Evaluation of a Child-centred Psychosocial Healthcare Intervention (KIDPROTEKT) – Results of a Cluster Randomized Controlled Trial in Paediatric and Gynaecologic Practices
[La evaluaciĂłn de la asistencia sanitaria psicosocial centrada en el niño (KIDPROTEKT): resultados de un ensayo clĂnico aleatorizado por conglomerados en clĂnicas pediátricas y ginecolĂłgicas]
Désirée Kolodziej1, Philipp Wolkwitz1, Gerhard Schön1, Sönke Siefert2, and Silke Pawils1
1University Medical Center Hamburg-Eppendorf, Hamburg, Germany; 2Catholic Children’s Hospital Wilhelmstift, Hamburg, Germany
https://doi.org/10.5093/pi2023a2
Received 24 March 2022, Accepted 11 October 2022
Abstract
KID-PROTEKT is a child-centred psychosocial healthcare intervention which aims at improving the identification of psychosocial needs and navigation in the outpatient gynaecologic and paediatric setting. In this cluster randomized-controlled trail we examined the effect of KID-PROTEKT on the referrals (to support services) in comparison to the regular gynaecologic and paediatric outpatient healthcare . A variant based on the qualification of the healthcare providers (qualified treatment, QT) and a variant with social worker (supported treatment, ST) were compared to the regular healthcare (treatment as usual, TAU). Twenty-four gynaecologic and paediatric practices were randomized to one of three study arms. Therefore 8,458 pregnant women and families recruited in one of these practices were enrolled in the study. Participating patients reported on average 1.73 (SD = 1.34) psychosocial risks. In total 522 patients were linked to a support service. Compared to TAU, the probability of a referral was significantly higher in QT (OR = 10.70) and ST (OR = 11.28). Also, a higher number of psychosocial risks were linked to a referral (OR = 2.72). These findings support the importance of a psychosocial assessment in the gynaecologic and paediatric setting.
Resumen
KID-PROTEKT es una intervención en asistencia sanitaria psicosocial centrada en el niño, cuyo objetivo es mejorar la detección de las necesidades psicosociales y la navegación en un entorno ambulatorio ginecológico y pediátrico. En este ensayo clínico aleatorizado por conglomerados analizamos el efecto de KID-PROTEKT en las derivaciones (a los servicios de apoyo) en comparación con la asistencia ginecológica y pediátrica externa periódica. Se comparó una variante basada en la cualificación de los proveedores de asistencia sanitaria (tratamiento cualificado, TC) y otra variante con trabajador social (tratamiento de apoyo, TA) con la asistencia sanitaria periódica (tratamiento habitual, TH). Se aleatorizaron 24 servicios ginecológicos y pediátricos en una de las tres ramas del estudio. De este modo participaron en el estudio 8,458 mujeres gestantes y familias reclutadas en una de estas prácticas. Los pacientes participantes notificaron una media de 1.73 (DT = 1.34) riesgos psicosociales. En total se vinculó a 522 pacientes a un servicio de apoyo. En comparación con el tratamiento habitual, la probabilidad de una derivación fue significativamente elevada en el tratamiento cualificado (OR = 10.70) y de apoyo (OR = 11.28). Igualmente se vinculó un elevado número de riesgos psicosociales a una derivación (OR = 2.72). Los resultados confirman la importancia de la evaluación psicosocial en el tratamiento ginecológico y pediátrico.
Keywords
Psychosocial stress, Prenatal stress, Screening, Intersectoral cooperation, HealthcarePalabras clave
EstrĂ©s prenatal, EstrĂ© prenatal, RevisiĂłn, CooperaciĂłn intersectorial, Asistencia sanitariaCite this article as: Kolodziej, D., Wolkwitz, P., Schön, G., Siefert, S., & Pawils, S. (2023). Evaluation of a Child-centred Psychosocial Healthcare Intervention (KIDPROTEKT) – Results of a Cluster Randomized Controlled Trial in Paediatric and Gynaecologic Practices. Psychosocial Intervention, 32(1), 33 - 42. https://doi.org/10.5093/pi2023a2
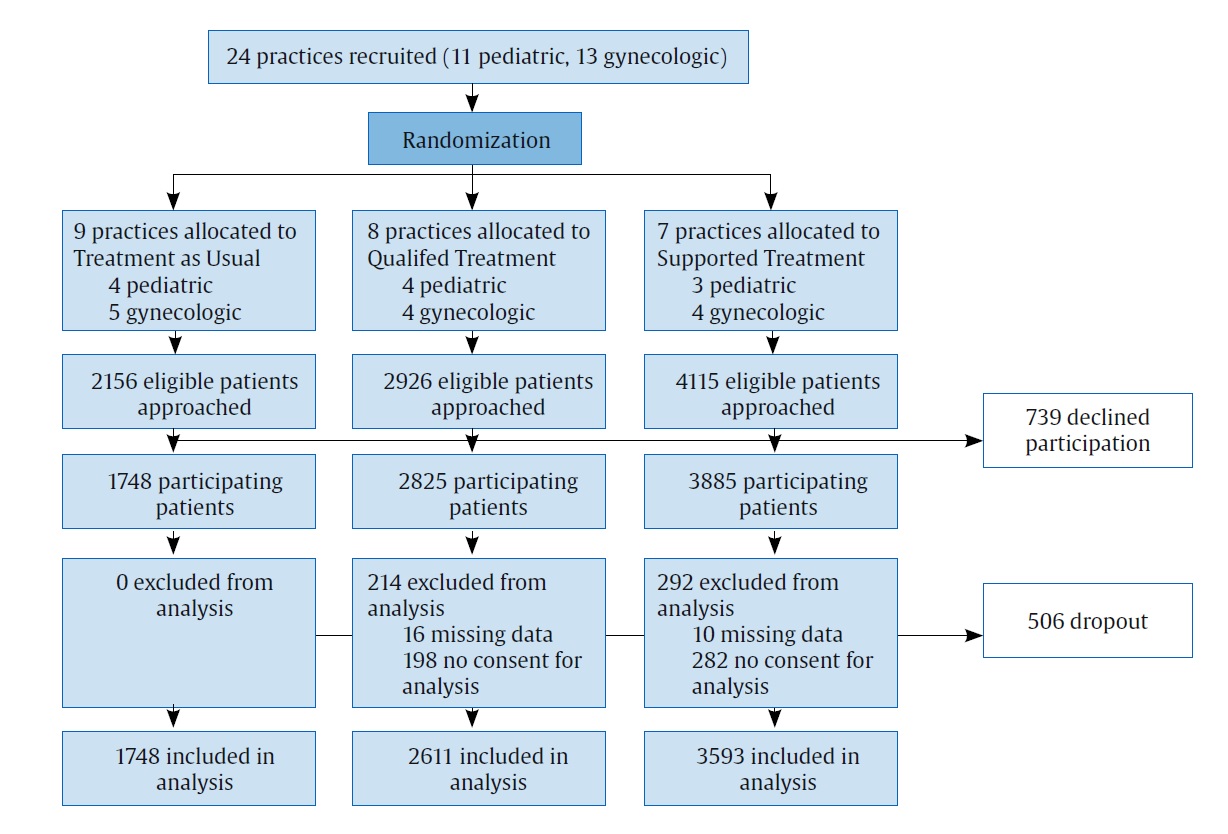
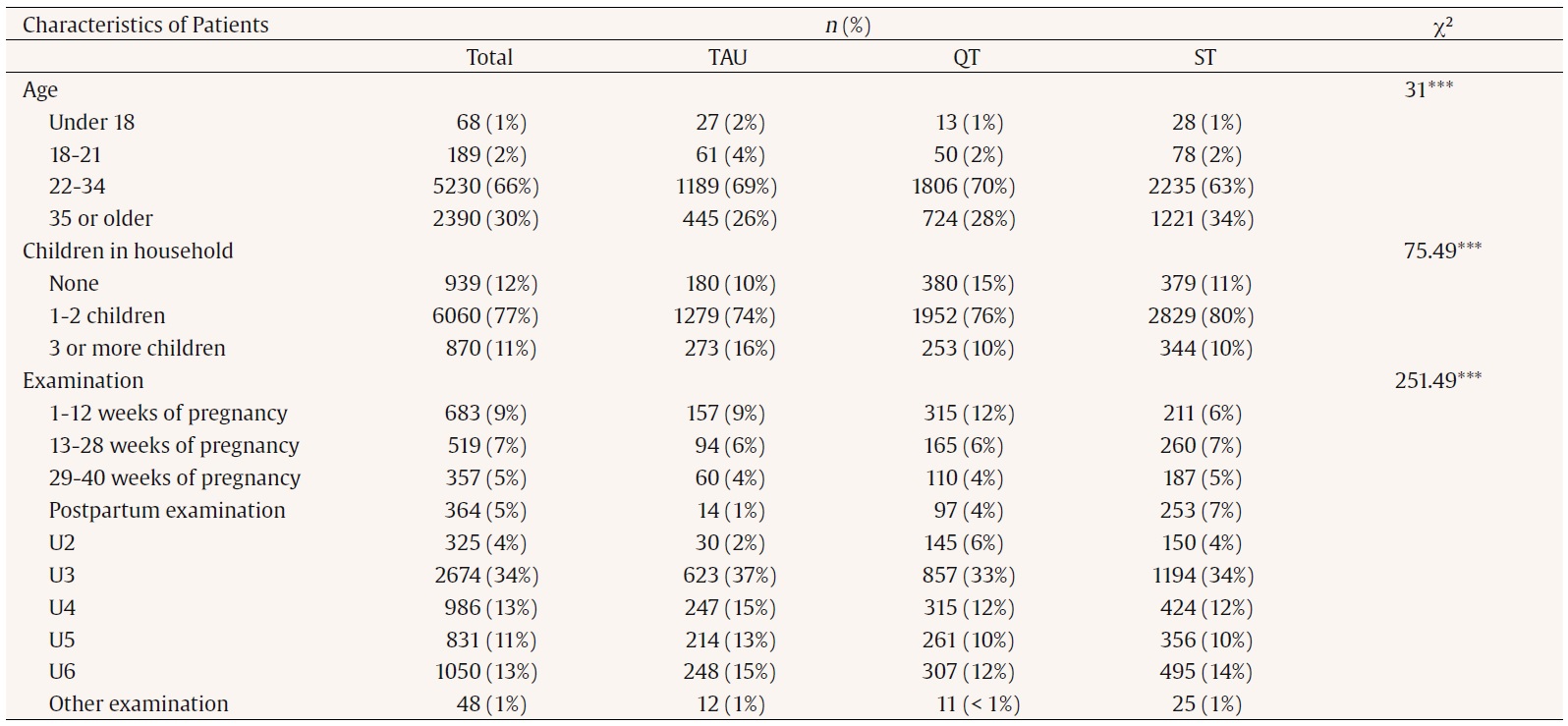
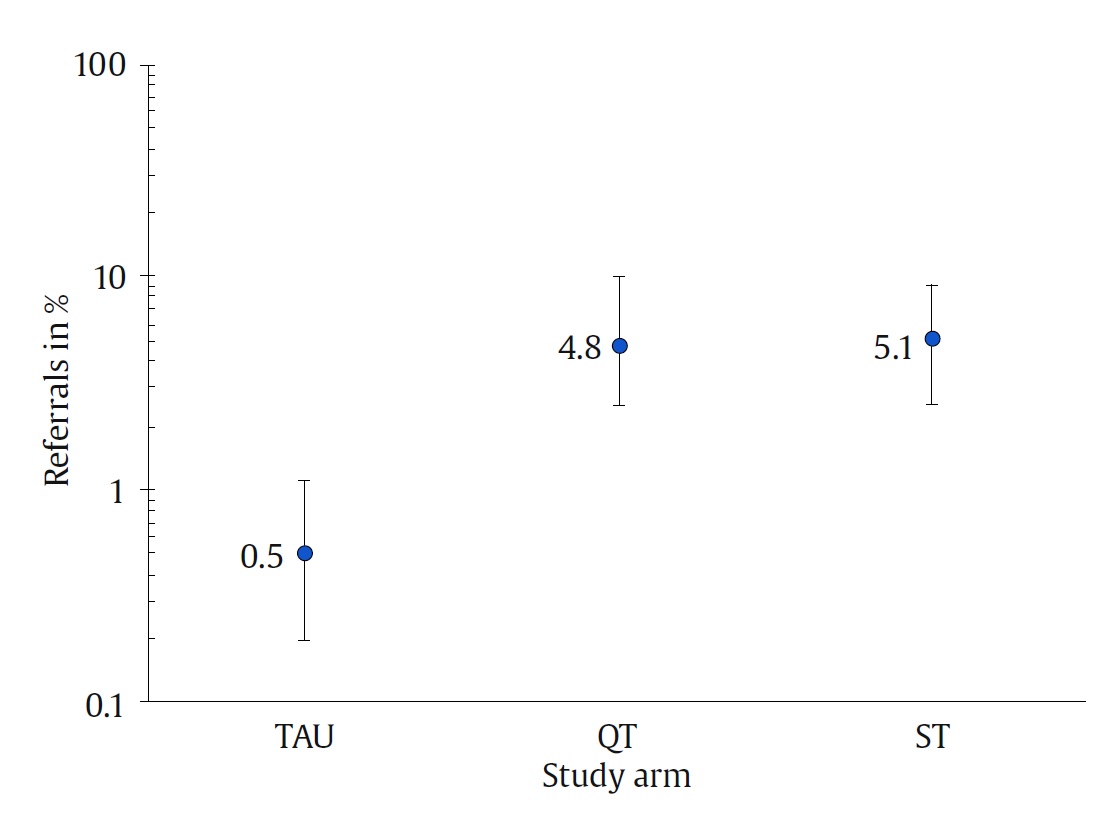
Correspondence: d.kolodziej@uke.de (D. Kolodziej).A broad range of research indicates that many parental psychosocial factors may exert short- and long-term adverse effects on the development and health of children (Buffa et al., 2018; Park et al., 2014; Rakers et al., 2017). Psychosocial stress can be described as an imbalance individuals perceive when the environmental demands exceed their resources to cope with these demands (Wadhwa et al., 2001). Common psychosocial stressors in pregnant women and families with infants include young parental age (Sezgin & Punamaki, 2020), parenting stress (Stone et al., 2016), mental illness (Davalos et al., 2012), drug abuse (Oga et al., 2018), and low socioeconomic status (Reiss et al., 2019). Children of psychosocially stressed families are at higher risk of adverse obstetric outcomes (Buffa et al., 2018; Togher et al., 2017), developmental outcomes (Karam et al., 2016), and behavioural problems (Okano et al., 2019; Rosenqvist et al., 2019), as well as developing mental health diseases later on (Maxwell et al., 2018; Plant et al., 2015). Psychosocial stress during early pregnancy can elevate in later phases of pregnancy and in the postpartum period (Wajid et al., 2020). Newborns and infants are specifically vulnerable as the perinatal period and the first year of life are critical phases for the cognitive, physical, and emotional development (DeSocio, 2018). A German representative study revealed that around 40% of families participating in the child development checks at paediatric practices reported three or more psychosocial stress areas, adverse biographical, prenatal, or perinatal characteristics (Lorenz, Ulrich, Sann, et al., 2020). Reaching parents with psychosocial needs and offering them relevant support and interventions is essential to prevent adverse consequences during child development and to ensure a healthy child development (Ruths et al., 2012). An emerging approach is to address psychosocial needs in paediatric and gynaecologic healthcare settings (Kreuter et al., 2021; McKenney et al., 2018; Pantell et al., 2020). Increasingly, the design and implementation of psychosocial risks screening procedures into these healthcare settings is becoming important (Gottlieb et al., 2016; Kreuter et al., 2021; Metzner et al., 2017). The assessment of the family’s psychosocial situation in healthcare setting, such as obstetric clinics or medical practices, can improve the low threshold access of burdened families to adequate support services and interventions (Mall & Friedmann, 2016) in a non-stigmatizing manner (Kuruvilla et al., 2018; Renner, 2010; Renner, Saint, et al., 2018; Renner, Scharmanski, et al., 2018). As psychosocial risk factors such as socioeconomic factors or mental health issues are highly correlated and often co-occur (Choi et al., 2019; Eick et al., 2020), many instruments for psychosocial stress are based on the cumulation of risk factors (Lorenz, Ulrich, Kindler, et al., 2020). However, the cumulation of risk factors alone does not indicate what kind of support might be needed (Lorenz, Ulrich, Kindler, et al., 2020). Thus, a personal anamnesis by a qualified person is necessary to discuss risk factors and subjective distress experienced by families as well as to identify the specific needs (Metzner & Pawils, 2021). Since parental challenges may differ during a child’s first year of life, a continuous monitoring of the psychosocial situation during pregnancy and in the first year of life is important (Lorenz, Ulrich, Sann, et al., 2020). At present, the regular outpatient healthcare in Germany is supposed to include a social anamnesis during prenatal care check-ups and the well-child-visits. However, there is no standardized instrument for this anamnesis and the implementation including the type of questions, length, and depth may differ between examinations (Neurath & Lohse, 2018). In the last years several projects have emerged that focused on addressing psychosocial risks and needs in pregnant women and families in different healthcare settings. For instance, the project Safe Environment for Every Kid (SEEK) model aimed at the identification of risk factors for child maltreatment in the paediatric and primary care setting (Dubowitz et al., 2012). The model comprised a training of staff, a screening questionnaire for parents, and a social worker who supported and supervised the clinic staff. Compared to a control group, there was significantly less maltreatment in the intervention group (Dubowitz et al., 2009) and mothers reported less psychological aggression and minor physical assaults (Dubowitz et al., 2012). Patient navigation approaches focussing on unmet (social) needs in the paediatric setting have also demonstrated promising findings, such as an increase in referrals, a decrease of social needs, and an improvement of the child’s health (Garg et al., 2015; Gottlieb et al., 2016; Gottlieb et al., 2020; Pantell et al., 2020). In Germany, pilot systems such as the family intervention “Babylotse” (baby pilot) have been established in many obstetric clinics and the gynaecologic and paediatric outpatient setting (Atabaki et al., 2012; Ayerle et al., 2010; Klapp et al., 2019). The evaluation of these approaches indicated a high participation and acceptance in pregnant women and families (Atabaki et al., 2012), reduced maternal depression and stress (Klapp et al., 2019), and an increase in self-efficacy and parental competencies (Ayerle et al., 2010) could also be observed. However, there is little knowledge regarding the efficacy of those approaches compared to the regular healthcare. Since pregnancy routine check-ups and well-child visits are commonly used in Germany, there is a high chance of reaching distressed families in the outpatient care setting (Renner, 2010; Renner, Saint, et al., 2018). Due to their high societal acceptance, healthcare providers such as gynaecologic and paediatric practices provide an ideal access to families at risk (Renner, 2010). We conducted a randomized controlled trial to evaluate a child-centred psychosocial healthcare intervention (KID-PROTEKT) in paediatric and gynaecologic healthcare providers in Germany. The goal of KID-PROTEKT is the promotion of a healthy child development by identifying families with psychosocial risks during routine check-ups and by connecting them to support services. The project also intended to facilitate the participation of families with barriers for participation, such as families with a migration background, psychiatric disorders, and low socioeconomic status. For this purpose, all pregnant women and parents coming to a routine check-up in gynaecologic and paediatric practice were actively addressed in a non-stigmatizing manner. The main components of KID-PROTEKT include a qualification of the medical staff and a psychosocial assessment implemented in the routine pregnancy check-ups (gynaecology) as well as well-child care visits for children in the first year of life (paediatrics).Two versions of KID-PROTEKT were investigated and compared to the regular healthcare treatment as usual (TAU). In Qualified Treatment (QT) the psychosocial assessment and counselling was conducted by the healthcare providers, while in Supported Treatment (ST) a social worker was added to support and supervise healthcare providers. Objectives and Hypothesis The aim of the study was to evaluate KID-PROTEKT as a new child-centred psychosocial healthcare intervention in the outpatient gynaecologic and paediatric setting. The main focus of the study was to evaluate the effectiveness of KID-PROTEKT compared to the regular healthcare. Effectiveness is here referred to as which form of care is most suitable to identify patients with psychosocial stress, as well as to refer and guide them to the help system. We expected that KID-PROTEKT is more effective than usual care in identifying and referring psychosocially stressed patients (TAU). We also assumed that a version in which a social worker is integrated into the practice (ST) will be more effective compared to a model without social worker (QT). Study Design and Setting This study was a multicentre, cluster randomized controlled, three-arm intervention study. The trial was conducted in 24 gynaecologic and paediatric medical practices in the metropolitan area in Hamburg and surrounding rural areas in Schleswig-Holstein and Lower Saxony, Germany. The 24 practices were recruited before the trial started and received a compensation for their participation. Particular structural features of the medical practices, such as size (number of treated patients) and location/catchment area (rural vs. urban), were considered in the recruiting process. The medical practices were categorized as either small or big, depending on the number of patients per year. The cut-off was set as the average number of patients per year of all practices. Table 1 Characteristics of the Participating Practices at the Start of Data-collection (N = 24)   Note.1Size was categorized by the number of treated patients per year in the practice. The cutoff was the average for gynecologic and paediatric practices respectively. The 24 clusters were allocated to one of three study arms, either one version of the child-centred psychosocial healthcare: QT, ST, or the regular healthcare, TAU. The participant flow is illustrated in Figure 1. The N = 24 paediatric and gynaecologic practices were randomly assigned to one of the three study arms stratified according to their location/catchment area and size. This ensured a balanced distribution of rural and urban as well as large and small practices across all study arms. Table 1 shows the result of the randomisation of the 24 medical practices. The majority of the practices (n = 23) were recruited before the trial in 2019, whereas one practice started afterwards and was added to the control group (TAU). Regarding the gynaecologic practices, 13 practices took part in the study (n = 4 QT, n = 4 ST, and n = 5 TAU). Furthermore, 11 paediatric practices were included in the study (n = 3 ST, n = 4 QT, and n = 4 TAU). Among the 24 practices, 11 practices were categorized as large and 13 as small. Regarding the location, 16 practices were located in an urban area and 8 in a rural area. The study was designed based on the ethical guidelines by the World Health Organisation (WHO) and the Medical Association Hamburg. It was approved by the Ethics Committee of the Medical Association Hamburg (PV 6027). Patients and medical staff were informed about the intention of the study. Study Population The study population consisted of pregnant women and women in childbed as well as families with infants (following referred to as patients). Patients were recruited in the gynaecologic and paediatric practices during routine pregnancy check-ups and well-child care visits (German “U-Untersuchungen”). In gynaecologic practices, patients were invited to participate in at least one time point during pregnancy (first trimester, second trimester, third trimester) and during childbed follow-up care (six to eight weeks after birth). In paediatric practices, patients were approached during the regular well-child visits that range from three to ten days postnatal (“U2”), four to five weeks postnatal (“U3”), three to four months postnatal (“U4”), six to seven months postnatal (“U5”) up to the children’s first year of life (“U6”). All patients who took part in at least one screening were included in the study. Families and pregnant women in the condition TAU served as a control group. Child-centred Psychosocial Healthcare (KID-PROTEKT) The key component of KID-PROTEKT is a psychosocial assessment, which is conducted by the health care providers (physicians, nurses, medical assistants) during the routine pregnancy check-ups in gynaecologic practices and the well-child visits in paediatrics. The aim is to identify areas of psychosocial stress in pregnant women and families, clarify the specific needs (psychological, social or medical), and link these patients to appropriate support services (e.g., early child interventions, family counselling, household help). This assessment consists of a screening questionnaire and an orientation interview . Two versions of KID-PROTEKT were implemented and evaluated in gynaecologic and paediatric practices: QT and ST. The two versions were compared to the regular outpatient healthcare (TAU) to investigate which version of KID-PROTEKT is more effective in identifying and referring psychosocially stressed patients to support services. Qualified Treatment (QT) In the study arm QT, medical staff (nurses, medical assistants, and physicians) of the gynaecologic and paediatric practices were trained to conduct the psychosocial assessment. The training (qualification “early childhood interventions in doctor’s practices”) took 20 hours in total and targeted all professional groups (physicians, nurses, medical assistants). It included an introduction into early childhood interventions and psychosocial stress in pregnant women and families. It was discussed how to assess patients’ psychosocial background and specific needs, select fitting support services, and establish referrals. Furthermore, motivational interviewing was practiced. The participants received a certificate and handouts after completing the qualification. During the trial, medical staff conducted the psychosocial assessment without supervision. The staff handed out a screening questionnaire to all patients, who could fill out the questionnaire while waiting for their appointment. If the questionnaire revealed an indication of psychosocial stress, an orientation interview was offered to these patients. The orientation interview was supposed to take place shortly after the screening was filled out, either at the practice location or via telephone. The screening questionnaire provided a basis for the orientation interview, as the stress areas resulting from the questionnaire were discussed with the pregnant woman or family. During the interview, the specific psychosocial risks and needs as well as existing protective factors were assessed. Healthcare providers offered a subjective rating of the patient’s stress intensity and need for support (ranging from no need to very high need for support) and evaluated if a referral to a support service was necessary. Depending on the identified support needs, the staff provided information about support offers, handed out contact information of support offers, or directly linked patients to support services (e.g., contacted institutions for appointments). The medical staff received a list of support services in Hamburg and surrounding areas before the trial. These support services ranged from pregnancy, mother, or family counselling to family interventions, educational guidance, psychotherapy, midwives, support services on financial problems, or household help. The referral was selected during or after the interview, depending on the specific needs and what kind of offers were available in the surroundings of the patient’s location. Supported Treatment (ST) The process in the study arm ST was analogue to QT regarding the training of medical staff and the execution of the psychosocial assessment. Additionally, a social worker (baby pilot) was integrated into the practice, who was present on site (according to prior agreement). The social worker supervised the medical staff regarding the execution of the psychosocial assessment and provided weekly consultation-hours for patients as a support service. If the medical staff recognized patients with complex needs, they could either consult with the social worker to receive supervision and guidance or arrange an appointment for this patient at the counselling hours of the social workers. During their counselling hours, social workers conducted a detailed assessment (clearing interview) of the family situation, psychosocial risk, and protective factors and evaluated the support needs. The case intensity was then divided into one of three categories (consultation, short-term, and intensive cases), depending on a patient’s need for support and required effort tied to the case. Cases of families with complex psychosocial needs that required several referrals and a high effort on the part of the social worker were categorized as intensive cases. After the clarification of patients’ needs, the social workers conducted and evaluated referral to support services. The social worker also provided regular supervision for medical staff regarding their cases of stressed families and was available for questions concerning the network of the regional support system. Treatment as Usual (TAU) In the study-arm TAU patients received the standard healthcare of their gynaecologic or paediatric practice. No changes in the process of the pregnancy check-ups or well-child-visits were made. This study arm did not include any training for medical staff nor a systematic psychosocial assessment. The determination of psychosocial needs and navigation to support services of burdened pregnant women and families depended on the individual experience and approach of the medical staff. Patients’ self-reported psychosocial distress and referrals to support services were only measured for the evaluation. Research Instruments KID-PROTEKT Stress Questionnaire The KID-PROTEKT stress questionnaire was designed as self-report instrument to assess self-reported psychosocial stress of pregnant women and families. The questionnaire was adapted from previous work (Pawils et al., 2022) and modified for this study. For the adaptation of the questionnaire, we consulted women from the target group in the user advisory board of the project. Using a cognitive debriefing, the questionnaire was critically reflected and items accordingly modified. The final questionnaire consisted of 11 items and was translated in seven different languages (English, Turkish, Spanish, French, Russian, Arabic, Farsi). The first three items measured sociodemographic characteristics of the patients, namely the timing of examination (pregnancy week or well-child-visit), age in categories (e.g., 18 to 21), and the number of children in the household in categories (e.g., 1-2 children). The remaining eight items assessed empirically based psychosocial risk factors for early child development and served as screening to provide indications of psychosocial stress. These items could be answered with either “yes” or “no”. It was assessed whether the patient was a single parent and feelings of depression, tiredness, loss of energy/joy, or having experienced something distressing were examined. The other items explored psychosocial stress factors in global categories and patients should indicate if they felt stressed in this particular area: (a) coping with everyday life, (b) relationship, (c) life situation, (d) pregnancy and birth, (e) children and education, (f) other stress factors. If at least one of the eight screening questions or an age younger than 21 was answered with yes, the screening was classified as positive and an orientation interview was initiated. Documentation of the Orientation Interview For the documentation of the orientation interview conducted by medical staff a semi-structured documentation sheet was developed in order to record the basic features of the interview, such as date, duration, where it took place (practice or telephone), and who conducted the interview (nurse/medical assistant or physician). Furthermore, the reason for the interview was documented (e.g., positive screening result). The topics discussed during the interview were recorded in the same categories as in the screening questionnaire (e.g., stress regarding relationship, life situation). Then the staff rated patients’ level of distress on a scale from “very high” to “very low” and whether the patients had a need for support. Finally, it was recorded whether the patient was referred to support services. The type of referral (recommendation of a support service or direct referral, such as making an appointment) and the institutions that patients were referred to were registered. Also, it was noted if patients were not referred to any service and the reason for this (e.g., family is already connected to support services). Implementation and Quality Management For the purpose of quality management, a scientific advisory board was employed in the project to discuss and evaluate deviations from the planned application as well as their influences on the results. The scientific advisory board consisted of experts from science, the social, child and youth welfare, health insurances, and other stakeholders. Furthermore, a user advisory board was set up, consisting of members of the target group who advised on questions of planning, implementation, and evaluation of measures from the patient perspective. Members of the user advisory board were former patients of the family intervention “Babylotse Hamburg” (Pawils et al., 2022). The user advisory board was anchored in the project structure and was involved in decision-making processes regarding the design of workflow and study materials. Before starting the actual data collection, the work flow was tested in an implementation phase for one month from July to August 2019 in all practices. The workflow was discussed with the practice team and specific processes per practice were defined and documented. Data collection was managed by the research team of the University Medical Centre Hamburg Eppendorf. During data collection, a study nurse visited the participating practices every week, picked up collected data, and carried out data quality checks. The study nurse also acted as a contact person for the medical staff regarding questions on the study. Data Collection Qualified Treatment and Supported Treatment Patients with an appointment for a routine pregnancy check-up (during first, second, or third trimester, or during childbed) or a well-child visit (German well-child-visits U2, U3, U4, U5, or U6) were informed about the project and asked if they would like to participate. They were asked to fill out the self-rating screening on psychosocial stress while waiting for their appointment. If they declined to fill out the questionnaire, the medical staff asked for the reason and documented it on a non-participation card. The card was thrown into a special letterbox for the study. The letterbox was locked and not accessible to the medical staff of the practice. Data collected in the letterbox was picked up by the study nurse weekly and delivered to the research group. After filling out screening, patients gave it back to the staff who evaluated it. If the screening did not show any indication of psychosocial stress, the questionnaire was returned to the patient, who had the option of passing it on to the research team for evaluation purposes. Patients were informed about the scientific evaluation of their information in the questionnaire if they put it into the letterbox. If the questionnaire revealed psychosocial risk factors, patients were invited to an orientation interview by the medical staff. The orientation interview took place either in the practice or via telephone and was documented by the medical staff using the documentation form. After completing the orientation interview, patients were informed by medical staff about the possibility to participate in KID_PROTEKT evaluation study. Herefore, patients received a study information sheet and a consent form in duplicate. If patients gave their consent to participate, all relevant data (screening questionnaire, documentation of orientation interview) were placed into the letterbox. The process of data collection in the study arm ST was analogous to QT. Both study arms were only differing in the opportunity to refer patients to the counselling hours of the social worker (ST). If patients agreed to being referred to the social worker, the medical staff faxed the patient’s contact information to the social worker or directly made an appointment for the patient. The social worker then took the case and cared for the family until case closure. Treatment as Usual As in QT and ST, patients in TAU were approached before an appointment for a pregnancy check-up or well-child care visit and invited to fill out the screening questionnaire in the waiting room before the appointment. They were informed about the evaluation study and received a study information sheet with a consent form. After filling out the questionnaire and consent form, patients were asked to put them into the letterbox. The medical staff was not supposed to look at or evaluate the questionnaire. There was no further intervention in this study arm. If physicians identified patients with psychosocial needs and linked them to support services, the staff documented the patient ID and the recommended support service or institution on a documentation sheet. Telephone Interviews To investigate the utilization rate of external support services, telephone interviews were conducted. All patients who received a referral during the psychosocial assessment and consented into a telephone interview were questioned. Additionally, in TAU all patients with psychosocial stress who agreed to the interview were questioned. During the interview, patients were asked whether they used the support services and whether they were satisfied with the recommended services. The interviews were conducted by the research team. Data Analysis All data were entered into the programme SPSS (Version 25) for the use of statistical analysis. The number of psychosocial risks was calculated by adding the items of the screening questionnaires that were answered with “yes”. Missing items were not imputed. Questionnaires with more than three missing items were excluded from data-analysis. The degree of support needs based on the subjective rating of medical staff during the orientation interview was categorised as either intensive needs (very high up to middle needs) or no/low needs (low up to no needs). Regarding the descriptive analysis, for categorical variables proportions and for metrical variables means were used. In order to test for differences between study arms, chi-square tests were applied for categorical variables and analysis of variance (ANOVA) for metrical variables. For the statistical assessment of the main effect we used a generalized mixed logistic regression. The mixed logistic regression was chosen to consider the hierarchical structure of the data from practices and patients and to enable the estimation of the intervention effect even in the presence of missing values. We carried out the mixed logistic regression model for the main outcome referral to support system (yes/no). For this purpose, we calculated a variable indicating whether or not a patient was linked to a support service based on the documentations made by the practices. The dependent variable was the main outcome referral to support service (yes/no). As fixed effect, the study arm and the number of psychosocial stress factors of the first questionnaire were added to the model. The cluster structure (study-ID of each practice) was taken into account in the model. As random effect, we included a random intercept (practice) into the model. The utilization of referred support services by families (yes/no) was tested by a chi-square test. Sample Recruitment and Demographics Twenty-four gynaecologic and paediatric practices took part in the study and were randomized to one of the three study arms. In total 9,197 pregnant women and families were invited to participate in one of the 24 practices during the phase of data collection. Of these patients, 8,458 pregnant women and families were enrolled in the study and participated in at least one psychosocial screening in their gynaecologic or paediatric practice and 739 refused to participate (see Figure 1). The reason for refusal was mostly no interest/no necessity (n = 401, 60%). Other reasons were language barriers (n = 125, 18%) or that the questionnaire was considered as too personal (n = 67, 10%). The total sample consisted of 2,158 patients (26%) recruited in the gynaecologic practices and 6,300 (74%) in paediatric practices. The participation rate was 92% over all study arms, 97% for QT, 94% for ST, and 81% for TAU. In total 506 patients in the study arms QT and ST had to be excluded from the analysis due to either missing data or missing consent for further analysis. Among the final sample consisting of 7,952 patients (see Table 2), most patients were between 22 and 34 years old (66%) or at least 35 years old (30%). Only few patients were younger than 18 (1%) or between 18 and 21 years old (2%). The majority of patients reported that at least one or two children (77%) were living in their household, 12% of patients had no child. The highest proportion of patients entered the study during the U3 examination (34%) and the lowest proportion during the U2 examination (4%) and other examinations (1%) . There were a few differences between the study arms regarding the variables age χ2 = 74.31, p < . 001, number of children in household χ2 = 75.49, p < . 001, and the timepoint of examination, χ2 = 251.49, p < . 001. However, these associations were small (Cramer V = .07, .07, and .13 respectively). More patients in QT were enrolled during one to 12 weeks of pregnancy (12%) than in TAU and ST, while in TAU (1%) fewer patients were enrolled after birth than in QT and ST. ST included more patients of age 35 or older (34%) than in QT (28%) and TAU (26%). Compared to QT and ST, there were more patients with three or more children in TAU (16%). There were some minor significant differences between patients who were included in the analysis and patients who were excluded regarding age, χ2 = 9.49, p = .023, Cramer V = .34 and number of children in household, χ2 (2) = 7.15, p = .028, Cramer V = .03. Results of the Psychosocial Assessment The number of reported psychosocial risks ranged from zero to eight stressors. In total 2,598 patients (33%) reported at least one stress area in the screening questionnaire. These 2,598 patients reported on average 1,73 (SD = 1.34) stressors across all three study arms (see Table 3). The most common stressor among all study arms was depressive symptoms/having experienced something distressing (46%), while the least common stressors were young parental age (3%) and relationship related problems (9%). Other frequently recorded stressors were feeling stressed regarding the life situation (22%) as well as regarding pregnancy and birth (21%). Table 3 Results of the Psychosocial Assessment and Referral Rate (N = 7,952)  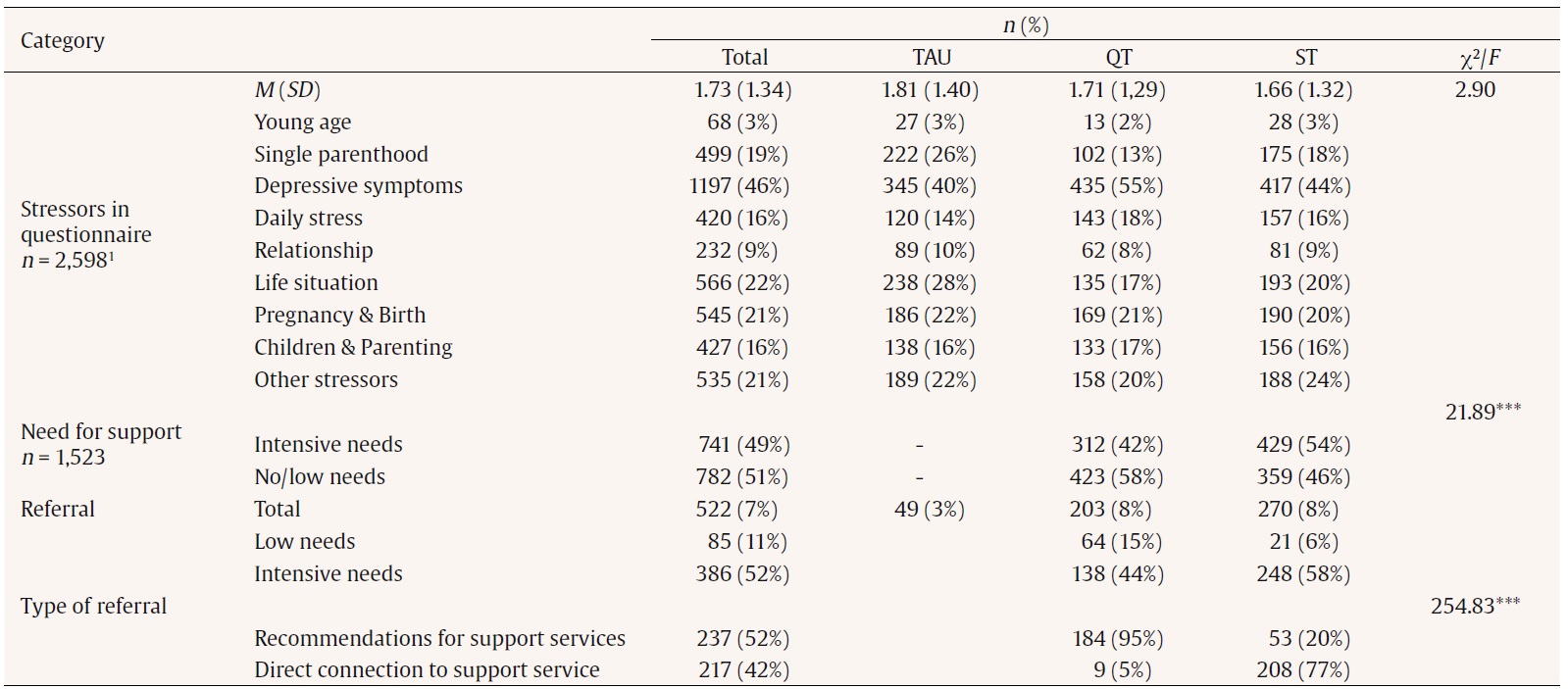 Note. 1Frequencies and proportions related to first screening questionnaire, mean over stressed patients in the first questionnaire. ***p < .001 In the two intervention arms (QT and ST) 1,530 patients received an orientation interview. Following with the orientation interview, the medical staff rated the patient’s need for support, which was then either categorized as intensive needs (middle to very high need for support) or low needs (no or low need for support). In ST the frequency of patients with intensive needs was higher than in QT (54% vs. 42%), χ2 (1) = 21.89, p < .001, ϕ = .12. Additionally in ST, 200 cases were handled by the social workers who contacted families to discuss their needs in an interview. Altogether social workers conducted interviews with and supported 176 families. Referrals to Support Services Among patients with psychosocial needs, 25% in QT, 28% in ST and 3% in TAU were referred to a support offer. Additionally, 28 patients were referred although the screening did not indicate psychosocial needs (e.g., because patients asked for support). Thus, in total, n = 522 (7%) of all 7,952 included patients were linked to a support service. In both intervention study arms QT and ST, the referral rate among all patients was 8%, whereas in the control condition TAU it was 3%. The proportion of referred patients with intensive support needs was higher in ST (58%) than in QT (44%). When considering the type of referral (recommendation of support offers vs. directly connecting patients), there was a significant difference regarding the study arms, χ2 (1) = 254.83, p < .001, ϕ = .75, as in ST more families received at least one direct connection to support services by the practices (77%) than in QT (5%). In ST most referrals occurred to the social workers (baby pilots). Other frequent support services were family counselling, therapeutic offers (e.g., psychiatric clinic), general counselling services, and financial or employment counselling (e.g., debt counselling). In QT most referrals were to the family counselling, childcare, or parent-child offers, pregnancy or mother counselling, educational guidance, and child- and family help centres. In TAU most referrals comprised an App on birth and the first year of life, mother counselling, childcare, parent-child offers, early childhood interventions and youth welfare services. The logistic mixed regression model (ICC = .38) revealed that the number of psychosocial stressors had the largest effect on the probability of a referral, F(1, 7948) = 758.46, p <. 001, n = 7,948. The study arm had a significant effect on the chance of being referred as well, F(2, 7948) = 12.41 , p < .001 , n = 7,948. QT differed significantly from TAU (t = 4.15, p < .001). Thus, the probability of a patient to be referred to a support service is 10.70-times higher (95% CI [3.74, 30.64]) for patients in QT compared to TAU. The difference between ST and TAU was significant as well (t = 4.41, p < .001). Thus, the probability of a referral is 11.28-times higher (95% CI [3.84, 33.10]) in ST than in TAU. The number of stressors was also significant (t = 27.54, p < .001) and the probability of a referral increases by 2.72 times for every additional stress area (95% CI [2.54, 2.93]). The mean of the random effect was 0.86 (95% CI [0.41, 1.81]; p <. 01), indicating that practice as cluster-structure had to be controlled for in the model. The marginal means of each study arm are displayed in Figure 2, showing the proportion of each study arm regarding the referrals. The referral proportions of both intervention study arms QT (M = 0.05, 95 % CI [0.03, 0.09]) and ST (M = 0.05, 95% CI [0.03, 0.10]) were higher than the regular care TAU (M = 0.01, 95% CI [0.00, 0.01]). Utilization of Support Services A sample of 133 patients with a referral was contacted by telephone, of which 26% utilized the recommended support services and 71% did not. The highest utilization rate was found in ST (35%), whereas the utilization rate in QT was 18% and 15% in TAU. Among patients with intensive needs, the utilization rate was higher in ST (34%) than in QT (12%). The chi-square test did not reveal a significant association between utilization of the referred services and study arm, χ2(2) = 5.19, p = .75. A post hoc power analysis was executed using the program G*Power. Consequently, the calculated power was .53 under consideration of a significance level of .05 and an estimated effect size of .20, meaning that possible differences could be detected by a probability of 53%. Psychosocial stress during pregnancy and the first years of life can lower the quality of life and have adverse consequences on the health and development of children (Mall & Friedmann, 2016). Therefore, psychosocial stress should be identified early on and support offers should be provided. The gynaecologic and paediatric healthcare represents an accepted setting to address psychosocial needs and provide counselling regarding support services (Renner, 2010; Sprecher et al., 2018; Yee et al., 2017). A tailored assessment of the psychosocial situation and the individual needs is necessary to refer patients with psychosocial stress to adequate social, psychological, medical healthcare, or other support services. Approaching pregnant women and families in healthcare settings provides the possibility to overcome barriers and link patients with support needs to the right support services (Sprecher et al., 2018; Yee et al., 2017). Previous studies have shown the advantage of interventions that address psychosocial needs in healthcare settings to link patients to the appropriate social, psychological and medical healthcare interventions (Dubowitz et al., 2012; Messmer et al., 2020; Pantell et al., 2020). We evaluated a new form of a child-centred psychosocial healthcare intervention in the outpatient setting in order to identify patients with psychosocial needs and to guide them to the appropriate support services. The evaluation of KID-PROTEKT was executed as a cluster randomized controlled trial conducted in 24 practices (13 gynaecologic and 11 paediatric practices) in Hamburg, Lower-Saxony, and Schleswig-Holstein. In both versions of KID-PROTEKT, QT, and ST, the medical staff (nurses, medical assistants, and physicians) were trained to assess psychosocial risks in a two-step assessment, consisting of a self-report screening questionnaire and a personal orientation interview. The focus of this psychosocial assessment was to address the specific needs of the family and to find the right social, psychological, or medical healthcare interventions for stressed families (e.g., early child intervention, child and youth welfare, psychotherapy). Additionally, in ST a social worker was integrated into the practice. During the 18 months of data-collection, 9,197 families were approached in the gynaecologic and paediatric practices. Due to the low-threshold service in the practice and the shortness of the screening, there was a high participation rate, which was probably facilitated by the procedure of obtaining the informed consent after the orientation interview was conducted. Of all families, 33% reported at least one psychosocial risk, the most common risk factors being depressive symptoms/having experienced something distressing (46%), feeling distressed regarding the life situation (22%), or pregnancy and birth (21%). Families who did not participate in the screening and were not reached by the intervention mostly reported as reason no necessity for participation. Other reasons for non-participation were language barriers or perceiving the psychosocial assessment as too personal; 1,530 patients in QT and ST received an orientation interview. The orientation interview between the medical staff and patients is a key component of KID-PROTEKT that aims at specifying the assessed risks and needs, identify potential protective factors or an existing support network, and to evaluate the families need for support and discuss appropriate interventions. A screening does not replace the expertise of qualified staff (Mall & Friedmann, 2016), but provides a starting point for further diagnostics. Thus, a personal interview with parents is required to clarify the specific needs of the family (Metzner & Pawils, 2021). In ST the staff could approach the social workers for either consultation regarding a case or send families to the counselling hours provided by the social workers in the practice. The social workers took over the cases of 176 families after the orientation interview with the staff. The referral rate across all patients was higher in KID-PROTEKT (both QT and ST 8%) than in TAU (3%). Patients in both intervention study arms were much more likely to be referred than in TAU (QT: OR = 10.70, ST: OR = 11.28). In fact, it was also shown that the number of psychosocial stressors was associated to referrals. A higher number of psychosocial stressors was related to an increased probability for a referral. Patients with intensive psychosocial needs showed a higher referral rate in ST (57%) than in QT (44%). In QT, patients mostly received recommendations and contact information for possible support services (95%), while in ST more patients were directly linked to at least one support service (77%). Thus, although the referral rates were similar in QT and ST, the type of referral differed between the two versions of KID-PROTEKT. The utilization of support services was tested in a subgroup of referred patients, who consented to the telephone interview. The highest utilization rate was found in ST (33%), followed by QT (18%), while it was lowest in TAU (15%). In ST, more patients received direct referrals (e.g., support services were contacted before and, where appropriate, an appointment was made) compared to QT that were possibly more binding than giving recommendations and information about services. The integrated social worker in ST had experience with the regional psychosocial support system and was aware of available support offers, which also could have helped with the selection of referrals. However, these descriptive differences regarding the utilization rate were not statistically significant, which is probably due to the low sample size. Furthermore, it has to be taken into account that the study was conducted during the COVID-19 pandemic, during which many support services were not available or highly restricted. Due to these restrictions, the utilization of support services was probably hindered. Since the utilization of support services remains a challenge in healthcare, future research should focus on barriers and facilitators for the utilization of help. This is the first study in German healthcare research examining a new psychosocial healthcare intervention in contrast to the regular healthcare using a cluster randomized controlled trial. The results of the KID-PROTEKT evaluation indicate that a psychosocial assessment by the medical staff leads to a better identification of pregnant women and families with psychosocial needs and referral to support services. In TAU, which represented the regular healthcare, there was no systematic psychosocial assessment and referrals were less likely. In the current regular gynaecologic and paediatric outpatient healthcare, psychosocial needs are not regularly discussed. Recommendations for and direct connections to support services occur only on irregular basis and the utilization of these services is not evaluated systematically by the practices. Even though physicians who took part in this study probably embraced psychosocial counselling in healthcare, the referral rate was considerably lower compared to KID-PROTEKT. Several limitations should be mentioned. The study was designed as a naturalistic study to enable the utilization of the intervention independent of study participation. Therefore, informed consent was obtained after the orientation interview. Due to this approach, we had to reduce the sociodemographic questions to a minimum and assess all variables in the screening questionnaire in categories. Thus, only a few sociodemographic characteristics of the sample are known and the psychosocial risks were recorded in broad categories. A further limitation is that the psychosocial stress assessment in TAU was only based on the screening questionnaire, while in QT and ST the stress degree was also evaluated by medical staff based on the orientation interview. For this reason, we could not consider the intensity of psychosocial needs in the statistical analysis across all study arms. Furthermore, during data collection it became evident that the documentation of referrals in TAU by the physicians was inadequate despite regular reminders and monetary compensation for study participation. Thus, to validate the referrals in TAU, patients who gave their consent and contact information were contacted by phone and asked about whether they were referred to a support service. The utilization of support services was investigated in a sub-sample of patients who were interviewed via telephone whether they went to the referred services. However, a post hoc power analysis indicated that the yielded sample was too small to uncover any significant differences. Importantly, it should be noted that the project was mainly conducted during the COVID-19 pandemic, which resulted in many restrictions in the provision of healthcare, social, and psychological services. Consequently, the utilization of the support services by families remains a topic for further research. The randomization of practices was conducted under consideration of different structural features such as size and location/catchment. Other characteristics such as the socioeconomic distribution of the district in which a practice was located could not be taken into account. However, in the statistical analysis of the main outcome the practice was controlled for as a random effect. Therefore, the results of this study can be generalized to the gynaecologic and paediatric healthcare in Germany. Conclusions To connect the psychosocially stressed families to the right support services, a systematic psychosocial assessment is needed to address psychosocial stress on a low-threshold and to guide patients in the complex healthcare and social welfare system. The offer of a child-centred psychosocial healthcare in gynaecologic as well as paediatric practices appears to be a promising approach to reach families with psychosocial needs. As a result, patients who are exposed to psychosocial stress are advised on services from the existing regional support systems and are referred to suitable support services such as early child interventions at an earlier stage in a more binding and sustainable manner. From the providers perspective, improved access management can also contribute to an improvement in the patient-oriented endpoints of care. Given the already existing standard care structures – pregnancy and paediatric check-ups – the obstacles to establishing these services are a clear definition of “best practice”, qualification opportunities for staff, and sufficient funding. KID-PROTEKT provides defined processes for a psychosocial assessment and navigation of families, a curricular for training of staff, and the standardized implementation of social workers. The results of this evaluation study highlight the need for the implementation of a routine psychosocial assessment and into the regular gynaecologic and paediatric healthcare to identify families with psychosocial needs and provide them with fitting support offers. The psychosocial assessment, consisting of the screening, interview, and counselling of parents, can be performed by qualified medical staff. For patients with several and complex psychosocial needs, a social worker or special patient navigator is required to connect these patients directly to adequate social, psychological, or medical healthcare interventions and monitor the utilization of these support offers. Finally, addressing psychosocial needs in the gynaecologic and paediatric setting is feasible and important to improve the healthcare of stressed families. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgements We would like to thank SeeYou Foundation, specifically Nikola Nitzschke. We also thank the medical staff of the 24 participating gynaecologic and paediatric practices for carrying out the study. Cite this article as: Kolodziej, D., Wolkwitz, P., Schön, G., Siefert, S., & Pawils, S. (2023). Evaluation of a child-centred psychosocial healthcare intervention (KID-PROTEKT) – Results of a cluster randomized controlled trial in paediatric and gynaecologic practices Psychosocial Intervention. Psychosocial Intervention, 32(1), 33-42. https://doi.org/10.5093/pi2023a2 |
Cite this article as: Kolodziej, D., Wolkwitz, P., Schön, G., Siefert, S., & Pawils, S. (2023). Evaluation of a Child-centred Psychosocial Healthcare Intervention (KIDPROTEKT) – Results of a Cluster Randomized Controlled Trial in Paediatric and Gynaecologic Practices. Psychosocial Intervention, 32(1), 33 - 42. https://doi.org/10.5093/pi2023a2
Correspondence: d.kolodziej@uke.de (D. Kolodziej).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS