A Controlled Evaluation of a Psychosocial Outreach Support Program for Adults with Severe Mental Illness
Melissa Savaglio1, Ash Vincent2, Marianne Bentley2, Jasmine Gaul2, Stuart Poke2, Nicole Watson2, Helen Skouteris1, and 3
1Health and Social Care Unit, School of Public Health and Preventive Medicine, Monash University, Melbourne, Victoria, Australia; 2Baptcare, Tasmania, Australia; 3Warwick Business School, University of Warwick, Coventry, United Kingdom
https://doi.org/10.5093/pi2024a12
Received 19 February 2024, Accepted 5 June 2024
Abstract
Objective: Serious mental illness (SMI) remains a leading cause of disability worldwide. However, there is limited Australian evidence of community-based programs to enhance the psychosocial wellbeing of adults experiencing SMI. Foundations is a long-term community-based psychosocial outreach support program delivered in Tasmania, Australia. A longitudinal non-randomised controlled trial was conducted to examine the effectiveness of the Foundations program on adults’ psychosocial functioning, clinical symptomology, and hospital readmissions, in comparison to standard care only. Method: Participants were adults aged 18-64 years experiencing SMI. Control participants received standard clinical care only. Intervention participants were engaged in the Foundations program in addition to standard care. Data were collected at program commencement, midpoint, closure, and six-months post-closure. Linear mixed modelling was used to examine differences between groups. Results: Intervention participants achieved better psychosocial functioning in comparison to the control group by program closure and at six-month follow-up. No significant differences were observed for clinical mental health symptomology or hospital readmission rates. Length of readmission stay was significantly shorter for intervention participants. Conclusions: The findings highlight the additional value of community-based, recovery-oriented, psychosocial outreach support alongside clinical mental health care to enhance the psychosocial wellbeing of adults experiencing SMI.
Keywords
Serious mental illness, Psychosocial, Outreach, Controlled trial, AustraliaCite this article as: Savaglio, M., Vincent, A., Bentley, M., Gaul, J., Poke, S., Watson, N., & Skouteris, H. (2024). A Controlled Evaluation of a Psychosocial Outreach Support Program for Adults with Severe Mental Illness. Psychosocial Intervention, 33(3), 179 - 185. https://doi.org/10.5093/pi2024a12
Correspondence: helen.skouteris@monash.edu (H. Skouteris).Mental illness continues to be a leading cause of disability and non-fatal burden of disease (World Health Organisation, 2023). It is estimated that 3-5% of adults experience a serious mental illness (SMI) each year, defined by a mental, behavioural, or emotional disorder that causes significant functional impairment, which severely hinders a person’s daily life/activities (National Institute of Health, 2023; Whiteford et al., 2017). Burden of disease and psychiatric hospitalisations (and readmissions) are also high among this population (Teigland et al., 2018). People with severe and persistent mental illness often have multidisciplinary psychosocial needs that are generally beyond the scope of traditional clinical mental health services (Isaacs et al., 2019; Whiteford et al., 2017). The most common unmet needs frequently reported by people with SMI often include support with daily activities/personal functioning, housing, social participation, employment/volunteering, physical health, and money (Isaacs et al., 2019). However, accessing appropriate services remains a challenge, with more than half of adults with SMI not receiving the support that they require to address such needs (Australian Bureau of Statistics, 2022). In recent years, mental health systems worldwide have undergone reform to better integrate mental health services into the community and reduce reliance on acute care. Specific focus has been on strengthening community-based supports and increasing the capacity of community services to provide more holistic, wrap-around options for adults experiencing serious mental illness that may provide more complementary, and step-down support to acute clinical services (Tyler et al., 2019). Case management approaches are well-established community-based models of care to support adults with SMI. The provision of consistent, goal-oriented, multidisciplinary wrap-around support has been shown to enhance improvements in clinical recovery (Dieterich et al., 2017). However, key limitations are widely recognised (i.e., high caseloads, short-term duration, inflexible engagement strategies, medical model, lack of recovery-oriented ooutcomes. This has led to calls for the development and implementation of adapted community approaches that may better suit this population (Harvey et al., 2023). The implementation and effectiveness of community-based models of care in the Australian community mental health sector for SMI is less established, and only few evaluations have demonstrated promising findings (O’Donnell, Savaglio, Vicary, et al., 2020; Smart et al., 2020). Despite yielding positive clinical outcomes, a greater focus on enhancing broader psychosocial functioning is warranted. To address the local gap of community-based psychosocial support for adults with SMI in the state of Tasmania, Australia, the Foundations program was developed in a collaborative partnership between the Tasmanian Health Service (Department of Health and Human Services) and a not-for-profit community service organisation, Baptcare. This organisation provides state-wide community-based psychosocial support for adults experiencing mental illness through its Mindset TAS service (Baptcare, 2023b). Foundations (previously called MyCare and MIcare) is a long-term psychosocial assertive outreach support program for people experiencing mental illness following a psychiatric admission (Baptcare, 2023a). It is delivered in tandem with clinical mental health case management support; this collaborative partnership approach seeks to meet adults’ clinical and psychosocial needs in the community. Nonetheless, Foundations extends upon standard case management through its assertive outreach approach, provision of wrap-around psychosocial support, long-term duration, smaller caseloads (8:1), and high intensity and flexibility of support. A recent qualitative study examined the program’s implementation from the perspective of key stakeholders, including clients and staff (O’Donnell, Ayton, et al., 2020). This preliminary evaluation demonstrated how core components of the Foundations program (i.e., relationship-focused, recovery-oriented, assertive outreach approach) were crucial to successfully implementing this model of psychosocial support (O’Donnell, Ayton, et al., 2020). However, the effectiveness of the program is yet to be established. There is also a lack of local Australian evidence of controlled evaluations of community-based programs to support adults experiencing SMI following psychiatric admission. A controlled evaluation is warranted to effectively build the evidence-base of such programs and scale-up supports to improve psychosocial outcomes for the community. Therefore, the aim of this study was to use a longitudinal non-randomised controlled trial to examine the effectiveness of the Foundations program on adults’ psychosocial functioning, clinical symptomology, and hospital readmissions, in comparison to standard care only. It was hypothesised that Foundations would yield significantly greater improvements in psychosocial functioning above and beyond that of standard clinical care only. Ethics and Study Design The study involved a longitudinal non-randomised controlled comparison design. Ethics was approved by the Tasmanian Health and Medical Human Research Ethics Committee (18536) and the Monash University Human Research Ethics Committee (25374). The study was registered with the Australian New Zealand Clinical Trial Registry and reporting followed the CONSORT guidelines (Schulz et al., 2010). It was conducted across the state of Tasmania, Australia. Data were collected across Baptcare’s three service regions in the South, North, and North West. The evaluation period was conducted over three years between 2019 and 2022. Further methodological details are published in the evaluation protocol (O’Donnell, Savaglio, Fast, et al., 2020). Patient and Public Involvement A lived-experienced advisory group of previous service-users with SMI underpinned every stage of this research. The advisory group advised the research team on the type of evaluation to be conducted, appropriate recruitment procedures, seeking informed consent, measures to be used, data collection procedures, and they supported the interpretation and dissemination of the study findings. Participants Participants met all of the following eligibility criteria: (1) aged 18 to 64 years, living in Tasmania, (2) diagnosed with a serious mental illness (SMI), (3) had a recent psychiatric admission prior to referral, (4) actively case managed by state-wide Mental Health Services (MHS), which provide ongoing clinical care and follow-up post-hospitalisation, (5) were voluntarily willing to engage, and (6) verbally consented to having their assessments shared with the research team. Exclusion criteria included: (1) engagement in any other community-based psychosocial support program or (2) on an involuntary order. Eligible participants who were referred to the Foundations program for wrap-around psychosocial support made up the intervention group. The control group comprised of participants who met the above eligibility and were engaged with MHS only. As this study was a naturalistic comparison of clients receiving standard care vs. standard care plus Foundations, group allocation could not be randomised nor concealed, yet participants were matched based on key demographic characteristics (e.g., age, gender, and service engagement duration). Control – Mental Health Services (MHS) Only All participants were engaged with MHS for standard clinical care following a psychiatric hospitalisation; the control group received this standard care only. MHS was operated through the Tasmanian Department of Health and provided individuals with clinical case management to promote clinical improvements. MHS case managers were embedded within a multidisciplinary team (i.e., psychologists, psychiatrists, mental health nurses, social workers, occupational therapists, and other specialist medical staff) and had a caseload of approximately 25 clients. MHS focused solely on addressing the clinical symptoms of the mental illness through the provision of assessment, psychoeducation, symptom management, medication, and monitoring medication adherence. Participants received clinical case management from their MHS case manager for an average of 13 months (M = 13.51, SD = 5.19), ranging between 11 and 18 months. Participants’ average frequency of contact with MHS was fortnightly, comprising of in-person centre-based visits or telephone support. Intervention – The Foundations Program In addition to receiving standard clinical support from MHS, participants in the intervention group engaged in the Foundations program. Foundations is a nationally-accredited, long-term (up to 18 months), capacity building psychosocial outreach program to support people experiencing severe and persistent mental illness. The program is underpinned by strengths-based, person-centred, goal-focused, assertive outreach, and recovery-oriented practice to facilitate improvements in clients’ psychosocial wellbeing. The Foundations program extends upon standard case management by incorporating lower caseloads, assertive outreach engagement strategies, a consistent key practitioner, higher intensity, longer-term duration, and a more flexible holistic approach (O’Donnell, Ayton, et al., 2020). Eligible clients who met the above criteria were referred into the Foundations program by their MHS case manager, following a psychiatric admission. MHS referred to Foundations when they identified that a client required additional psychosocial support and was not already engaged in any other community-based service. The MHS case manager and Foundations senior practitioner determined the appropriateness of the referral, depending on the client’s psychosocial needs and current program capacity. Approximately 87% of all eligible clients participated in the current evaluation. Each client was allocated a Foundations practitioner, who supported clients to set and achieve their own personalised psychosocial goals to enhance their psychosocial wellbeing (encompassing emotional, social, physical or spiritual dimensions of health). Practitioners provided assertive outreach support to assist clients in achieving their goals. Examples of key psychosocial goals included improving social connections with family/peers, increasing capacity to manage day-to-day activities, encouraging re-engagement in employment/volunteering, or healthy lifestyle behaviours (e.g., engaging in exercise, accompanying the client while grocery shopping to improve eating habits). Brokerage was also available to fund activities that may support the achievement of psychosocial goals. Participants engaged in Foundations for 11.5 months on average (M = 11.6, SD = 5.5), ranging between 10 and 18 months. Frequency and intensity of support varied throughout program engagement as practitioners have the flexibility to operate on a needs-led basis depending on each client’s required level of support. On average, clients received approximately two outreach visits per week from their key practitioner for 1.5 hours at their home or in the community (i.e., café, park, transport to and from appointments, walk). Practitioners had a small caseload of 1:8 clients which allowed them to adopt a personalised and tailored approach. Practitioners completed an average of four background (non-client) hours per week per client (M = 4.22, SD = 1.36), which included outreach travel time, administration, and referral/service navigation. Foundations practitioners had significant community services experience and various background qualifications (i.e., social work, community services), which ensured they were well-equipped to support individuals experiencing mental illness. Practitioners engaged in regular training and professional development opportunities, and frequent supervision, including both one-on-one and peer group supervision. Foundations practitioners worked collaboratively with the community-based MHS case managers, who maintained oversight over the client’s clinical mental health care. The collaborative partnership and regular contact between MHS and Foundations was crucial to program implementation in providing complementary support. A more detailed description of the Foundations program is published elsewhere (O’Donnell, Ayton, et al., 2020; O’Donnell, Savaglio, Fast, et al., 2020). Outcome Measures Demographic information was collected upon referral (Time 1 - baseline). Demographic characteristics included age, gender, country of birth, relationship status, highest level of education achieved, and any mental health diagnoses given by MHS. Data were collected by the allocated Foundations practitioner (intervention group) or MHS case manager (control group) in collaboration with the client. Practitioners completed two measures with their client to measure outcomes across four time-points: Time 1 at baseline (upon entry into the program), Time 2 at program midpoint (approximately six months of program engagement), Time 3 at program closure (approximately 12 months of program engagement), and Time 4 at six months post-closure (follow-up for intervention group only). Completion of the measures at this time-point was more reliant on participants’ self-report rather than the practitioners’ perspective, as clients were no longer involved in the program. Psychosocial Functioning The Behavioural and Symptom Identification Scale (BASIS-32) was used to assess psychosocial functioning. It has high validity and internal reliability (α = .75 to α = .91; Cameron et al., 2007) to measure the extent of difficulty that an individual experiences in five psychosocial functioning areas: (1) relation to self and others, (2) daily living and role functioning, (3) depression/anxiety, (4) impulsive/addictive behaviour, and (5) psychosis. Each item (n = 32) is scored on a 5-point Likert scale from 0 (no difficulty) to 4 (extreme difficulty). Participants received an overall total averaged score and an average score for each domain. Lower scores indicated less impairment/difficulty in psychosocial functioning. The study’s primary outcome was overall psychosocial functioning at closure (Time 3), as measured by the total BASIS-32 score. All other outcomes were secondary. Clinical Symptomology The Health of the Nations Outcomes Scale (HoNOS) was used to assess the severity of clinical mental health problems. It is well-regarded as a valid tool with moderate to high internal consistency (α = .59 to .76; Pirkis et al., 2005) to measure clinical severity across four domains: (1) behaviour (i.e., substance use, aggression, self-injury, overactivity), (2) impairment (i.e., cognitive or physical illness/disability), (3) symptomology (i.e., symptoms of anxiety/depression/psychosis), and (4) social functioning (i.e., social relationships, employment, living conditions, daily activities). The 12 items were rated on a 5-point Likert scale from 0 (no problem) to 4 (severe problem). Participants received an overall total score (total sum of all 12 items) and a score for each domain (sum of domain items). Lower scores indicated lower severity of clinical mental health symptomology. These two measures were chosen for the primary outcomes as they were already routinely used by MHS to inform case planning. Therefore, they were embedded into standard practice within the Foundations program to enable comparisons between groups. Practitioners received training in administering the two questionnaires to ensure inter-rater reliability and to minimise variability associated with individual interpretation. All data provided to the research team were de-identified, as participants were assigned a unique code. Psychiatric Readmissions The Tasmanian Health Service provided the research team with de-identified hospital admission data. Data included date of hospital admission, reason for admission, and date of discharge for any participants during the study period. This data was used to compare the number of psychiatric-related hospital admissions and length of stay (in days) between groups within six months of program closure. Data Analysis Analyses were performed using IBM SPSS Statistics version 28. Linear mixed modelling (LMM) was the main analysis used to examine differences in scores on the outcomes measures between the intervention and control groups, whilst controlling for age, gender, baseline HoNOS and BASIS ratings, and service engagement duration. Time was the within predictor with four time-points: baseline (Time 1), midpoint, (Time 2), closure (Time 3), and six-months postintervention (Time 4). Group was the between predictor: intervention and control group. This analysis was chosen to compare changes between groups over the time-points in order to determine the effect of the intervention. Compared to other analyses, such as mixed methods analysis of variance, LMM removes randomly missing observations without deleting the participants, so that all participants could be included in the analysis and imputation methods were not required. Post-hoc pairwise comparisons were conducted for outcomes that yielded a significant group x time interaction to determine at which time points groups differed. Sample size calculations for the LMM analysis were conducted using G*Power, with 145 participants required overall to detect statistically significant differences in the primary outcome measure (overall psychosocial functioning at closure) between groups with 80% power. Chi-square tests were used to calculate differences between groups on categorical baseline characteristics and hospital readmission rates. Independent t-tests were used to calculate differences between groups on baseline age and length of re-admission stay. Paired sample t-tests were conducted to compare intervention participants’ mean differences on each outcome measure from closure to six-month follow-up. All relevant assumptions for each analysis were met. Cohen’s d was used to estimate effect sizes, with benchmarks of 0.20, 0.50, and 0.80 indicating small, moderate, and large effects, respectively (Cohen, 1969). A Bonferroni correction was applied where multiple comparisons were tested to account for Type 1 error (Larzelere & Mulaik, 1977). Participant Characteristics There were 204 adults who participated in the study, with n = 103 in the intervention group and n = 101 in the control group. The six-month-follow-up assessment was completed by 54 intervention participants (52%). The remaining 48% either did not provide consent/declined to participate in the follow-up or were uncontactable after three attempts. Table 1 presents a summary of the sociodemographic and descriptive characteristics of both groups. Participants in the intervention group were slightly older in age (M = 42.61, SD = 12.86), in comparison to the control group (M = 39.15, SD = 11.89). There were no other statistically significant differences in baseline characteristics between groups. On average, the sample was 41 years of age, born in Australia, identified as male, were not in a relationship, had a high school-level education, and were most commonly experiencing depression. Table 1 Sociodemographic Characteristics of Participants in the Intervention and Control Groups  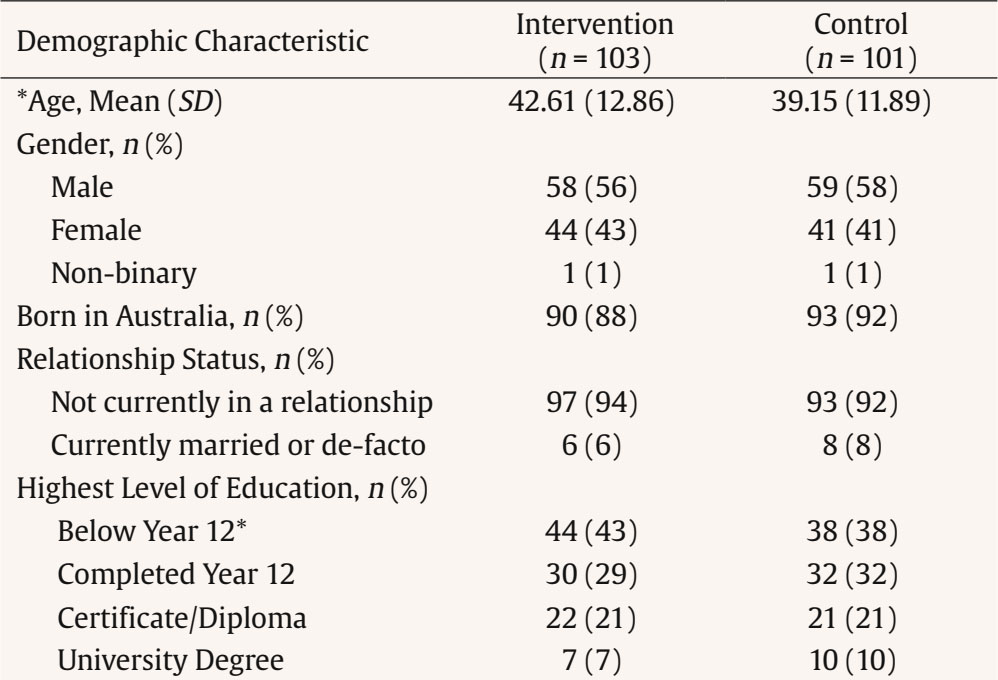 Note. SD = standard deviation. *p < .05. Key Findings Results of the multilevel modelling analyses for psychosocial functioning and clinical symptom severity are presented in Tables 2 and 3. Table 2 shows the mean (standard error) scores for participants on the BASIS and HoNOS, and the group x time interaction effects. Table 3 presents the post-hoc comparisons at Time 2 (midpoint) and Time 3 (closure) for outcomes where a significant interaction effect was identified. Paired t-test comparisons for intervention participants at six-month follow-up are presented in Table 4. Table 2 Intervention Effect: Interaction of Group by Time  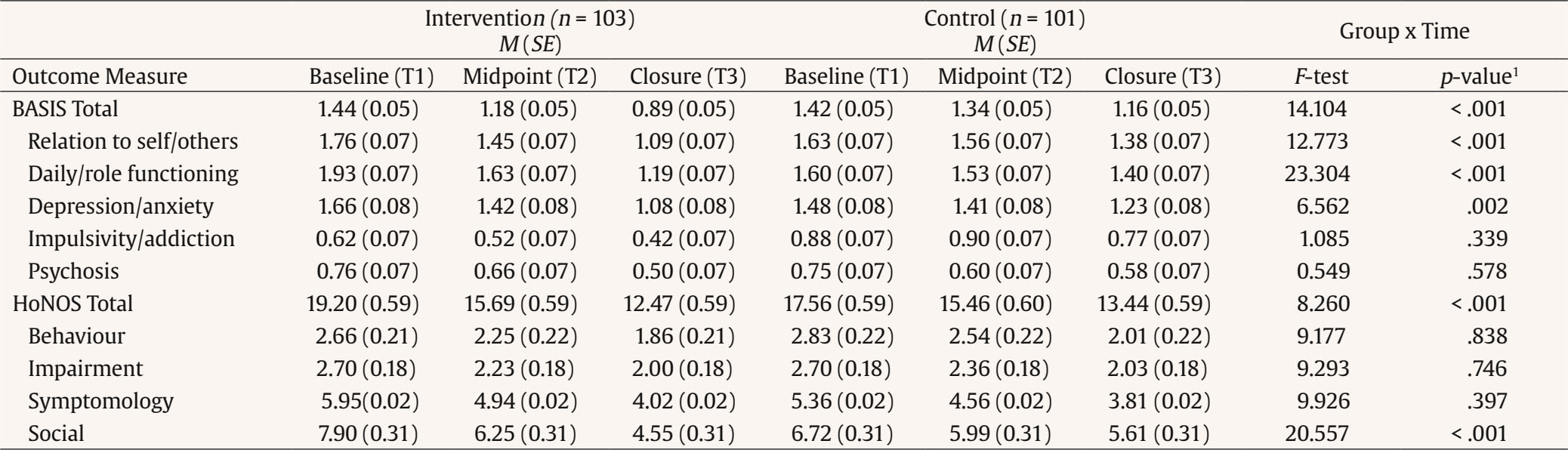 Note. M = mean; SE = standard error; Total N = 204 participants; T1 = Time 1 (baseline); T2 = Time 2 (midpoint); T3 = Time 3 (closure). 1Bonferroni correction applied with significance level set at .001. Table 3 Pairwise Comparisons between the Intervention and Control Groups  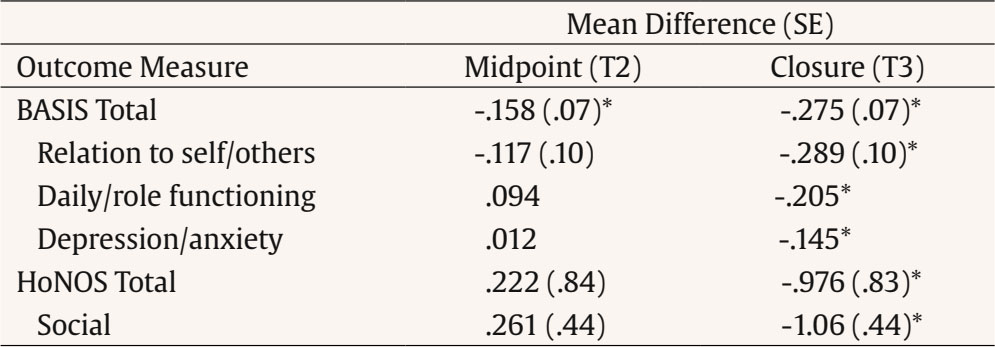 Note. Only outcomes with a significant interaction effect were included. * Statiscally significant, Bonferroni correction applied with significance level set at .01. SE = standard error; T2 = Time 2 (midpoint); T3 = Time 3 (closure). Table 4 Paired t-test Comparisons for Intervention Group between Closure (Time 3) and 6-month Follow-up (Time 4)  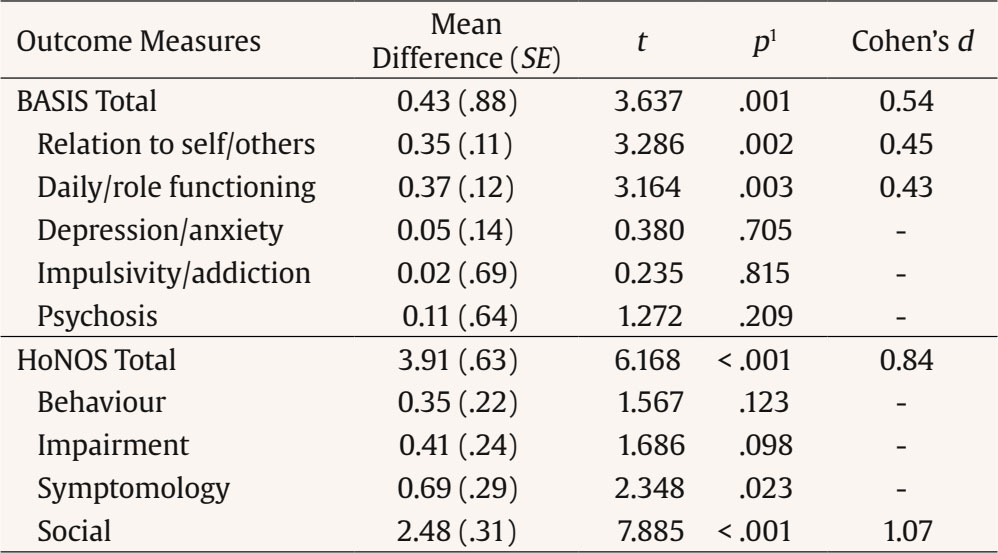 Note. N = 54, SE = standard error. 1Bonferroni correction applied with significance level set at .004. Psychosocial Functioning There was a significant group x time difference in participants’ total BASIS score (F = 14.104, p < .001). Post-hoc comparisons show that intervention participants reported significantly less difficulty in overall psychosocial functioning than the control group at Time 2 (program midpoint) and Time 3 (program closure), which is attributed to the intervention. There were significant interaction effects on three of the five BASIS subscales: relation to self and others, daily and role functioning, and depression/anxiety groups, (F = 20.577, p < .001). Post-hoc pairwise comparisons show that these differences were significant at closure (Time 3) only. Further, the effect of time was significant for all outcomes. Post-hoc comparisons demonstrated statistically significant mean decreases in scores for intervention participants across each timepoint for all psychosocial outcomes. The paired t-test comparisons between closure and six-month follow-up for intervention participants are presented in Table 4. Intervention participants experienced further improvement in their overall psychosocial functioning overall, as indicated by the BASIS total score with medium effect size, t(1, 53) = 3.637, p = .001, d = 0.54. Specifically, intervention participants had improved relationships with self and others, t(1, 53) = 3.286, p = .002, d = 0.45, and better daily/role functioning, t(1, 53)= 3.164, p = .003, d = 0.43, between program closure and 6-month follow-up. Clinical Symptomology There was a significant group x time difference in participants’ HoNOS total score, with a medium effect size (F = 8.260, p < .001, see Table 2). Post-hoc comparisons demonstrate that intervention participants had significantly lower clinical severity than the control group by closure (Table 3). Specifically, there was a significant difference in social functioning between groups, with a large group x time interaction effect size (F = 20.577, p < .001). By closure, intervention participants had significantly reduced social impairment compared to control participants, as shown in the post-hoc pairwise comparisons (Table 3). There were no other statistically significant differences between groups for the remaining HoNOS subscales. Nonetheless, the effect of time was significant across all outcomes except the impairment domain. Intervention participants experienced a significant reduction in scores from baseline to closure on all other subscales. At six-month follow-up (see Table 4), intervention participants experienced a significantly large reduction in their overall clinical severity, as indicated by the total HoNOS score, t(1, 53) = 6.168, p < .001, d = 0.84. Specifically, there was a significant improvement in participants’ social functioning between closure and six-month follow-up, with a large effect size, t(1, 53) = 7.885, p < .001, d = 1.07). There were no other significant differences on the remaining HoNOS subscales. Psychiatric Readmissions The rate of psychiatric readmissions in the six-months following program closure are presented in Table 5. There were no significant differences in the number of readmissions between groups: 7% of the intervention group and 9% of the control group experienced one readmission (χ2 = .316, p = .574). However, intervention participants had a statistically significantly shorter mean length of stay (M = 4 days), approximately six days less than the control group (M = 10 days), on average (t = -2.150, p < .05) Table 5 Psychiatric Readmission Outcomes between Groups at 6-months post-closure (Time 4)  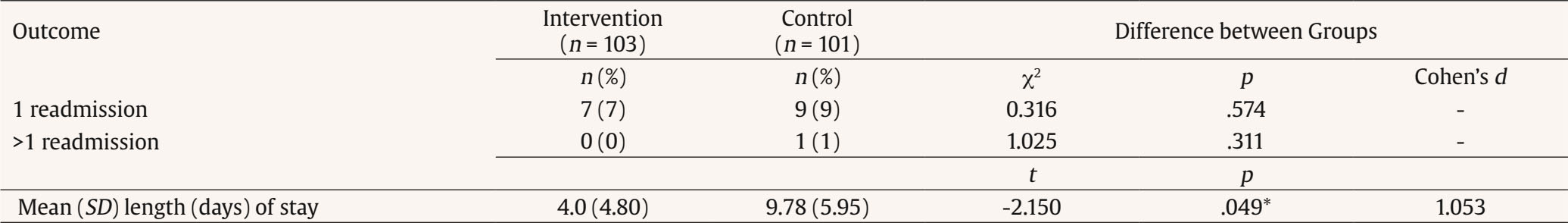 Note. SD = standard deviation *p < .05. This is the first longitudinal controlled evaluation of a psychosocial outreach support for individuals with SMI in Tasmania, Australia. The study evaluated the effectiveness of Baptcare’s Foundations program on adults’ psychosocial functioning, clinical symptomology, and hospital readmissions, in comparison to standard clinical care only. The hypothesis that the intervention group (Foundations) would experience significantly greater improvements in their psychosocial functioning in comparison to the control group was supported. There were no significant differences in clinical symptom severity or hospital readmission rates between groups. The findings demonstrate that the addition of wrap-around psychosocial support alongside clinical mental health care can yield significant improvements in psychosocial outcomes by program closure. In comparison to MHS only, clients who also engaged in Foundations achieved better overall social functioning, including improved self-esteem and self-confidence, increased social network or quality of social relationships, increased community and/or economic participation, including employment, volunteering, education or meaningful activities, and greater capacity to manage day-to-day activities (i.e., managing household responsibilities, cooking etc). These significant quantitative findings support previous anecdotes from staff and clients (O’Donnell, Ayton, et al., 2020). Stakeholders attribute such outcomes to key program components, including a persistent engagement strategy, relationship and trust with a consistent key practitioner, assertive outreach, long-term duration and a strength-based, goal-focused, and recovery-oriented tailored approach to support (O’Donnell, Ayton, et al., 2020). These components differentiate Foundations from MHS and traditional models of clinical mental health case management. For example, in comparison to MHS, the smaller caseloads of Foundations promote adaptability, flexibility, outreach, and more intensive support to facilitate clients’ achievement of their psychosocial goals, which aligns with recovery-oriented practice (van Weeghel et al., 2019). Additionally, at six-month follow-up, Foundations clients experienced further significant improvements across all outcomes related to social functioning. This demonstrates the sustainable longer-term effect of the program in building people’s capacity to live independently, strengthening relationships with others and themselves (i.e., self-esteem) and enhancing community participation, which are associated with improved quality of life (Sanchez et al., 2016). A unique finding was that differences between groups were more pronounced at program closure rather than at program midpoint. Both groups often experienced a comparable reduction in psychosocial severity in their first six months of program engagement. However, control participants plateaued in the second half of program engagement, whereas Foundations participants experienced further improvements that surpassed the control group by closure. This highlights the necessity of longer-term psychosocial support on a needs-led basis to achieve clients’ goals and yield sustainable changes above and beyond that of standard clinical care. It also demonstrates the strengthening of the relationship and trust between Foundations practitioners and clients over time, with a positive therapeutic relationship being the key determinant of engagement and positive outcomes among adults with SMI (Easter et al., 2015; McCabe & Priebe, 2004). Both standard clinical care and psychosocial support yielded significant reductions in participants’ clinical symptom severity over time. However, there were no significant differences between groups by program closure in externalising and internalising symptom severity, physical/cognitive impairment, impulsivity/addiction, or psychosis. This is likely because all participants were engaged with the same level of clinical care from MHS, including medication management and regular consultation with a multidisciplinary mental health team as required. Nonetheless by closure, intervention participants had reduced functional impairment associated with the symptoms of depression and anxiety and reduced overall clinical severity, in comparison to the control group. This demonstrates the added benefit of long-term wrap-around psychosocial support to addressing individuals’ unmet needs. Whilst this study has generated new evidence, there are some key limitations to acknowledge. The six-month follow-up findings are a unique strength of this study as there is a dearth of existing follow-up data among this population. However, we observed very high rates of attrition as approximately half of the intervention participants (48%) were uncontactable or declined to participate at the optional follow-up point, which may have positively skewed the current findings. The post-treatment attrition is consistent with previous literature, especially among participant groups with more severe mental illness (Liu et al., 2018). Future research could apply an opt-out consent process to service follow-up protocols, which may have increased the sample size for the current study. Further exploration of strategies to reduce attrition among individuals experiencing SMI is recommended. Secondly, measuring a recovery-oriented psychosocial-focused program with predominantly clinical measures may not provide a holistic representation of program impact. The HoNOS and BASIS were used as they are routinely completed by MHS and allowed comparison to a control group. To enhance program implementation and routine outcome measurement, a more holistic and recovery-oriented psychosocial outcome tool could be embedded into standard practice of the Foundations program. This will assist in capturing holistic outcomes that are more meaningful for clients and align more closely with the goals of the program. Further, it was not feasible to randomise participants due to the intervention referral process from MHS. It would have been unethical to withhold or delay participation in Foundations for participants referred to the psychosocial program. Therefore, participants were matched on key demographics that could have confounded the results, and baseline characteristics were controlled for during the analysis. Despite our efforts, there likely remained distinct disparity between groups, as other variables that were unable to be captured (e.g., previous admissions, previous service engagement, etc.), which provide greater insight into the severity and persistence of SMI that could have influenced the effectiveness of the intervention. Further, selection bias may have occurred as only those willing to engage in the research were included (87% of all potentially eligible clients). This likely imbalance between groups emphasises that the findings and conclusions drawn from this study must be interpreted with caution. The findings of this study revealed that psychosocial outreach can effectively support adults with SMI, highlighting the additional value of wrap-around, recovery-oriented, outreach support alongside clinical mental health care to improve adults’ psychosocial wellbeing. Being the first controlled evaluation of its kind in this state, this work makes a valuable contribution to the local Australian mental health literature. The findings strengthen the evidence base for the Foundations program and provide support for its ongoing implementation. There is potential for the program to be scaled-up in efforts to further reduce the demand on broader health and social care systems, and to ultimately continue enhancing the lives of adults experiencing SMI. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Savaglio, M., Vincent, A., Bentley, M., Gaul, J., Poke, S., Watson, N., & Skouteris, H. (2024). A controlled evaluation of a psychosocial outreach support program for adults with severe mental illness. Psychosocial Intervention, 33(3), 179-185. https://doi.org/10.5093/pi2024a12 Funding: This work was funded by Baptcare and conducted by Monash University. Authors AV, MB, JG, SP, and NW are employed by Baptcare. |
Cite this article as: Savaglio, M., Vincent, A., Bentley, M., Gaul, J., Poke, S., Watson, N., & Skouteris, H. (2024). A Controlled Evaluation of a Psychosocial Outreach Support Program for Adults with Severe Mental Illness. Psychosocial Intervention, 33(3), 179 - 185. https://doi.org/10.5093/pi2024a12
Correspondence: helen.skouteris@monash.edu (H. Skouteris).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS