
Special Issue: Treatment Resistant Perpetrators of Intimate Partner Violence: Research Advances
Randomized Clinical Trial of a Brief Alcohol Intervention as an Adjunct to Batterer Intervention for Women Arrested for Domestic Violence
[Ensayo clÃnico aleatorizado de una intervención breve para el consumo de alcohol como complemento a la intervención con mujeres agresoras detenidas por violencia doméstica]
Meagan J. Brem1, Ryan C. Shorey2, Susan E. Ramsey3, and Gregory L. Stuart4
1Virginia Polytechnic Institute and State University, Backsburg, USA; 2University of Wisconsin-Milwaukee, USA; 3Alpert Medical School of Brown University and Rhode Island Hospital, Providence, USA; 4University of Tennessee-Knoxville, USA
https://doi.org/10.5093/pi2023a4
Received 6 September 2022, Accepted 10 January 2023
Abstract
Despite a rise in women being arrested for domestic violence and court-ordered to batterer intervention, batterer interventions remain limited in their ability to address women’s treatment needs. Alcohol use is an important intervention target: one-third of women in batterer interventions have an alcohol-related diagnosis, half engage in at-risk drinking, and alcohol use contributes to intimate partner violence (IPV) and batterer intervention dropout. Research has not evaluated whether adding an alcohol intervention to batterer intervention improves women’s alcohol use and IPV outcomes. We randomized 209 women (79.9% white) in Rhode Island to receive the state-mandated batterer intervention program alone or the batterer intervention program plus a brief alcohol intervention. Alcohol use (percentage of days abstinent from alcohol [PDAA], number of drinks per drinking day [DPDD], percentage of heavy drinking days [PHDD], percentage of days abstinent from alcohol and drugs [PDAAD]), and IPV perpetration and victimization frequency (psychological, physical, and sexual IPV, injury) data were collected at baseline and 3-, 6-, and 12-month follow-up. Multilevel modeling revealed that, relative to the batterer intervention alone, women who received the brief alcohol intervention reported a higher PDAA and PDAAD, fewer DPDD, and a lower PHDD across all follow-up assessments. Women who received the brief alcohol intervention perpetrated less physical IPV and experienced less injury than did women who only received the batterer intervention. For physical IPV, these differences became more pronounced over time. No other group differences or group x time interactions emerged. Adding an alcohol intervention may improve batterer intervention outcomes for women arrested for domestic violence.
Resumen
Aunque haya aumentado el número de mujeres detenidas por violencia doméstica remitidas a programas de intervención, los programas de intervención para agresores siguen estando limitados en cuanto a su capacidad para cubrir las necesidades de tratamiento de las mujeres. El consumo de alcohol es un objetivo de intervención importante: un tercio de las mujeres en intervención para maltratadores tienen diagnósticos relacionados con el alcohol, la mitad presentan consumo de alcohol de alto riesgo y el consumo de alcohol contribuye a la violencia de pareja (VP) y al abandono de la intervención para maltratadores. No se ha investigado si añadiendo una intervención para el consumo de alcohol a la intervención con maltratadores se reduce dicho consumo y la VP en mujeres. Aleatorizamos una muestra de 209 mujeres (79.9%) en Rhode Island para que recibieran solo el programa de intervención estándar previsto o acompañado de una intervención breve en alcohol. Se recogieron los datos de línea base sobre consumo de alcohol (porcentaje de días de abstinencia [PDAA], número de bebidas por día en el que se consume [VBD], porcentaje de días en que se bebe con intensidad [DBI], porcentaje de días de abstinencia de alcohol y drogas [DAAD]), y frecuencia de la perpetración y victimización de la violencia de pareja (VP psicológica, física y sexual, lesiones) y se realizó seguimiento de 3, 6 y 12 meses. Mediante un modelo multinivel se mostró que, en comparación con las mujeres que participaron en la condición control, aquellas que recibieron la intervención breve para el consumo de alcohol presentaron mayor PDAA y DAAD y menor VBD y DBI en todas las evaluaciones de seguimiento. Las mujeres que recibieron la intervención breve para el consumo de alcohol perpetraron menos VP física e informaron de menos lesiones que las que solo habían recibido intervención para maltradores. Estas diferencias se hicieron más pronunciadas con el tiempo para la VP física. No se encontraron otras diferencias entre ambos grupos o interacciones grupo x tiempo. Añadir una intervención para el consumo de alcohol puede mejorar los resultados de la intervención con mujeres agresoras detenidas por violencia doméstica.
Keywords
Women, Batterer intervention, Alcohol intervention, Domestic violence, Intimate, Partner, Violence, PerpetrationPalabras clave
Mujeres, Intervención con agresores, Intervención en el consumo de alcohol, Violencia doméstica, Perpetración de violencia de parejaCite this article as: Brem, M. J., Shorey, R. C., Ramsey, S. E., & Stuart, G. L. (2023). Randomized Clinical Trial of a Brief Alcohol Intervention as an Adjunct to Batterer Intervention for Women Arrested for Domestic Violence. Psychosocial Intervention, 32(2), 79 - 88. https://doi.org/10.5093/pi2023a4
Correspondence: gstuart@utk.edu (G.L. Stuart).The past 30 years witnessed a rise in the number of women arrested for domestic violence following implementation of mandatory arrest policies (Chesney-Lind, 2002; Durfee, 2012; Henning et al., 2006). Women represent as many as 31% of all domestic violence arrests in some jurisdictions which has contributed to their increasing visibility in batterer intervention programs (Hamel et al., 2017; Hirschel & Buzawa, 2002; Solinas-Saunders & Stacer, 2022). Women now comprise up to 25% of batterer intervention program participants, with comparable or more frequent psychological and physical intimate partner violence (IPV) perpetration being reported by women relative to men enrolled in batterer interventions (Busch & Rosenberg, 2004; Buttell et al., 2012; Dalton, 2007; Elmquist et al., 2014; Feder & Henning, 2005; Hamel et al., 2017). Women who perpetrate IPV also experience frequent IPV victimization, with data largely supporting that IPV is bidirectional (Langhinrichsen-Rohling et al., 2012; Stuart et al., 2006; Stuart, Moore, et al., 2003; Stuart et al., 2004). Problematically, batterer intervention programs are only minimally effective in reducing violence recidivism, with even less support for the efficacy of court-mandated programs in reducing women’s IPV (Babcock et al., 2016; Babcock et al., 2004). The deleterious consequences of IPV experienced by women’s partners (e.g., posttraumatic stress symptoms, depression, suicidality, and severe injury), the risk IPV perpetration poses for women’s victimization, and the economic burden of IPV-related expenses (e.g., health care and criminal justice costs) underscore the need for efficacious programs that prevent women’s violence recidivism (Bonomi et al., 2009; Gerstenberger et al., 2019; Hines & Douglas, 2011; Leisring et al., 2003; Machado et al., 2020; Peterson et al., 2018; Stuart et al., 2004). The present study proposed that targeting alcohol use concurrently with batterer intervention programming may improve alcohol and IPV outcomes among women court-mandated to batterer intervention. Theory and extensive empirical data indicate that alcohol use and alcohol-related problems are distally and proximally related to IPV among men and women (Foran & O’Leary, 2008; Leonard & Quigley, 2017). Conceptual models of IPV (e.g., Finkel & Eckhardt, 2013; Leonard, 1993, 2001; Stuart et al., 2006) suggest that distal characteristics (e.g., aggressogenic traits, the couple’s maladaptive communication patterns) interact with proximal factors (e.g., the pharmacological effects of acute alcohol intoxication) to strengthen the likelihood of IPV perpetration. Consistent with these theoretical frameworks, one-third of women in batterer intervention programs have an alcohol-related diagnosis (Stuart, Moore, et al., 2003), half met criteria for hazardous or at-risk drinking (Stuart, Moore, et al., 2003; Stuart et al., 2004), and women arrested for domestic violence who were hazardous drinkers perpetrated physical, psychological, and sexual IPV more frequently, caused more injuries to their partner, and experienced physical IPV victimization more frequently than did non-hazardous-drinking women (Stuart, Moore, et al., 2003; Stuart et al., 2004). Even after accounting for other factors (e.g., antisociality, relationship discord, and their partner’s alcohol problems and IPV perpetration), alcohol use and problems were positively related to IPV perpetration among women arrested for domestic violence (Stuart et al., 2006) and associated with a 2.5-fold increase in risk of severe (relative to mild) female-to-male IPV (McKinney et al., 2010). In a subset of women who participated in the present study, timeline follow-back interview data revealed that physical IPV perpetration and victimization reported at baseline were more likely to occur on a drinking day and on a heavy drinking day relative to a non-drinking day (Stuart et al., 2013). Similarly, 53.1% of women arrested for felony domestic violence were under the influence of alcohol or drugs at the time of the offense (Friend et al., 2011). Given the overrepresentation of alcohol use among women arrested for domestic violence and the distal and proximal associations between alcohol use and women’s severe IPV, it is not surprising that calls for targeting women’s alcohol use in batterer interventions have emerged (e.g., Babcock et al., 2016; Langenderfer, 2013; Stuart et al., 2006; Stuart et al., 2007). Treating alcohol use and other substance use disorders corresponds with reductions in IPV perpetration among clinical populations of men and women in substance use treatment (Easton et al., 2007; Easton & Sinha, 2002; Klosterman et al., 2011; O’Farrell et al. 2004; O’Farrell et al., 1999; Schumm et al., 2009; Stuart et al., 2002; Stuart, Ramsey, et al., 2003; Stuart et al., 2013). However, these programs were designed to treat [primarily men’s] substance use as the primary focus and IPV as a secondary focus; no study examined the effect of such interventions on IPV perpetration and alcohol use among women in batterer intervention programs. Drawing from evidence that sequential treatment of substance use and IPV did not improve overall batterer intervention outcomes and is generally poorly coordinated and attended, Stuart et al. (2013) hypothesized that a brief, 90-minute adjunctive intervention to batterer intervention would improve IPV and alcohol use outcomes among men arrested for domestic violence (Bennett & Lawson, 1994; Dalton, 2007; Gondolf, 2009; McCollum et al., 2011). Results revealed that men who received the brief, motivationally-based alcohol intervention in addition to batterer intervention reported greater abstinence from alcohol and less frequent severe physical and psychological IPV perpetration 6 months after the intervention ended relative to men who only participated in batterer intervention (Stuart et al., 2013). Though improvements in alcohol use and IPV perpetration faded by 12 months post-intervention, these results hold promise for the efficacy of adjunctive alcohol interventions for populations court-referred to batterer intervention. To date, no research has evaluated whether adding an alcohol treatment component to batterer intervention improves IPV and alcohol use outcomes for women court-mandated to batterer intervention. This gap in research is notable given that alcohol use is associated with IPV perpetration and batterer intervention program dropout among women court-mandated to batterer intervention (Buttell et al., 2012; Stuart et al., 2006; Stuart, Moore, et al., 2003; Stuart et al., 2004; Stuart et al., 2013). Additionally, data on whether court-mandated batterer intervention reduces women’s physical IPV perpetration do not exist, which impedes clinical scientists’ ability to recommend evidence-based treatments for women arrested for domestic violence. To address these gaps, we conducted a randomized clinical trial with hazardous-drinking women arrested for domestic violence and attending batterer intervention in Rhode Island to evaluate whether adding a 90-minute alcohol intervention to batterer intervention improved women’s alcohol use and IPV outcomes relative to batterer intervention alone. We hypothesized that women who received the 90-minute alcohol intervention and batterer intervention would evidence less substance use, less IPV perpetration, less IPV victimization, and fewer new arrests/restraining orders during the 12 months post-intervention relative to women who only received batterer intervention. Trial Design We conducted a randomized clinical trial in which hazardous-drinking women arrested for domestic violence received a 90-minute brief alcohol intervention plus batterer intervention (BAI + BI) or batterer intervention alone (BI). Participants were assessed at baseline and at 3-, 6-, and 12-months post-intervention. Methods did not substantially change after trial commencement. The primary substance use outcomes were percentage of days abstinent from alcohol (PDAA), number of drinks per drinking day (DPDD), percentage of heavy drinking days (PHDD), and percentage of days abstinent from alcohol and drugs (PDAAD). The primary IPV outcomes were psychological aggression, physical assault, sexual coercion, and injury perpetration and victimization, and new arrests/restraining orders. Participants Two-hundred and nine women agreed to participate. All participants were court-referred to batterer intervention following a domestic violence arrest (i.e., no women self-referred to batterer intervention). Women were eligible for the study if they were 18 years of age or older, were participating in a batterer intervention program following a domestic violence arrest, and, if they reported hazardous drinking, defined as meeting one or more of the following criteria: scoring in the hazardous drinking range (i.e., > 5 as recommended by Neumann et al., 2004 for identifying women who are appropriate candidates for brief alcohol interventions) on the Alcohol Use Disorders Identification Test (Saunders et al., 1993), consuming > 4 drinks on one occasion at least monthly for the past year, and/or drinking to the point of self-defined intoxication at least once per month for the past six months. Participants were excluded if they (1) consumed ≥ 9 drinks daily, which could contribute to significant withdrawal symptoms if they were to quit drinking without medical supervision, (2) attended more than six batterer intervention program sessions prior to screening, (3) were incarcerated for more than half of the previous six months due to the potential impact of incarceration on drinking patterns, (4) evidenced psychosis and/or cognitive impairment, or (5) did not speak English. We opted to enroll participants in the study within the first six batterer intervention sessions to ensure that participants in the study would still be enrolled in the batterer intervention program at the time of their three-month follow-up. This way, if we had difficulty scheduling follow-up appointments, we were easily able to locate the participant at the BIP site. Participants were primarily White, non-Hispanic/Latino women (mean age = 31.80 years, SD = 10.60) with an average annual household income of $12,041.91 (SD = $12,328.31). See participant demographic and diagnostic characteristics of the final sample, by treatment condition, in Table 1. Table 1 Summary Statistics of Intent-to-treat Sample by Treatment Condition  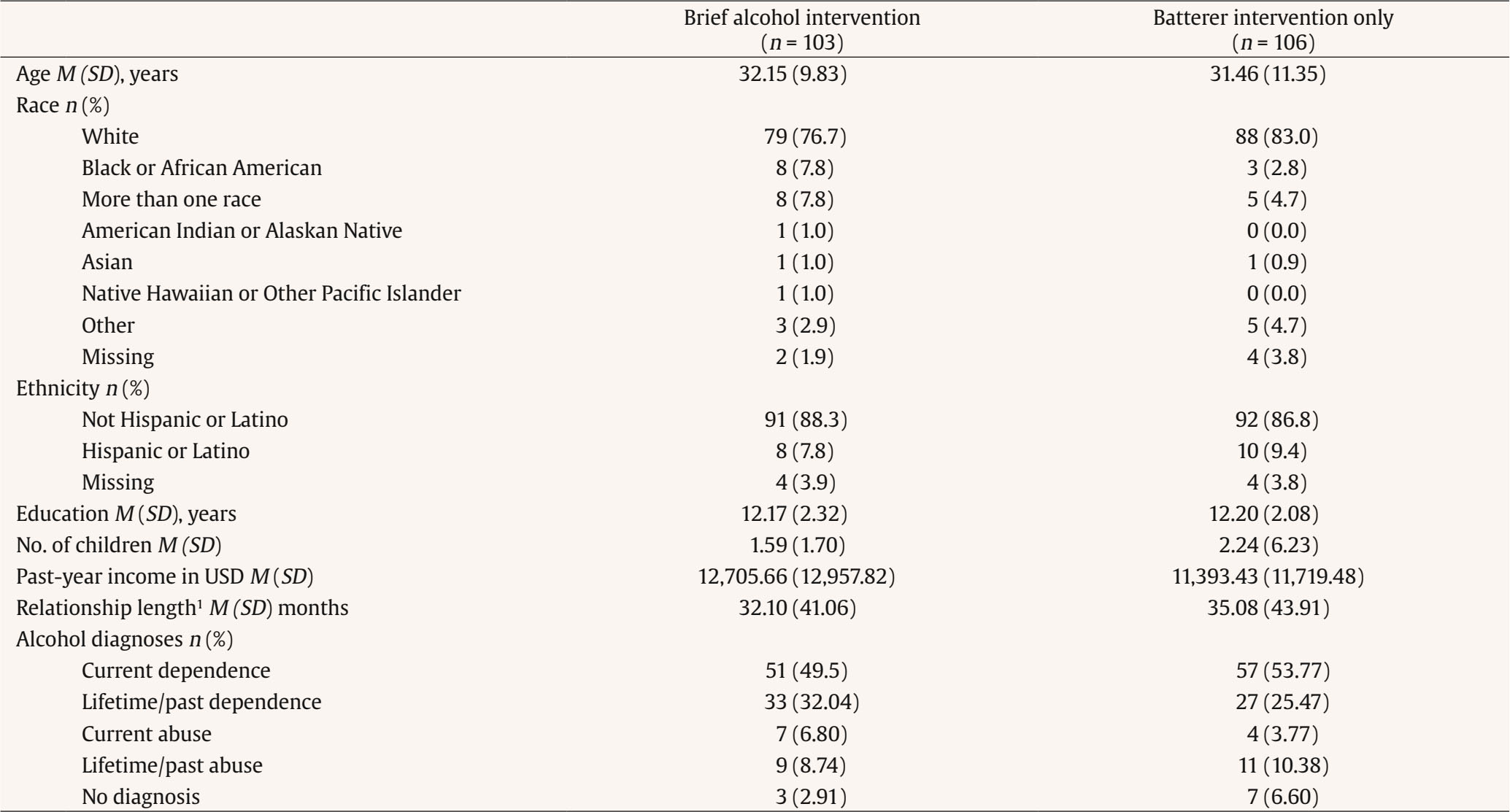 Note. Groups did not differ significantly on any baseline characteristics. 1Relationship length was only reported by participants who had a romantic partner at the time of the baseline assessment (n = 71 for the brief alcohol intervention + batterer intervention condition, and n = 73 for the batterer intervention only condition). SD = standard deviation; USD = United States dollars. Procedure Women were recruited during batterer intervention intake or groups across five Rhode Island batterer intervention programs. Batterer intervention sites were throughout the state of Rhode Island. Women were informed that their participation was voluntary. They were told that their data were protected by a certificate of confidentiality and that none of their information would be shared with batterer intervention staff. Participants signed a written consent form prior to completing paper-and-pencil screening questionnaires to determine eligibility. Participants were able to choose compensation in the form of either a check, gift cards to a local mall or grocery store, or batterer intervention program vouchers. Participants earned $75 for baseline, $50 for the 3-month follow-up, $75 for 6-month follow-up, and $100 for the 12-month follow-up. Women deemed eligible were given an additional written consent form, scheduled to complete a baseline assessment, and were compensated for completing screening and baseline assessments. Women were scheduled for in-person follow-up assessments at each time point and were compensated for completing each follow-up assessment. Women were asked to refrain from substance use prior to the brief alcohol intervention and assessment appointments and were breathalyzed at each appointment to confirm they were alcohol-negative. Of the 1,265 women screened, 1,006 did not meet inclusion criteria. Of the 259 eligible women, 48 declined to participate in the study and 2 had scheduling conflicts at baseline. Thus, the intent-to-treat sample was comprised of 209 participants (see Figure 1). Randomization Urn randomization (Wei, 1978) was used to randomly assign participants to treatment condition to ensure relationship status and frequency of physical violence was balanced between treatment conditions. Research assistants provided data pertaining to randomization to the last author who conducted the urn randomization. The last author had no knowledge of other participant characteristics unrelated to randomization. Research assistants were not masked to treatment condition because research assistants were often involved in scheduling participants’ sessions. Of the 209 participants, 106 were randomized to BI and 103 were randomized to the BAI + BI. At baseline, 71 women in the BAI + BI and 73 women in the BI had a current relationship partner. Interventions Batterer Intervention Program (BI) The Batterer Intervention Program Standards Oversight Committee of Rhode Island determined the content and training of group facilitators at each of the five sites for batterer interventions. Each site contained 40 hours of group batterer intervention, which included the following curriculum: communicating that violence is a serious crime, challenging excuses and justifications for abuse, devising a plan to reduce risk for future abuse, explaining models of abuse, identifying cultural and social influences that contribute to violence, communication skills training, discussing the impact of abuse on others, and homework assignments. Brief Alcohol Intervention (BAI) Doctoral- or Master’s-level therapists conducted the 90-minute, audiotaped BAI session. The BAI session manual was adapted from the Motivational Enhancement Therapy manual used in Project MATCH (Miller et al., 1995) and included rapport building, empathy expression, support for self-efficacy to change alcohol use, personalized feedback about current drinking, eliciting motivation to change drinking, discussion on the relation between alcohol use and IPV, identifying discrepancies between current and desired level of drinking, and planning for changes in drinking. Motivational interviewing (Miller & Rollnick, 2002) techniques intended to minimize resistance were central to the BAI. Therapists heavily relied on a non-confrontational approach given that participants were not seeking treatment to address their alcohol use and may have been ambivalent about changing their drinking. Within the BAI, ambivalence was addressed by asking women to reflect on and discuss the pros and cons of their drinking. Therapists provided personalized feedback on women’s current drinking in relation to national norms, alcohol-related consequences, risk from women’s family history of alcohol problems, risk conferred by other drug use, women’s reasons for drinking, and risk from depression, generalized anxiety, and trauma symptoms. Therapists also discussed the temporal association between substance use and IPV, how women with alcohol problems were more likely to become physically aggressive, and that when women drank they were at greater risk for IPV victimization. Furthermore, we discussed that women’s partners were more likely to be violent on partner-drinking and partner-heavy-drinking days. Women who were interested in changing their drinking behaviors were asked to (1) specify the change that they would make, (2) detail the steps that would be involved in making the change, (3) identify ways in which others might be helpful toward their efforts to change, (4) generate potential barriers to change, and (5) problem solve ways to address barriers to change. Participants were sent a letter within a week of the BAI that reviewed the session and encouraged them to follow through with their commitment to change. Measures Alcohol Use Disorder Assessment The Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, fourth edition (SCID-IV) is a widely used and well-validated semi-structured interview that was used to assess diagnostic criteria for current and lifetime alcohol use disorder (previously referred to as alcohol abuse and dependence per the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (American Psychiatric Association, 2000; First et al., 1995; Kranzler et al., 1996). Outcome measures Alcohol and Drug Use. We assessed substance use with the Timeline Followback Interview (TLFB; Sobell & Sobell, 1996), which is one of the most reliable and valid methods of assessing prior alcohol use (Sobell & Sobell, 1979, 1980). The TLFB is a structured interview that cues participants’ memory using a calendar with holidays and dates of personal significance highlighted. Participants are asked to recall drinking and drug use for each day. The TLFB interview has excellent reliability and validity for up to 24 months, and is considered the gold standard in retrospective substance use reporting (Carney et al., 1998; Sobell & Sobell, 1979, 1980, 1992, 2003). At baseline, the TLFB was administered for the six months prior to the interview and, at each follow-up assessment, it was administered for the time since the previous interview. If participants endorsed drinking on a given day, they were asked to report the number of standard drinks consumed on that day. Heavy drinking was defined as ≥ 4 drinks on one occasion. From the TLFB, we examined participants’ reports of percentage of days abstinent from alcohol (PDAA), percentage of days abstinent from both alcohol and drugs (PDAAD), average number of drinks consumed per drinking day (DPDD), and percentage of heavy drinking days (PHDD). Intimate Partner Violence. The Revised Conflict Tactics Scale (CTS2; Straus et al.,1996; Strauss et al., 2003) was used to assess psychological aggression (8 perpetration and 8 victimization items), physical assault (12 perpetration and 12 victimization items), sexual coercion (7 perpetration and 7 victimization items), and IPV that caused injury (6 perpetration and 6 victimization items). The CTS2 is the most widely-used self-report measure of IPV, with adequate reliability and validity of the CTS2 being demonstrated across various samples (Straus et al., 1996). For each item, participants report the frequency with which they engaged in each behavior ranging from 0 (never) to 6 (more than 20 times). The CTS2 is scored by summing the frequency of each of the behaviors for each subscale, with higher scores indicating more frequent IPV. For the baseline assessment, the CTS2 was administered to participants who had a relationship partner. Participants were asked to report the frequency with which they perpetrated and were victimized by IPV within the prior 6 months from the baseline assessment. For each follow-up assessment, participants completed the CTS2 if they remained in a relationship with the same partner. Participants were asked to report the frequency with which IPV occurred since the previous assessment. Arrest record information, which included the number of domestic violence arrests and restraining orders filed during the follow-up period, was available for all participants at 12-month follow-up assessments. Data Analytic Strategy To examine the effects of treatment across time on alcohol use and IPV, analyses were conducted using multilevel modeling in HLM7 (Raudenbush et al., 2011). Multilevel modeling was also employed due to the data being nested within individuals due to repeated assessments. For PDAA, PDAAD, DPDD, PHDD, normal distributions were specified. For IPV, frequency of perpetration and victimization at all three follow-ups were the dependent variables, with a Poisson distribution specified due to positive skewness and count data derived from IPV variables. When examining alcohol use outcomes, baseline indicators of alcohol use (i.e., PDAA, PDAAD, PHDD, DPDD) were entered as covariates for the corresponding indicator of use at follow-ups. When examining IPV outcomes, baseline indicators of IPV were entered as covariates for the corresponding indictor of IPV at follow-ups. Analyses were conducted in two steps. In the first level of the model, time, coded as the number of months since baseline, was entered as a predictor of each outcome variable. Treatment group (dummy coded with BI as the reference) was entered onto the intercept in the second level of the model, as was the baseline level of the outcome variable. A second model was then conducted that added the time x treatment group interaction. All predictor variables were uncentered and specified with random slopes. Significant time x treatment group interactions were explicated by centering the time variable and examining the treatment effects at each follow-up assessment (i.e., 3-, 6-, and 12-month follow-ups). In the absence of significant time x treatment group interactions, main effects models were interpreted. We report unstandardized B values which represent a metric of effect size (also known as the simple effect size) that is more robust, versatile, and preferable than standardized effect size metrics (e.g., Cohen’s d) because standardized effect size metrics are negatively impacted by factors such as reliability, range restriction, and study design (Baguley, 2009). In contrast, unstandardized B provides a metric that is independent of the variance and more meaningful than an unstandardized effect size because it is scaled in terms of the original units of analysis (i.e., it describes the degree of change in terms of the units of measure; Baguley, 2009). Following multilevel modeling, we conducted a t-test to compare the number of arrests for women in the BAI + BI group to women in the BI group. Means and standard deviations of study variables by treatment condition are displayed in Table 2. Results of multilevel modeling analyses are presented in Table 3. Table 2 Means and Standard Deviations of Study Variables by Treatment Condition  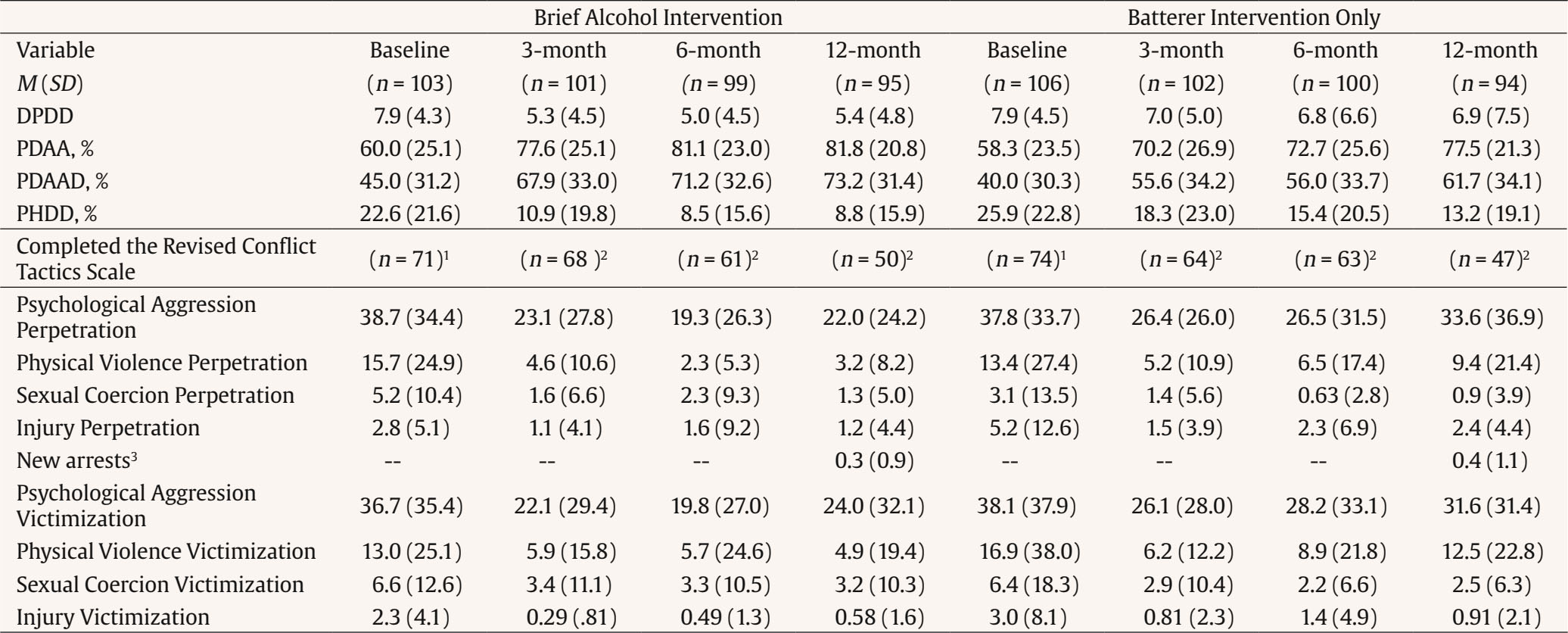 Note. DPDD = drinks per drinking day; PDAA = percentage of days abstinent from alcohol; PDAAD = percentage of days abstinent from alcohol and drugs; PHDD = percentage of heavy drinking days; 1participants who had a romantic partner at baseline; 2participants still in a relationship with the same partner from the baseline assessment; 3new arrest data were only collected at 12-month follow-up assessments. Table 3 Parameters of Models Predicting Substance Use and IPV Outcomes at 3, 6, and 12 Months after Intervention  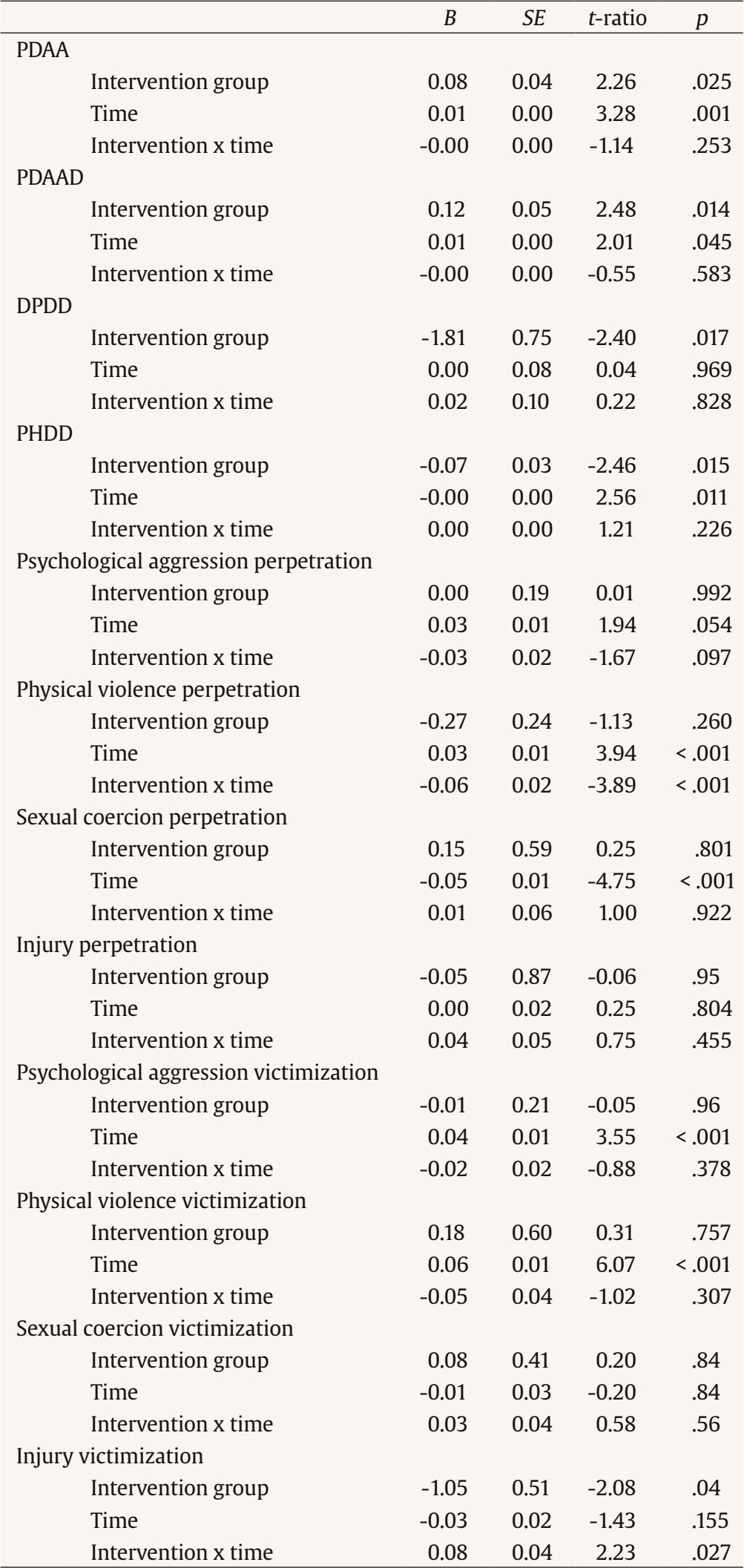 Note. PDAA = percentage of days abstinent from alcohol; PDAAD = percentage of days abstinent from alcohol and drugs; DPDD = drinks per drinking day; PHDD = percentage of heavy drinking days. Participants were considered missing if they could not be located or were in a controlled environment (e.g., prison) for the duration of the follow-up interval. Follow-up rates were 97.13% (3-month), 95.21% (6-month), and 90.43% (12-month); excluding the three deceased participants (see Adverse Events below), the 12-month follow-up rate among people still living was 91.38%. Attrition across the two treatment conditions was comparable (see Figure 1). Two participants who received BI and one participant who received BAI + BI died prior to follow-up assessments. These events were unrelated to study participation. There was a significant main effect of treatment condition across time for PDAA (t = 2.26, B = 0.06, SE = 0.03, p = .02), PDAAD (t = 2.86, B = 0.10, SE = 0.03, p = .005), DPDD (t = -2.75, B = -1.65, SE = 0.60, p = .007), and PHDD (t = -2.49, B = -0.05, SE = 0.02, p = .014), such that women in the BAI + BI condition reported a higher percentage of days abstinent from alcohol, higher percentage of days abstinent from both alcohol and drugs, lower number of drinks per drinking day, and lower percentage of heavy drinking days relative to women in the BI condition. There was also a significant main effect of time for PDAA (t = 3.64, B = 0.01, SE = 0.00, p < .001), PHDD (t = -2.67, B = -0.00, SE = .00, p = .01), and PDAAD (t = 2.67, B = 0.01, SE = 0.00, p = .01), such that women reported a higher percentage of days abstinent from alcohol, a lower percentage of heavy drinking days, and a higher percentage of days abstinent from both alcohol and drugs as time since intervention completion increased. There were no significant interactions between treatment groups and time in any model. Intimate Partner Violence Outcomes IPV Perpetration In the physical IPV perpetration model, results revealed a significant time x treatment group interaction (see Table 3). Explicating the interactions revealed that, relative to women who received BI alone, women who received BAI + BI reported significantly less frequent physical IPV perpetration at 3-month follow-up (B = -0.45, p = .049), 6-month follow-up (B = -0.64, p = .01), and 12-month follow-up (B = -1.01, p < .001). In the sexual coercion model, there was a significant main effect of time such that women, regardless of intervention group, perpetrated less sexual coercion as time since intervention completion increased. No main effects or time x treatment group interactions emerged for psychological aggression perpetration or perpetration that caused injury to a partner. Although women who received BAI + BI had fewer arrests and restraining orders filed against them during the follow-up period than did women who received BI alone, this difference was not statistically significant, t(207) = 0.76, p > .10. IPV Victimization In the injury victimization model, results revealed a significant time x treatment group interaction (see Table 3). However, explicating the interaction revealed that, at three months post-intervention, women who received BAI + BI trended toward reporting less injury victimization than did women who received BI alone, but this difference was not statistically significant (t = -1.83, B = -0.81, SE = 0.44, p = .07), treatment group differences with regard to injury victimization were not statistically significant at 6-month follow-up (t = -1.41, B = -0.56, SE = 0.40, p = .16), or 12-month follow-up (t = -0.16, B = -0.06, SE = .39, p = 0.87). There were no other significant time x treatment group interactions. For the psychological and physical IPV models, significant main effects for time emerged; regardless of intervention received, women reported more frequent physical and psychological IPV victimization as time since intervention completion increased. Results demonstrated no significant main effects for sexual coercion victimization. This is the first randomized clinical trial to examine the incremental efficacy of a brief, adjunctive alcohol intervention to batterer treatment for hazardous-drinking women arrested for domestic violence and court-referred to batterer intervention programs. Our hypothesis was partially supported. Relative to women who received only batterer intervention, women who also received the 90-minute alcohol intervention reported a higher percentage of days abstinent from alcohol, higher percentage of days abstinent from both alcohol and drugs, lower number of drinks per drinking day, and lower percentage of heavy drinking days for 12 months following the brief intervention. Women receiving the brief alcohol intervention also reported perpetrating physical IPV less frequently than did women who only received batterer intervention; the benefits of the adjunctive alcohol intervention relative to batterer intervention alone became more apparent over time and persisted for 12 months post-intervention. Although women in both treatment groups continued to experience psychological and physical IPV victimization with increasing frequency as time since intervention increased, women who received the brief alcohol intervention experienced less frequent injuries from IPV victimization relative to women who only received batterer intervention, though this difference was not statistically significant. In contrast to our hypothesis, no group differences emerged for psychological IPV perpetration, IPV perpetration that caused injury, sexual IPV victimization, or new arrests/restraining orders. Results of the present study extend to women conclusions that were previously limited to men arrested for IPV: that targeting alcohol use in treatment corresponds to reductions in IPV perpetration (Easton et al., 2007; Easton & Sinha, 2002; Klosterman et al., 2010; O’Farrell et al., 2004, 1999; Stuart et al., 2002; Stuart et al., 2013). For hazardous-drinking men arrested for domestic violence, the superiority of a 90-minute, adjunctive alcohol intervention over batterer intervention alone diminished after 6 months (Stuart et al., 2013). However, the present findings suggest that, for women arrested for domestic violence, the superiority of a 90-minute adjunctive alcohol intervention over batterer intervention alone persisted 12-months post-treatment. Scant data point to specific components of alcohol interventions for women who perpetrate IPV. Consistent with data supporting the general efficacy of brief, motivationally-based interventions in reducing alcohol use (DiClemente et al., 2017; Kaner et al., 2018; Lundahl et al., 2010; O’Donnell et al., 2014), our findings suggest that just 90 minutes of alcohol intervention can reduce women’s substance use and physical IPV perpetration when the intervention includes (1) a non-confrontational therapist stance, (2) discussions on the alcohol-IPV link, (3) personalized feedback about current drinking, (4) developing discrepancies between current and desired drinking, and (5) identifying plans for change. Notably, women who received the brief alcohol intervention also reported a lower percentage of days that involved both drug and alcohol use. Reminders of their commitment to change were mailed to women one week after completing the brief alcohol intervention, which may have aided in maintaining behavior change over time (Neal et al., 2012; Verplanken, 2005). Future research is needed to evaluate specific components of batterer and motivationally-based alcohol interventions that facilitate changes in women’s substance use and IPV. Despite these promising results, women in both treatment groups continued to report IPV perpetration and victimization, as well as causing and experiencing IPV-related injuries at 12 months post-treatment. Similarly, physical and psychological IPV victimization increased as time since intervention completion increased. Although Rhode Island has a “primary aggressor” law (i.e., officers are required to attempt to identify a “primary aggressor” when considering the arrest of both parties following an IPV incident; Domestic Violence Prevention Act, 1988), which suggests that women in the present study were identified as the primary aggressor when arrested, it is plausible that some women were involved in bidirectionally-violent relationships or were dually arrested with their partner (Durfee, 2012; Hirschel & Deveau, 2017). Women’s partners may not have learned strategies for reducing IPV perpetration, thereby contributing to women’s continued psychological and physical victimization post-intervention. Notably, women who received the brief alcohol intervention sustained less frequent IPV-related injuries relative to women who did not receive the brief alcohol intervention, which suggests that a brief alcohol intervention may offer the benefit of protecting women from more physically injurious forms of IPV victimization. Nonetheless, batterer interventions for women should address IPV victimization and include safety planning to enhance women’s safety. We opted to evaluate a 90-minute alcohol intervention because we believed that an intervention of this duration would be easily exportable to community settings if efficacious, and based on evidence that a 90-minute alcohol intervention improved substance use and IPV outcomes among men arrested for domestic violence (Stuart et al., 2013). However, investigators may consider evaluating whether booster sessions, reminders of change talk/plans, and other techniques to help bolster behavior change and habit (e.g., self-monitoring, cues, incentives) enhance IPV outcomes. Similarly, investigators have proposed that targeting mental health characteristics of women who perpetrate IPV, including depression, posttraumatic stress disorder, and drug use, may strengthen the efficacy of batterer interventions for women (Babcock et al., 2016; Dowd et al., 2005; Stuart et al., 2006). Despite a number of treatment programs being recommended for women who perpetrate IPV (e.g., Bowen, 2009; Dowd & Leisring, 2008; Hamberger & Potente, 1994; Leisring et al., 2003), there have not been randomized clinical trials that evaluate the efficacy of such programs in reducing IPV among women court-mandated to batterer intervention programs. The present findings support treatment components that may reduce IPV and alcohol use among hazardous-drinking women in batterer intervention programs, but additional research on batterer intervention efficacy among women is sorely needed. Results of the present study should be evaluated while considering limitations. Although less than 10% of the total sample (9.57%) was excluded due to their relationships ending, these relationships may have involved more severe IPV. Additionally, IPV can continue or increase after relationships end (Anderson & Saunders, 2003), and IPV could occur with new partners; however, examining IPV in these contexts is beyond the scope of the present study. Future research would benefit from continued assessment of IPV over time with a larger sample. Corroborating reports of IPV from one’s partner and more objective substance use data (e.g., urine drug testing, wearable alcohol sensors) were not obtained. Future studies should collect corroborating reports of IPV and substance use because women may underreport these stigmatizing behaviors. Additionally, participants’ IPV measures were only analyzed if they were in a relationship at baseline and remained in a relationship with that same partner at each follow-up assessment. IPV data collected during the 12-month post-intervention assessment from women who ended their relationships during the study were not analyzed to prevent artificial deflation of IPV data due to less partner contact. IPV was measured using the CTS2 (Straus et al., 1996, 2003) which does not assess the contexts of or motivations for IPV. Given that a substantial portion of IPV is bidirectional (Langhinrichsen-Rohling, et al., 2012), it is plausible that some IPV was perpetrated in self-defense. Relatedly, targeting one partner’s IPV perpetration and alcohol use may be insufficient in reducing the other partner’s perpetration. The present study’s sample included primarily white women whose sexual orientations and gender identities are unknown. Additional research is needed to determine whether the present findings extend to populations who are more ethnically, sexually, and gender diverse. Finally, the present study was the first trial to examine the effects of a brief alcohol intervention on women’s IPV perpetration and involved a relatively small sample. We conducted separate analyses for each outcome variable, which may increase type I error. Additional trials with larger samples are needed to replicate and extend results. Limitations notwithstanding, the present study demonstrates that adding a 90-minute, motivationally-based alcohol intervention to batterer intervention improves alcohol and physical IPV outcomes for 12 months among hazardous drinking women arrested for domestic violence. These results offer an initial step toward the development of evidence-based intervention programming for women court-referred to batterer intervention. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Brem, M. J., Shorey, R. C., Ramsey, S. E., & Stuart, G. L. (2023). Randomized clinical trial of a brief alcohol intervention as an adjunct to batterer intervention for women arrested for domestic violence. Psychosocial Intervention, 32(2), 79-88. https://doi.org/10.5093/pi2023a4 Funding: This work was supported by the Spanish Ministry of Health, Consumption and Social Services, National Drugs Plan (PND2018/021). |
Cite this article as: Brem, M. J., Shorey, R. C., Ramsey, S. E., & Stuart, G. L. (2023). Randomized Clinical Trial of a Brief Alcohol Intervention as an Adjunct to Batterer Intervention for Women Arrested for Domestic Violence. Psychosocial Intervention, 32(2), 79 - 88. https://doi.org/10.5093/pi2023a4
Correspondence: gstuart@utk.edu (G.L. Stuart).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






