injury and food maintenance behaviors. The development of these psychological problems and disorders can be explained by the presence of adverse circumstances and traumatic events in the family histories of youth, making them a population at high risk (Raviv et al., 2010). In this regard, there is an extensive and useful framework based on the impact of trauma that helps to understand complex symptomatology presented by children with a history of victimization (D’Andrea et al., 2012). The existing evidence shows that the complex trauma explains the wide range of symptoms presented and, above all, emphasizes the importance of trauma-informed practices (Vostanis, 2018). There has been less research focused on the progression of emotional and behavioral problems during the stay of children and youth in OOHC (Attar-Schwartz et al., 2017; Havnen, et al., 2012). Some studies have suggested that the rates of mental health difficulties decrease during their stay in care (Goemans et al., 2015; Lee & Holmes, 2021) while others have shown stable trajectories or even deterioration in the long term in residential care (Attar-Schwartz et al., 2017), in foster or kinship care (Bell et al., 2015; Goemans et al., 2015; Tarren-Sweeney, 2017), and in different care programs (Proctor et al., 2010). A meta-analysis carried out to examine the longitudinal developmental outcomes of children in long-term out-of-home care (focused on regular foster care that does not include therapeutic residential care) included 24 studies on the internalizing problems of the Child Behavior Checklist (CBCL) (N = 1,984), 21 on the externalizing problems (N = 1,729), and 25 studies for the total scale (N = 2,523) (Goemans et al., 2015). Results confirmed the existence of different trajectories, with some studies revealing an improvement and other studies finding major deterioration. The presence of several distinct trajectories for children’s mental health has been also described by Tarren-Sweeney (2017). Following a sample of children in long-term foster or kinship care in New South Wales (Australia) in a prospective study of up to 9 years, the author found that more than 60% of children exhibited either sustained mental health or meaningful improvement in their mental health, while less than a quarter displayed significant deterioration (using as assessment tool the CBCL and Assessment Checklists for Children (ACC). A recent review with children in foster care and residential settings (group homes and residential treatment) examined the variables associated with particular behavioral development paths (Lee & Holmes, 2021). Among the factors that have been identified as predictors of worst mental health outcomes for children in child welfare is older age (Symanzik et al., 2019; Wade et al., 2018), gender (in boys or girls depending on the type of mental health problems) (Habersaat et al., 2018; Hussey & Guo, 2002), placement instability (Bell et al., 2015; Eltink et al., 2018; Konijn et al., 2019; Villodas et al., 2016), previous history of maltreatment (Yoon, 2017), and family background (Attar-Schwartz et al., 2017; Yoon, 2017). Proctor et al. (2010) found that positive trajectories were associated with early child cognitive ability and social competence, long-term caregiver stability, and low frequency of physical abuse in middle childhood and adolescence. Likewise, previous research has also indicated that the number of children in the residential facility receiving mental health treatment and positive parenting were predictors of resilient trajectories (Bell et al., 2015). Research by Attar-Schwartz et al. (2017) examined change trajectories of aggressive behaviors among children in long-term RCC in Israel (N = 799). The results showed that predictors of less resilient trajectories were mothers’ difficulties and disabilities, children’s attendance to special education classes, more intensive care, and non-immigrant status (Attar-Schwartz et al., 2017). Tarren-Sweeney (2017) concluded that research should focus on identifying the interpersonal characteristics of care that promote positive evolution, as well as the characteristics that are developmentally harmful. In this regard, Bellonci and Holmes (2021) have pointed out a lack of evidence to enumerate risk and protective variables associated with the behavior problems and wellbeing in children and young people in RCC. Therefore, longitudinal studies of children in care constitute a major priority that will enable us to identify which children and young people are more likely to make positive gains during their stay in care with the aim of adjusting the interventions to the specific needs and particularities of these profiles. The Current Study In Spain, 49,171 children and youth were in OOHC in 2020 according to the latest national statistics (Observatorio de la Infancia, 2021), with just over half (52%) in RCC. Several national studies have demonstrated high rates of victimization and mental health problems in children in RCC (Águila-Otero et al., 2020; Águila-Otero et al., 2022; Fernández-Artamendi et al., 2020; González-García et al., 2017), in addition to failures in the therapeutic coverage of these problems (González-García et al., 2017). However, there are no studies of children in RCC examining children’s mental health outcomes while in RCC. Given the lack of data, this research is the first study evaluating the evolution of emotional and behavioral problems in children in RCC and analyzing the factors associated and its practical implications. Consequently, our research examines the changes in mental health outcomes in a group of 492 children and youths who have been living in RCC for at least 24 months and who were attending mental health services. We also explored the interdependence between mental health outcomes and the provision of mental health services (receiving any mental health treatment), as well as child, family, and placement factors. According to previous research, we hypothesize that there will be different mental health pathways and that some groups will experience little improvement in their mental health problems. We also consider that the variable “provision of mental health services” will be a key factor in understanding the results. Participants The baseline study collected information about 1,216 children who had been living in RCC for at least 3 months (T1) and a follow-up study was carried out 24 months later (T2) with those children who remained in RCC after two years. The final sample consisted of 492 children and young people since many of them (n = 655) had moved out of RCC due to different reasons, mainly reaching the come of age, family reunification, or transfer to foster care. The sample at T2 comprised 492 participants, 228 females (46.2%) and 265 males (53.8%), between 8 and 17 years of age (M = 13.96, SD = 2.46) who had been living in residential child care for at least 24 months (Mmonths = 70.67, SD = 35.60), since that was the follow-up period. Most of the sample was Spanish, but there were also 2.2% (n = 11) of unaccompanied migrant children (UMC) (more descriptive data can be found in Table 1). The sample came from 80 children’s homes in the Spanish regions of Asturias (n = 105), Cantabria (n = 13), Extremadura (n = 105), Murcia (n = 22), Guipúzcoa (n = 43), Tenerife (n = 59), and 7 SOS Children’s Villages (divided into different units) in regions of Madrid, Barcelona, Cuenca, Pontevedra, Granada, Tenerife, and Zaragoza (n = 145). Children and young people were fostered in different types of residential care facilities, with most of them living in basic network homes or children’s homes specifically for adolescents (95%), while the rest were in homes for children and young people with specific needs or profiles (UMC’s homes, homes for children with disabilities and therapeutic residential care for young people with emotional and behavioral problems). Table 1 Mental Health Changes and Child, Family, Placement, and Treatment Variables  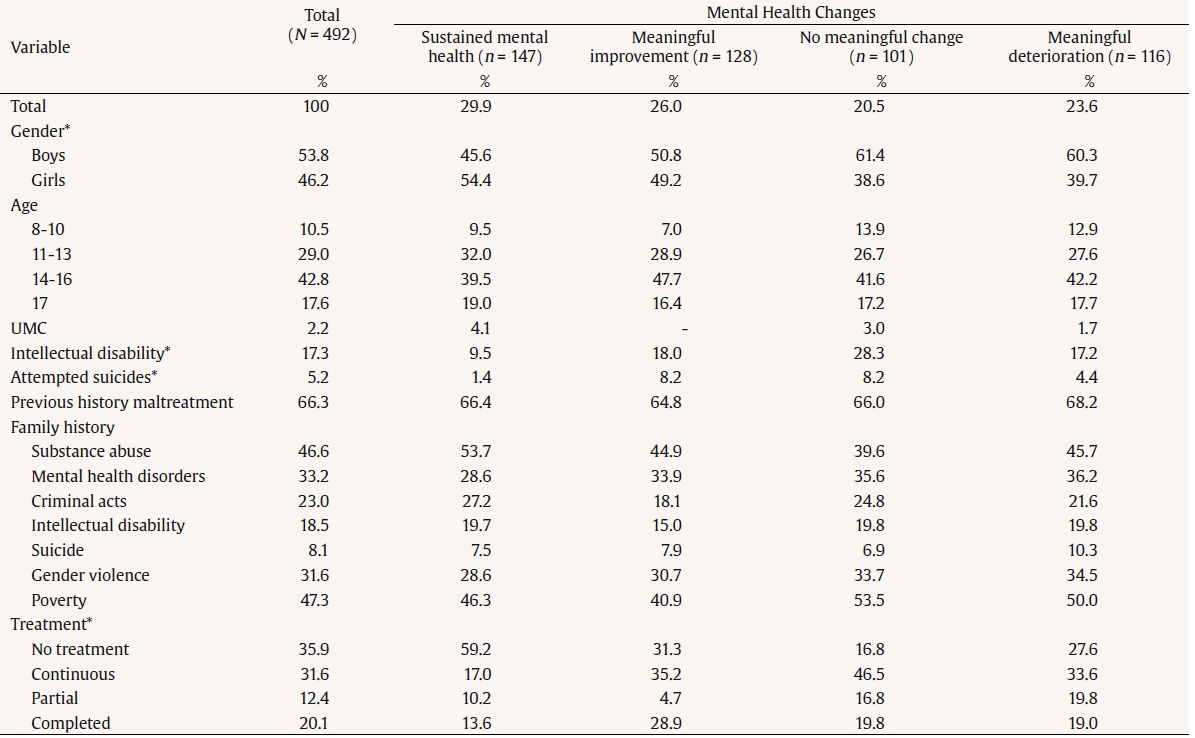 Note. UMC = unaccompanied migrant children. *p ≤ .05. These regions were selected because of two criteria: for its representativeness in the national context (geographical and cultural diversity) and because of the permission obtained of the regional care authorities. All children living in RCC in these regions were included at the beginning of the study after getting the consent from care authorities. The only exclusion criteria for the present study were 1) the non-validity of CBCL in those cases where the instrument was not fully completed at T1 (baseline) or T2 (follow-up) (n = 48) and 2) the existence of missing data about mental health background (n = 20). Therefore, the sample was finally reduced from 561 to 492. Procedure The requirements of Spanish Law 15/1999 on the Protection of Personal Data were met and data confidentiality were guaranteed by means of a code to ensure anonymity. This study was conducted in accordance with the ethical requirements established by the 1964 Declaration of Helsinki for research studies with human beings. The research was also approved by the Secretariat of Welfare and Social Affairs of the Ministry of Economy and Competitiveness of Spain, which also funded this study. Furthermore, recruitment was carried out after obtaining permission from local authorities and the legal tutors (the birth family or the regional authority). Prior to data collection, researchers were in charge of explaining the instructions of the study. They visited each residential facility to explain the study to the young people and obtain their signed permission and informed consent to participate in the research for data collection at T1 and T2. To collect follow-up data regarding participants still in RCC, a procedure was developed to control sample changes in each residential facility through regular contact by telephone and e-mail between the researchers and the person in charge of each residential facility. When a child or a young person was going to leave the facility, the reason and date of departure were registered. These cases were not included in the study. Measures Sociodemographic, Family, and Treatment Information Characteristics and risk factors in children and young people were collected at T1 through an ad hoc questionnaire based on the Residential Care Evaluation and Registration System (SERAR, for its acronym in Spanish) (Bravo et al., 2015), a monitoring system implemented in several regions of Spain to collect relevant information in each case. We gathered information about child (gender, age, UMC, intellectual disability, and attempted suicides), previous history of abuse and/or neglect, family background, and mental health treatments. Table 1 shows the variables that were collected. Regarding the suicide variable, information was collected from children and young people who had attempted suicide according to what was recorded in their files. The criterion for intellectual disability corresponded with those cases with a legally recognized disability (formal diagnostic and certification of disability). The provision of mental health services refers to receiving any kind of mental health treatment, which will be referred to as the “mental health treatment” variable from now. The key/responsible residential worker (in Spain social educators) of each child answered this questionnaire. Variables were organized dichotomously (No/Yes), except for age (categorized by ranges 8-10, 11-13, 14-16, and 17) and treatment. Treatment information was collected at T1 by asking the key residential worker if the child was receiving mental health treatment including psychiatric, pharmacological (receiving prescription drugs, but supervised by other health professionals), and/or psychological treatment. The same information was collected about treatment status at T2, so that we could differentiate four treatment modalities: “continuous” (in mental health treatment during the 24 months between T1 and T2; n = 156), “completed” (individuals who had finished their treatment during the follow-up period for many different reasons; n = 99, so they were in treatment in T1 but not in T2 ), “partial” (individuals who were not attending any mental health services at the beginning of the follow-up [T1], but started later [along T2]; n = 61), and “without treatment” (no treatment during the 24 months; n = 177). Mental Health Outcomes The Child Behavior Checklist/6-18 (CBCL; Achenbach & Rescorla, 2001) is one of the most commonly used instruments to identify internalizing and externalizing behavior in children aged 6-18 years. It was answered by the key residential worker of each child or youth. CBCL has broad assurance of reliability and validity, which has been tested in samples from many countries and cultures (Achenbach et al., 2008), including Spain (Sardinero et al., 1997). CBCL consists of 113 items with three response options: (0) not true (as far as you know), (1) somewhat or sometimes true, (2) very true, or often true. It provides eight empirically-derived clinical sub-scales and three broadband scales: internalizing, externalizing, and total. The scores from the tests were transformed into T-scores that classify the cases into three ranges: normal (≤ 59), borderline (60 ≤ 63), and clinical (≥ 64) for the broadband scales, and normal (≤ 64), borderline (65 ≤ 69), and clinical (≥ 70) for the eight subscales. The CBCL has shown to be effective in detecting psychopathological problems (Deutz et al., 2016; Van Meter et al., 2014; Volkl-Kernstock et al., 2016) or to monitor treatments (Walter et al., 2018). Defining Meaningful Prospective Changes in Mental Health Scores To define meaningful changes in CBCL scores, we followed the method established by Tarren-Sweeney (2017) in a follow-up study with children in long-term out-of-home care. This author made a distinction between statistical significance, clinical significance, and the degree of change that entails developmental and social meaning. One of the most widely used methods is the reliable changes index (RCI) (Jacobson & Truax, 1991), a psychometric criterion that discriminates the magnitude of change that is significant, thereby identifying changes in scores that are not attributable to internal measurement. Tarren-Sweeney (2017) follows a somewhat more conservative definition of meaningful change than the RCI, defining meaningful change as an increase (meaningful deterioration) or decrease (meaningful improvement) of 12 or more points on CBCL total problems scale. Two sets of measures were defined from the dispersion of scores across the clinical range and cut-off points. Thus, this approach defines change in CBCL total scores in terms of the gap between the highest score in the normal range, and the lowest score in the clinical range (this means a 12-point score differential), that was also selected in this study as cut-off score to distinguish meaningful change on the CBCL total problems scale. Following this approach, the present study also distinguishes four mental health groups: A, “sustained mental health”; B, “meaningful improvement”; C, “no meaningful change”; D, “meaningful deterioration”. The “sustained mental health” group is composed of those children whose scores were in the normal ranges at both T1 and T2. In contrast, the definition of “meaningful change” was applied to create the remaining groups. Young people with “meaningful improvement” (B) obtained clinical score in T1 and showed an improvement of at least 12 points in T2; those with “meaningful deterioration” (D) showed a worsening of at least 12 points in T2, reaching a clinical range or getting a worse level into the clinical range; finally, those with “no meaningful change” (C) showed clinical score in T1 and its improvement or deterioration in T2 did not reach the 12 points necessary to consider the change to be significant. Data Analyses Firstly, the four mental health groups (sustained mental health, meaningful improvement, no meaningful change, and meaningful deterioration) were analyzed following the approach of Tarren-Sweeney (2017) described above. Secondly, bivariate analyses by means of χ2 were used to explore the relationships between the four groups and child, family, placement, and treatment variables. A value of p ≤ .05 was established as the degree of significance in these analyses, except for standardized corrected residuals, for which values below -1.95 or higher than 1.95 were set. Size effects were calculated using Cramer’s V for categorical variables. Thirdly, we carried out multiple correspondence analysis (MCA) to explore the interdependencies between variables under study and identify groups of children and young people with similar characteristics with respect to such variables. This is a factorial exploratory analysis introduced in the 1970s by the French school of data analysis (Benzécri, 1973) widely used to explore categorical variables. It examines the relationship between a set of categorical variables and synthesizes them into a small number of latent variables (dimensions or factors) that are capable of accounting for a large part of the variability contained in the data. The variables can be included in the analysis plan with different roles, depending on whether the variable contributes to the formation of the factorial axes (active variables) because they enter directly into the analysis. Meanwhile, the other variables are used after extracting the factorial axes and their role is to contribute to the interpretation of results, according to their position in the factorial plan (illustrative or supplementary variables). MCA results in mutually independent factors that are linear combinations of original variables and reproduce the maximum inertia present in the data in descending order. The number of active variables and modalities associated with them determines the total inertia in MCA. Factorial coordinates enable factorial axes to be interpreted, inasmuch as they express the projection of the original modalities on the factorial plan, as well as the relationships between modalities and factors. The formation of the factorial axis is associated with the highest values on a factor. Additionally, closer modalities in the factorial plan indicate greater interdependence. Data analyses were performed using SPSS v26.0. Changes in Mental Health Findings indicated that 29.9% (n = 147) of the young people manifested sustained mental health, 26% (n = 128) displayed meaningful improvement in their mental health, 23.5% (n = 116) exhibited meaningful deterioration in their mental health, and the remaining 20.5% (n = 101) showed no meaningful change. Table 1 illustrates these groups and their relationship with child, family, placement, and treatment variables. Significant associations were detected through a chi square analysis with the variables sex (χ2 = 8.79, p = .032, V = .134), intellectual disability (χ2 = 14.56, p = .002, V = .172), attempted suicides (χ2 = 9.453, p = .038, V = .133), and treatment (χ2 = 74.76, p < .001, V = .225). A significant relationship between these variables was found, as described below. With reference to the sex variable, girls were more concentrated in the “sustained mental health” group, while boys were more present in “meaningful deterioration or no meaningful change”. With respect to those who had an intellectual disability, they were more present in “no meaningful change”, while their percentage was significantly lower in “sustained mental health”. Regarding young people who had attempted suicides, their percentage is very low in “sustained mental health”, while they present higher values in “meaningful improvement” and “no meaningful change”. As for the treatment variable, young people who had not received treatment were to a greater extent in “sustained mental health”, while they presented a significantly lower percentage in “no meaningful change”. On the contrary, those with continuous treatment had lower percentages of “sustained mental health” and higher percentages of “no meaningful change”. Young people who received partial treatment showed lower percentage of “meaningful improvement”, and higher percentage of “meaningful deterioration”. Finally, those who completed treatment were mostly present in “meaningful improvement”. Based on these findings, we made multiple correspondence analyses with those variables that were significantly associated with changes in mental health, to have a complete view of the underlying interdependencies. Multiple Correspondence Analyses To carry out MCA, we have selected eight variables from a wide set of variables collected in the study. Six were used as active variables in the formation of the factorial axes, i.e., “mental health change” (sustained mental health, meaningful improvement, meaningful deterioration, or no meaningful change), “treatment” (continuous, completed, partial, or without treatment), “internalizing” and “externalizing” at T1 and T2 (normal, borderline, or clinic scores), for a total of 20 active modalities. The other two variables were used as illustrative variables in order to enrich the interpretation of the factorial plan, i.e., “intellectual disability” (No/Yes) and “previous history of maltreatment or abuse” (No/Yes). As reviewed in the introduction, there are different factors associated with changes of mental health children and young people in RCC. The reason for including these variables in MCA is their high significant association in this study (e.g., mental health change, treatment, intellectual disability) or in previous literature (e.g., maltreatment), and their representativeness of the CBCL scores (internalizing and externalizing scales at different times). According to MCA results, the first dimension explained 46% of total variance and the second dimension, 27%; consequently, the two factorial axes account for 73% of the total inertia. It may be useful to specify that total inertia does not have the same meaning in MCA than in a factor analysis, because it depends on the number of active variables and associated modalities. In this kind of analysis, in fact, the inertia explained may not be very high due to the large number of modalities (and consequently of variability) present in the data matrix. Table 2 gives the discrimination measures that link variables and factors. Almost all the variables were associated with the first dimension, except for the “mental health change” variable, which is more closely related to the second dimension. Table 2 Measures of Discrimination of MCA   Note. MCA = Múltiple Correspondence Analysis; Int = Internalizing; Ext = Externalizing. Figure 1 shows the first factorial plane on which the active and illustrative variables included in the analysis have been projected. The first dimension evolved from “normal” scores in internalizing and externalizing according to the CBCL at T1 and T2 on the negative semi-axis to “borderline” or “clinical” scores on the positive semi-axis. In contrast, the second dimension illustrated “meaningful improvement” at the bottom of the positive semi-axis and “meaningful deterioration” at the top. Furthermore, “sustained mental health” was close to normal scores on the negative-semiaxis while “no meaningful change” was on the opposite side, on the positive semi-axis. As regards the treatment variable, “no treatment” was related to normal scores on the internalizing and externalizing scales and to “sustained mental health” on the negative semi-axes (see Figure 1). Conversely, “continuous treatment” was found to correlate with clinical and borderline scores on the CBCL on the positive semi-axis. Moreover, at the bottom of the positive-semiaxis, “significant improvement” was shown to be associated with “completed treatment”, while at the top we can see the proximity of “partial treatment to significant deterioration”. The illustrative variables (“intellectual disability” and “previous history of maltreatment”) were in proximity to the origin of the axes and present the respective modalities in the opposite semi-axes of the first dimension. Both were found on the positive semi-axis, where borderline and clinical scores were also located. Meanwhile, the modalities “No ID and No previous history of maltreatment” were on the negative semi-axis, where the normal CBCL scales scores were also found. Similarly, “ID” was close to continuous treatment and no meaningful change. From the arrangement of the modalities of the variables in the factorial plan described, the first dimension can be interpreted as a synthesis of the internalizing and externalizing scales of the CBCL and treatment. However, the second dimension is represented by the “changes” on children’s mental health. Finally, we projected the children and young people of our sample on the factorial plan. Based on the distribution of points represented in the figure we identified four possible groups (Figure 2) and proceeded to describe them based on the interpretation of the dimensions. The first group whose children and youths who were on the negative semi-axis of first dimension were those who had sustained mental health, had not received any type of treatment, and scored in the normal range on the CBCL scales at T1 and T2 (see Figure 2). Additionally, they did not have ID and have not suffered any history of maltreatment or abuse (IV quadrant). It can also be found children and young people without treatment, normal scores on the CBCL, and sustained mental health in this semi-axis (III quadrant). For its part, those who manifested a clinical or borderline score on the CBCL scales had a prior history of maltreatment and ID were located on the positive semi-axis of the first dimension (I and II quadrant). Specifically, in the first quadrant we found children and youths with partial treatment and who have suffered meaningful deterioration, while those who completed treatment and who have had meaningful improvement are found in the second quadrant. Finally, the last group was made up of those who had continuous treatment and no meaningful change (II quadrant). This study captures the results of the follow up of a sample of children and youth in residential care in Spain for the first time. One quarter (26%) of them exhibited meaningful improvement in their mental health, 23.5% displayed meaningful deterioration in their mental health, 20.5% showed no meaningful change, and, finally, the remaining 29.9% manifested sustained mental health. Earlier studies have identified variables related with being older, the instability of the measure, previous history of maltreatment, or the risk family factors as being correlated with worse evolution (Bell et al., 2015; Hussey & Guo, 2002; Lee & Holmes, 2021; Villodas et al., 2016; Yoon, 2017). In this study, MCA identified the kind of path to treatment and, consequently, whether the young person received some type of therapeutic intervention (psychological, psychiatric, and/or pharmacological) during the study period as a key variable in the course of these problems. Two groups emerged as being essential because of their implications: those who were in continuous treatment and, in turn, linked to the “no meaningful change” (20.5%) group, and the group that received partial treatment associated with “meaningful deterioration” (23.5%). Bellamy et al. (2010), in a follow up of a sample of 439 boys and girls, found that a sizeable number of cases that received some kind of therapeutic care from outpatient mental health services did not display significant improvement. The existence of a group in continuous mental health treatment (at least for two years) that fails to evidence improvements speaks to the need to evaluate the effectiveness of the mental health treatments being used and, hence, the importance of conducting more studies of treatment cost-effectiveness (Vostanis, 2010) that enable clinical interventions that best suit these profiles to be identified. Likewise, the therapies that appear to be most fitting for the profiles in care should make an effort to meet the needs of children and young people in RCC, which is subject to greater instability in their lives and ever-changing environments (González-García et al., 2017; Vostanis, 2010). Moreover, Tarren- Sweeney (2010) highlights the importance of therapists having specific training to intervene clinically in light of the particularities of the needs these young people present. In keeping with the results, the group who received partial care associated the most negative change in mental health outcomes. Numerous studies have already underscored the difficulties in detecting those individuals who are clinically in need of treatment and their subsequent referral for care, with many cases with unmet mental health needs who are not being treated because they are not being detected (Burns et al., 2004; González-García et al., 2017). This reality reiterates conclusions that point out the importance of establishing protocols that guarantee adequate detection and referral to treatment (Fong et al., 2018; Pecora et al., 2009). Martín et al. (2020) report on instruments, such as the CBCL used in this study, as being a good tool to assess psychopathological problems and detect young people with clinical needs, as well as also being useful in monitoring treatment impact in mental health (Walter et al., 2018). The use of robust psychometric measures as key for stirring decision-making in OOHC is becoming increasingly relevant in Spain in the area of assessing young people’s preparation for independent living previous to leaving care (García-Alba et al., 2021; García-Alba et al., 2022). It is also imperative to indicate that the very existence of cases that are not referred to mental health treatment may also be due to young people’s resistance to attend mental health services (Aventin et al., 2014) or to previously failed therapies and the turnover of professionals and services (González-García et al., 2017). The negative changes in mental health outcomes of this group makes it impossible to call into question the relevance of early interventions in preventing the chronification of mental health issues (Thompson, 2009). As far as the results of the MCA regarding the supplemental variables are concerned, the overrepresentation of cases of intellectual disability in the group of continuous treatment and no meaningful change is particularly noteworthy. This group has already been mentioned owing to their elevated presence in foster care (Hill, 2012) and to their special vulnerability and specific mental health needs (Águila-Otero et al., 2018; Tarren- Sweeney, 2008). Studies such as the one by Anctil et al. (2007) in out-of-care youths have already found that young people with any kind of disability follow a course characterized by a greater gap in different areas of adulthood, most striking in the high prevalence of mental health diagnoses. Earlier results suggest that a greater proportion of this group is referred for mental health treatment with psychotropics (Águila-Otero et al., 2018; González-García et al., 2017). Nevertheless, the outcomes of this study again point to the need to review the interventions and development of these cases in RCC and the treatments used with these children and young people. An analysis is needed into the suitability of treatments and interventions to the kinds of issues these young people present. This analysis would also benefit from the comparison of interventions and support received by children and young people with ID without an OOHC background, considering that certain experiences might impact differently in their trajectories (García-Alba, Gullo, et al., 2022a). Conclusions Like previous studies, these data confirm the existence of very diverse situations in care, such that some young people exhibit improvement, while other get worse (Goemans et al., 2015; Lee & Holmes, 2021; Tarren-Sweeney, 2017). The main conclusion from this study reaffirms the need to conduct more longitudinal studies (Havnen et al., 2012) that make it possible to identify which factors foster fewer problems and more favorable outcomes in residential care and, in contrast, which variables are linked to a more unfavorable course (Tarren-Sweeney, 2017). This study identifies the type of provision of mental health services as a key variable in the changes of mental health problems. The results enable us to state that referral to mental health services does not suffice (Bellamy et al., 2010) and that the effectiveness of the models and treatments being implemented in outpatient mental health services must be reviewed, as does the child protection system itself (Tarren-Sweeney, 2010; Vostanis, 2010). Evidence-based interventions that have proven effectiveness with the profiles in care must be promoted (Bellamy et al., 2010; Pecora & English, 2016; Vostanis, 2010). This study also emphasizes the need to examine the particular situation of young people with physical and psychiatric disabilities, given that their outcomes appear to be more compromised than that of their peers (Anctil et al., 2007). Limitations Despite the fact that this study yields highly important conclusions, it does have its limitations. Firstly, some of the variables that research has shown to be fundamental in young people’s development, such as the instability of the measure and parents’ history, have not proven to be substantial in our study. This could possibly be due to a loss of information or the way information was collected, which may have contributed to those variables failing to yield valuable conclusions in this study. In this line, there are other variables that have been reviewed in the introduction that should be included in the design of future studies (e.g., the number of children in the residential facility, long-term caregiver stability, characteristics of mental health treatment). Regarding the treatment, it would be important to delve into the nature of the mental health treatment, reasons for referral, and discharge. Secondly, an inherent limitation of longitudinal studies is the stability of informants. Although the informant at T1 and T2 was always the key educator, in some cases it may have changed, and this should be evaluated in future studies. Thirdly, the results are based on the CBCL as an assessment tool to examine how problems evolve; another type of instrument should be included, as well as the information reported by the young people themselves, to get other informants’ view. Finally, future studies should be conducted with more prolonged follow-up times, thereby enabling the weight of other variables to be identified, in addition to monitoring treatments for longer, gathering more information about treatment characteristics. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: González-García, C., Vassiliadis, E., Moreno-Manso, J. M., Alcántara, M., del Valle, J. F., & Bravo, A. (2022). Changes in mental health of children and young people in residential care: Outcomes and associated factors. Psychosocial Intervention, 32(1), 11-19.https://doi.org/10.5093/pi2022a16 Funding: This research has been supported by the Ministry of Economy and Competitiveness of Spain through the National Plan of I + D + i (Ref. PSI2012-33185). |
Cite this article as: González-García, C., Vassiliadis, E., Moreno-Manso, J. M., Alcántara, M., del Valle, J. F., & Bravo, A. (2023). Changes in Mental Health of Children and Young People in Residential Care: Outcomes and Associated Factors. Psychosocial Intervention, 32(1), 11 - 19. https://doi.org/10.5093/pi2022a16
Correspondence: amaiabravo@uniovi.es (A. Bravo).Copyright © 2026. Colegio Oficial de la Psicología de Madrid









 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






