
Which Psychosocial Strengths Could Combat the Adolescent Suicide Spectrum? Dissecting the Covitality Model
Raquel Falcó1, Samuel Falcon2, Beatriz Moreno-Amador1, Jose A. Piqueras1, and Juan C. Marzo1
1Miguel Hernández University, Elche, Alicante, Spain; 2University of Las Palmas de Gran Canaria, Spain
https://doi.org/10.5093/pi2024a9
Received 18 October 2023, Accepted 20 February 2024
Abstract
Objective: Covitality is a meta-construct of positive intra/interpersonal self-schemas that organize and process life experiences. Its synergy favors psychosocial adjustment and prevents mental health problems during adolescence. At these ages, suicide is one of the leading causes of death worldwide. The purpose of this study was to determine which psychosocial strengths of the covitality model could combat adolescent suicide spectrum. Method: Participants were 5,528 Spanish adolescents aged 12-18 years, 50.74% females. The assessment protocol was completed in schools, under the supervision of the research staff. Statistical analyses were conducted using hurdle models, i.e., modeling zero-inflated count data. This process provided two sets of outcomes: the association – in probabilistic terms – between psychosocial strengths and the absence of suicide indicators (i.e., non-occurrence) and the association of these assets – via regression coefficients – with increased experimentation (i.e., duration/quantity). Results: All psychosocial strengths of the covitality model were related to the non-ocurrence of suicidal thoughts and behaviors, but not all to a shorter duration/quantity of their phenotypic manifestations. Covitality obtained greater association values on suicidal tendencies than its components analyzed independently. Belief in self and engaged living were the second-order factors with the higher estimating capacity. Specifically, emotional self-awareness, enthusiasm, gratitude, family support, and behavioral self-control were key first-order assets. Conclusions: These findings suggest that training adolescents in covitality assets could be an effective strategy for universal prevention against premature suicide. Moreover, this study provide evidence on which psychosocial strengths could counteract each phenotypic manifestation of suicide in order to customize selective and indicated preventive actions.
Keywords
Suicide, Psychosocial strengths, Covitality, Adolescents, PreventionCite this article as: Falcó, R., Falcon, S., Moreno-Amador, B., Piqueras, J. A., & Marzo, J. C. (2024). Which Psychosocial Strengths Could Combat the Adolescent Suicide Spectrum? Dissecting the Covitality Model. Psychosocial Intervention, 33(3), 133 - 146. https://doi.org/10.5093/pi2024a9
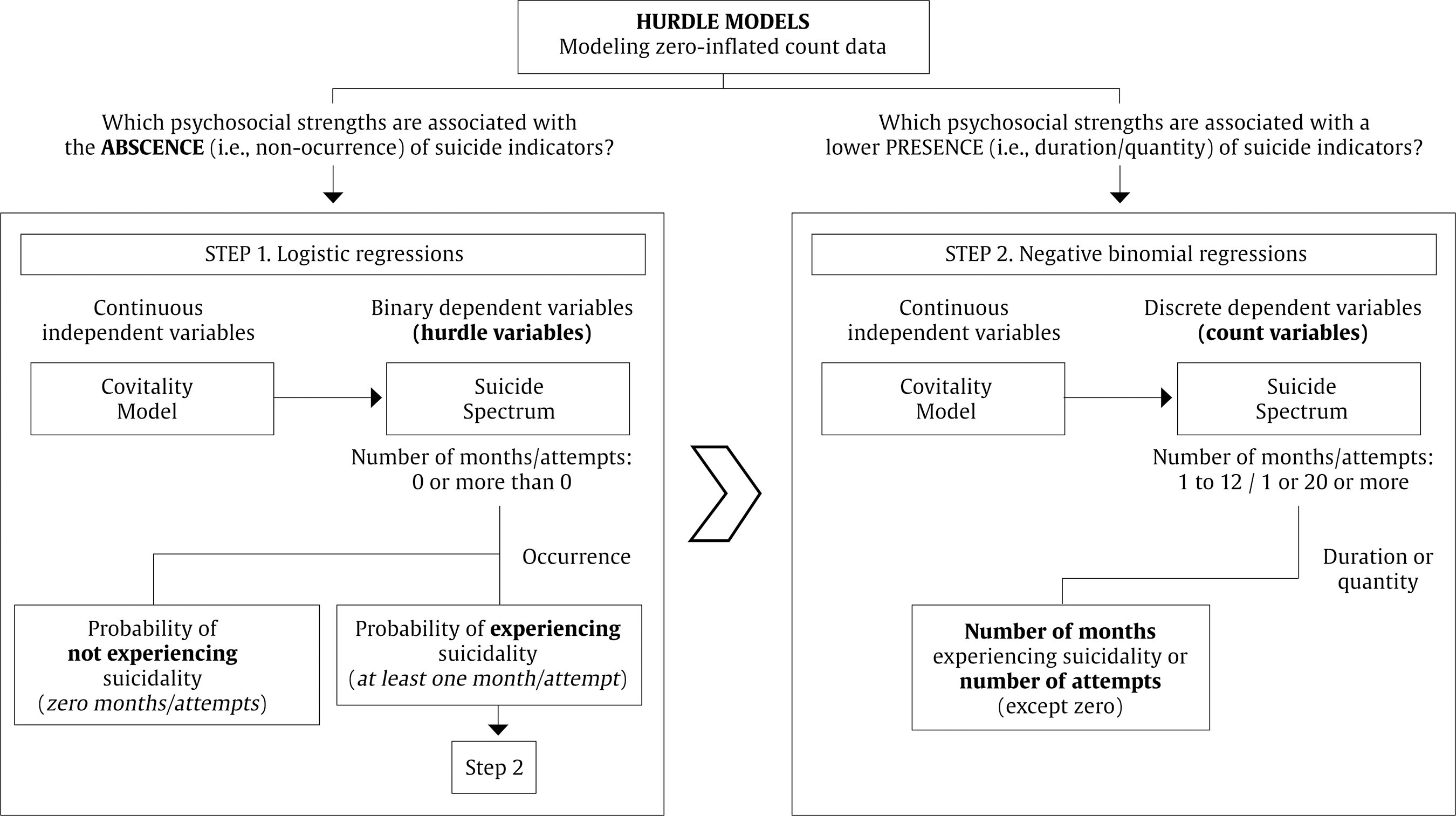
Correspondence: jc.marzo@umh.es (J. C. Marzo).The World Health Organization calls suicide prevention as a global imperative (WHO, 2014). This phenomenon claims more than 700,000 lives each year and represents the fourth leading cause of death among young people aged 15-19 years, although the official figures underestimate the true magnitude of the problem (WHO, 2023). Spain, for its part, reaches record highs for the fourth consecutive year and suicide constitutes the absolute leading cause of death among youth population (Instituto Nacional de Estadística [INE, 2023]). Although worrisome, these data are just the tip of the iceberg. Not exempt from complexity and controversy, the most accepted conceptualization of this phenomenon contemplates a spectrum with elements of different idiosyncrasies and growing intentionality, which go beyond the lethal act (García-Haro et al., 2023). Suicide is a polyhedral construct whose expression encompasses a dynamic continuum of ideation, planning, communication in life and autolytic act (Anseán, 2014; O’Connor & Nock, 2014). Figure 1 illustrates its structure and phenotypic composition. Thus, theoretically, the risk of suicide would be determined by the conjunction of the type of indicator and its level of intensity, frequency, and functional interference (O’Connor & Pirkirs, 2016). However, it should be noted that the scaling may not necessarily occur in a linear sequence, since the unpredictability of human behavior can lead to a leap from cognition to action (Fonseca-Pedrero & Pérez-Albéniz, 2020), not forgetting that multiple factors of a biological, psychological, clinical, social, and environmental nature converge and interact in the complex etiology of suicidal behavior (Al-Halabí & Fonseca-Pedrero, 2023; Turecki et al., 2019). Figure 1 Conceptual Delimitation of Suicide Spectrum.  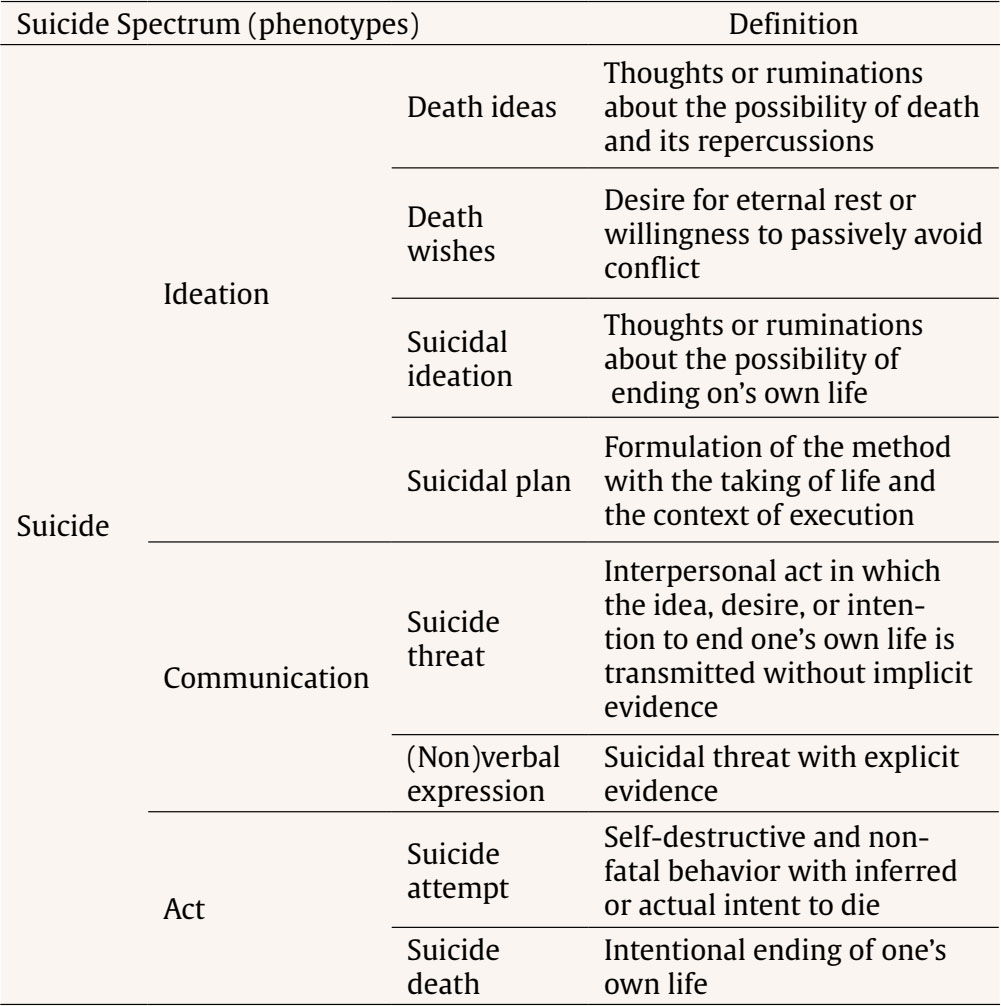 Figure adapted from Anseán (2014) and Fonseca-Pedrero and Pérez-Albéniz (2020). Psychology has developed numerous models and explanatory theories that try to elucidate the same question: why suicide? Zaldívar-Basurto et al. (2023) provide a comprehensive review, should it be of interest to the reader. In this study, the phenomenological-contextual model takes on special relevance (González-González et al., 2019; Michel, 2011). From this approach, suicidal behaviors are understood as limit-solutions to situations of existential crisis, rupture, and entrapment of the self with the world, with others and with oneself (Fonseca-Pedrero et al., 2022). The phenomenological vector of suicide resides inf a suffering experienced as intolerable, inescapable, and endless, for which the person sees no better solution than to end his or her own life (Al-Halabí et al., 2021). Therefore, the goal is not death, but to stop suffering. For quantifying the magnitude of the problem in the target population, Lim et al. (2019) compiled epidemiological publications on this topic grouping 686,672 children and adolescents in a meta-analysis. Lifetime prevalence was 18% for ideation, 9.9% for planning, and 6% for suicide attempts, while past 12-month prevalence was 14.2%, 7.5%, and 4.5%. At the Spanish scope, Fonseca-Pedrero et al. (2020) obtained figures of up to 17.8%, 5.9%, and 3.7%, respectively. Both reference publications provide pre-pandemic data, so considering the recent and notable increase in the number of suicide deaths worldwide, the forecasts point to an even greater trend. Moreover, this developmental stage is considered critical for the onset of mental health problems in general, and suicide in particular (Solmi et al., 2022). Key etiological factors (Fusar-Poli, 2019) and first suicidal thoughts and behaviors (Alqueza, 2023) usually emerge during early adolescence, while the abrupt growth of such manifestations occurs in mid-late adolescence (Voss et al., 2019). Similarly, research suggests that starting age (Thompson et al., 2012) and the premature presence of suicidal elements (Castellví et al., 2017) assume a prodromal and exacerbating character on the suicide risk in later stages. It seems clear that preventive efforts should be directed with more emphasis on this collective. Meantime, only 38 countries have a comprehensive national suicide prevention strategy, and Spain is not among them. For this reason, WHO (2021b) has published a practical guide for its design called ‘Live LIFE’, which lists the key effective evidence-based interventions: ‘L’, limit access to means of suicide; I, interact with the media on responsible reporting; ‘F’, foster socioemotional life skills among adolescent population (aged 10-19); and ‘E’, early identify, assess, manage, and follow up anyone who is affected by suicidal ideation and behavior. Focusing on action strategy ‘F’, the “Helping adolescents thrive Toolkit-guidelines” (WHO, 2021a) proposes specific training on intra- and interpersonal skills, positive personal beliefs about oneself, adaptative coping styles, and social support. Thus, the question arises as to whether a unitary model that integrates these psychosocial strengths could combat youth suicide: the covitality model. In the framework of positive psychology, the concept of covitality was originally born as a counterpoint to psychopathological comorbidity. Thus, covitality represents a meta-construct of positive intra- and interpersonal self-schemas that organize and process life experiences (Paz & Kim, 2022). The co-disposition and synergy of these assets favors psychosocial adjustment and prevents mental health problems during adolescence (Weiss et al., 2002). Based on scientific literature, Furlong et al. (2014) selected the psychosocial strengths with the strongest empirical support and designed the covitality model. Conceptual underpinnings are found primarily in social psychology (e.g., Lips, 1995), self-concept theory (Chi-Hung, 2005), and cognitive therapy (e.g., Dozois et al., 2012; Young et al., 2003) research. It also integrates facets of preexisting models, such as those of emotional intelligence or resilience, among others (Furlong et al., 2020; Furlong et al., 2014). As a result, the structure and composition of this hierarchical model contemplates 12 factors first-order latent factors, grouped into 4 second-order, and a general higher-order (i.e., covitality): 1) belief in self – self-efficacy, self-awareness, and persistence; 2) belief in others – school support, family support, and peer support; 3) emotional competence – emotional regulation, empathy, and self-control; and 4) engaged living – optimism, enthusiasm, and gratitude. Renshaw et al. (2014) provide a discussion of the empirical merit of each of the 12 positive psychological dispositions. Figure 2 contains a brief definition of constructs. Figure 2 Hierarchical Model of Covitality: Construct Definitions.  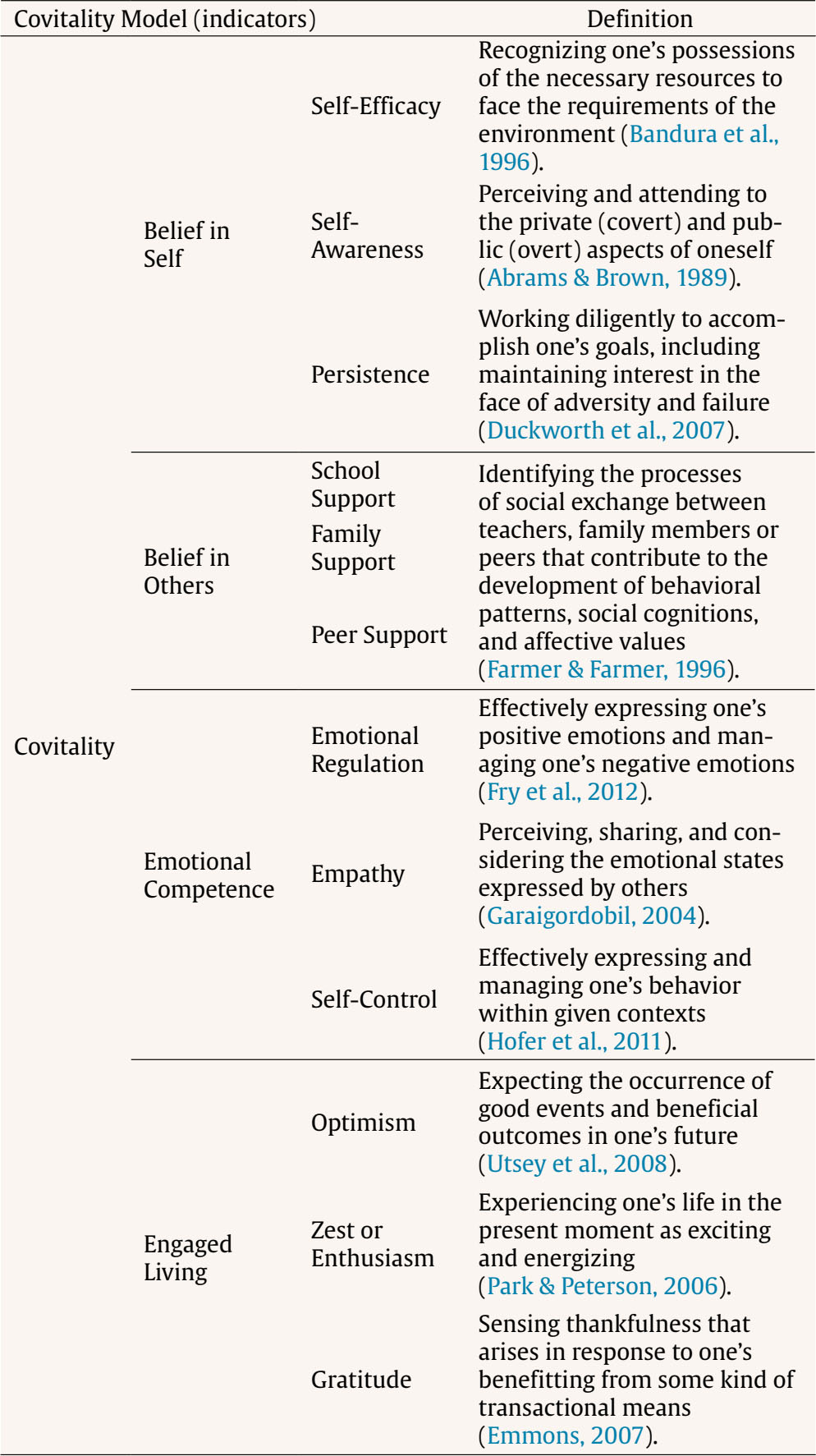 Figure adapted from Renshaw et al. (2014) and Rebelez-Ernst (2015). The evidence accumulated among large samples of adolescents from different countries indicates that covitality is an excellent predictor of positive mental health, in terms of subjective well-being (e.g., Telef & Furlong, 2017), prosocial behavior (e.g., Piqueras et al., 2019), successful academic performance (e.g., Arslan, 2019), health-related quality of life and life satisfaction (e.g., Kim et al., 2017). In contrast, a deficit of these personal resources has been linked to multitude of undesired situations, such as learning difficulties (e.g., Carnazzo et al., 2019), school absenteeism (e.g., Wroblewski et al., 2019), problematic use of the Internet and social networks (e.g., Marino et al., 2018), victimization in bullying dynamics (e.g., Fullchange & Furlong, 2016), membership in criminal gangs (e.g., Lenzi et al., 2019), internalizing and externalizing problems (e.g., You et al., 2014), substance use (e.g., Lenzi et al., 2015), and feelings of loneliness (e.g., Wang et al., 2021), among others. However, the study of covitality and suicide during adolescence is still in preliminary stages. The findings are incipient, and the approach is limited to suicidal ideation. Thus, correlation analyses show a negative association of weak-moderate magnitude (Larson, 2021). Probabilistic models indicate that a greater number and variety of psychosocial strengths, with equal configuration, reduce suicidal ideation (Lenzi et al., 2015). In addition, moderation analyses suggest that covitality significantly mitigates the impact of bullying on suicidal thoughts among sexual and gender minorities (O’Malley et al., 2021) or foster youth (Larson, 2021). To the best of our knowledge, this is the only evidence available. The Present Study At this point, there are unaddressed issues that would have important practical implications for youth suicide prevention. For example, clarifying which psychosocial strengths play a more determinant role in the face of each phenotypic manifestation of suicide would allow the design of more focused and personalized interventions. Besides, differentiating between the inhibitory and buffering effects of these assets could lay the basis for a multilevel action strategy (universal, selective, and indicated). Therefore, the purpose of this study was to elucidate which psychosocial strengths of the covitality model could combat the adolescent suicide spectrum. The appropriateness of the statistical methodology to the suicidological data set (Leikfer et al., 2021) led to the operationalization of this objective into a double research question: 1) which psychosocial strengths are associated with the ABSENCE (i.e., non-occurrence) of suicide indicators? and 2) which psychosocial strengths are associated with a lower PRESENCE (i.e., duration/quantity) of suicide indicators? The paucity of scientific literature on this topic prevented the establishment of evidence-based hypotheses, so the present study adopted an exploratory character. However, considering precedents, the authors expected that the link between psychosocial strengths and the suicide spectrum would be negative and that covitality would present a stronger association than its components analyzed independently. Participants and Procedure This study followed a quantitative, observational, descriptive-correlational, and cross-sectional methodology. Its multicenter design required a non-probabilistic quota sampling to ensure the representativeness of the adolescent community population in two areas of southeastern Spain: Province of Alicante and Region of Murcia. Thus, 100 secondary schools were contacted via e-mail, telephone, and in person; 34 finally agreed to collaborate. Their teaching staff disseminated information material about the research project. Student participation required fulfillment of 2 inclusion criteria: 1) providing the double informed consent of parents – or legal guardians – and adolescents; and 2) showing an optimal level of understanding of the Spanish language. The sample retention rate was 85%. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Prior approval was obtained from the ethics committee of Miguel Hernández University (DPS.JPR.02.17). Written informed consent was compiled from all participants and their parents or legal guardians. Data collection was conducted from group to group in digitized classrooms of schools. The assessment protocol was answered individually through the LimeSurvey© app, which presented a mandatory response system, in an average time of 20 minutes. Research staff conducted this process on-site, and guaranteed the minors’ voluntariness, pseudo-anonymity, and confidentiality. Student participation was not incentivized, although educational centers and regional secretariats of both territories received a descriptive report about adolescent mental health status. Besides, the legal, ethical, and deontological regulations on the detection and early care of minors at suicide risk led to the adoption of an interdisciplinary action protocol. For more detailed information about procedural aspects, see Falcó, Piqueras et al. (2023). Initial recruitment reached a total of 5,741 students in Compulsory Secondary Education, Baccalaureate, and Vocational Training, according to the Spanish educational system. Subsequently, 213 cases (3.7%) were excluded due to unfinished surveys, so the final sample was composed of 5,528 adolescents aged 12 to 18 years old (M ± SD = 14.20 ± 1.53). Table 1 shows its sociodemographic characteristics. Table 1 Sociodemographic Characteristics of the Sample  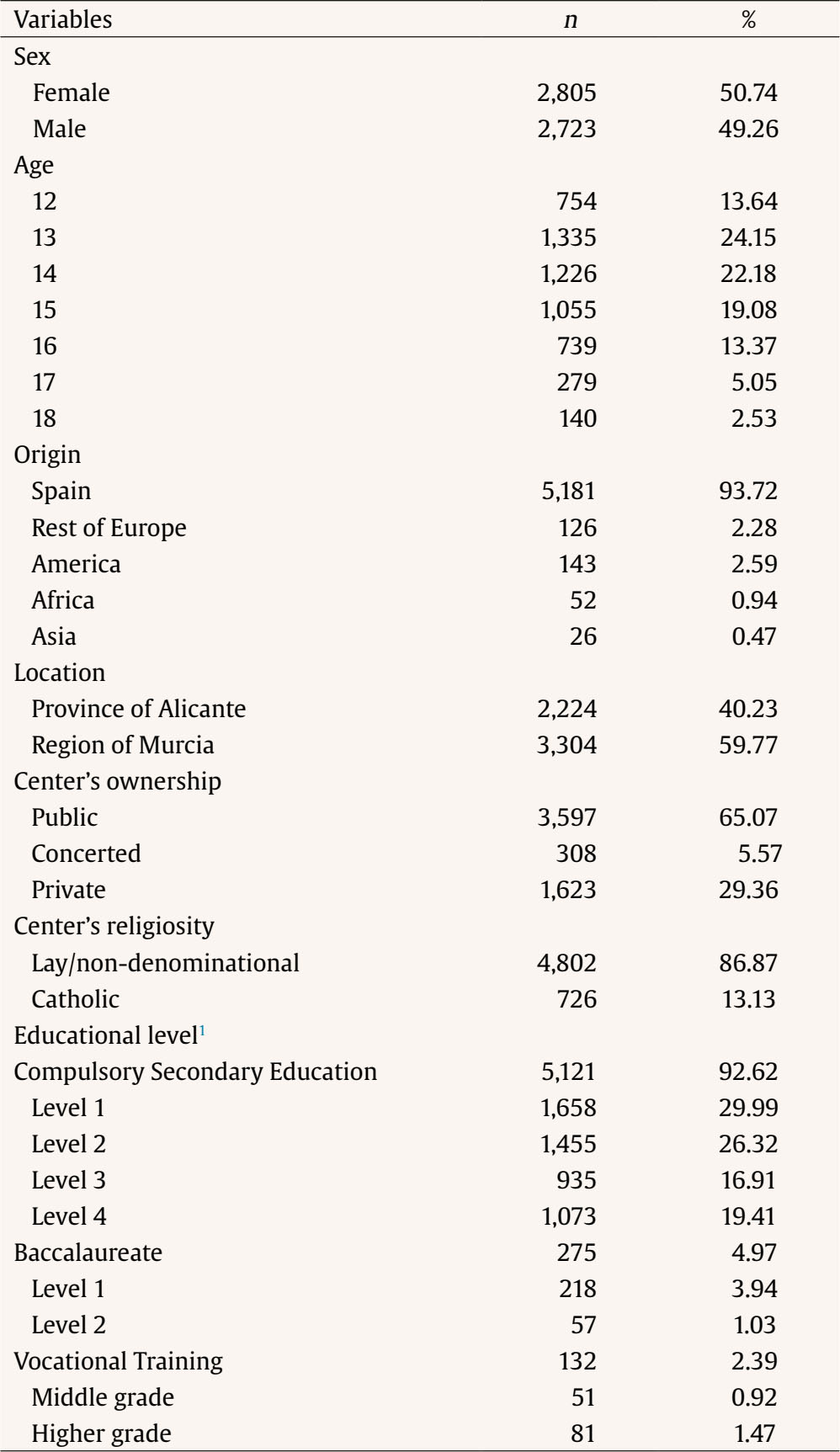 Note. Total sample: N = 5,528. 1According to the Spanish Educational System. Measures Adolescent Psychosocial Strengths The authors administered the Spanish version (Piqueras et al., 2019) of the Social Emotional Health Survey-Secondary (SEHS-S; Furlong et al., 2014) for the specific assessment of the psychosocial strengths that encompass the covitality model. This is a self-report instrument designed for adolescents aged 12-18 years. It contains 36 items – i.e., 3 for each of the 12 first-order factors – and presents a 4-point Likert-type response scale, according to the degree of identification with the listed intra- and interpersonal self-schemas (1 = not true at all, 4 = totally true). Some items that exemplify the 12 explored constructs: “I am able to solve my problems” (i1, self-efficacy), “I understand why I do what I do” (i6, self-awareness), “When I don”t understand something, I ask the teacher again and again until I understand it” (i7, persistence), “At my school there is a teacher or other adult who wants me to do my best” (i10, school support), “My family feels united” (i14, family support), “I have at least one friend my age who really cares about me” (i16, peer support), “I assume the consequences of the things I do” (i19, emotional regulation), “I feel bad when they hurt someone”s feelings” (i22, empathy), “I am able to accept when I get a «no» for an answer” (i25, self-control), “Normally I hope to have a good day” (i29, optimism), “Most days I feel energized (i31, enthusiasm) and “I feel grateful for many things in my life” (i36, gratitude). Composite scores were subsequently created for SEHS-S scales by averaging items. Adolescent Suicide Spectrum For the measurement of the indicators of the adolescent suicide spectrum, the authors elaborated an ultra-brief self-report selecting 5 core items from the Self-Injurious Thoughts and Behaviors Interview (SITBI; Nock et al., 2007) and the Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2011) in their Spanish versions (Al-Halabí et al., 2016; García-Nieto et al., 2013). These indicators were death wishes, suicidal ideation, determination of a suicide method, design of a detailed suicide plan, and suicide attempts. The items examined their manifestation during the past 12 months using a time-based response scale – duration from 0 to 12 months ; except for suicide attempts, where the informant reported the number of times – quantity from 0 to 20 or more suicide attempts. Moreover, an additional response alternative was included due to the sensitive nature of the information examined, “prefer not to say”, whose clinical implications have been analyzed in a previous study (Falcó, Piqueras et al., 2023). For this manuscript, its selection was recodified to a missing value. Before processing the dataset, the reliability of the scales was estimated using Cronbach’s alpha (α; Cronbach, 1951) and McDonald’s omega (ω; McDonald, 1999), considering > .70 as the criterion value for an optimal internal consistency (Gu et al., 2017). Descriptive statistics of the measures were also analyzed using parameters of central tendency, dispersion, and distribution of the sample, reported in Table 2. Table 2 Descriptive Statistics of the Data Set  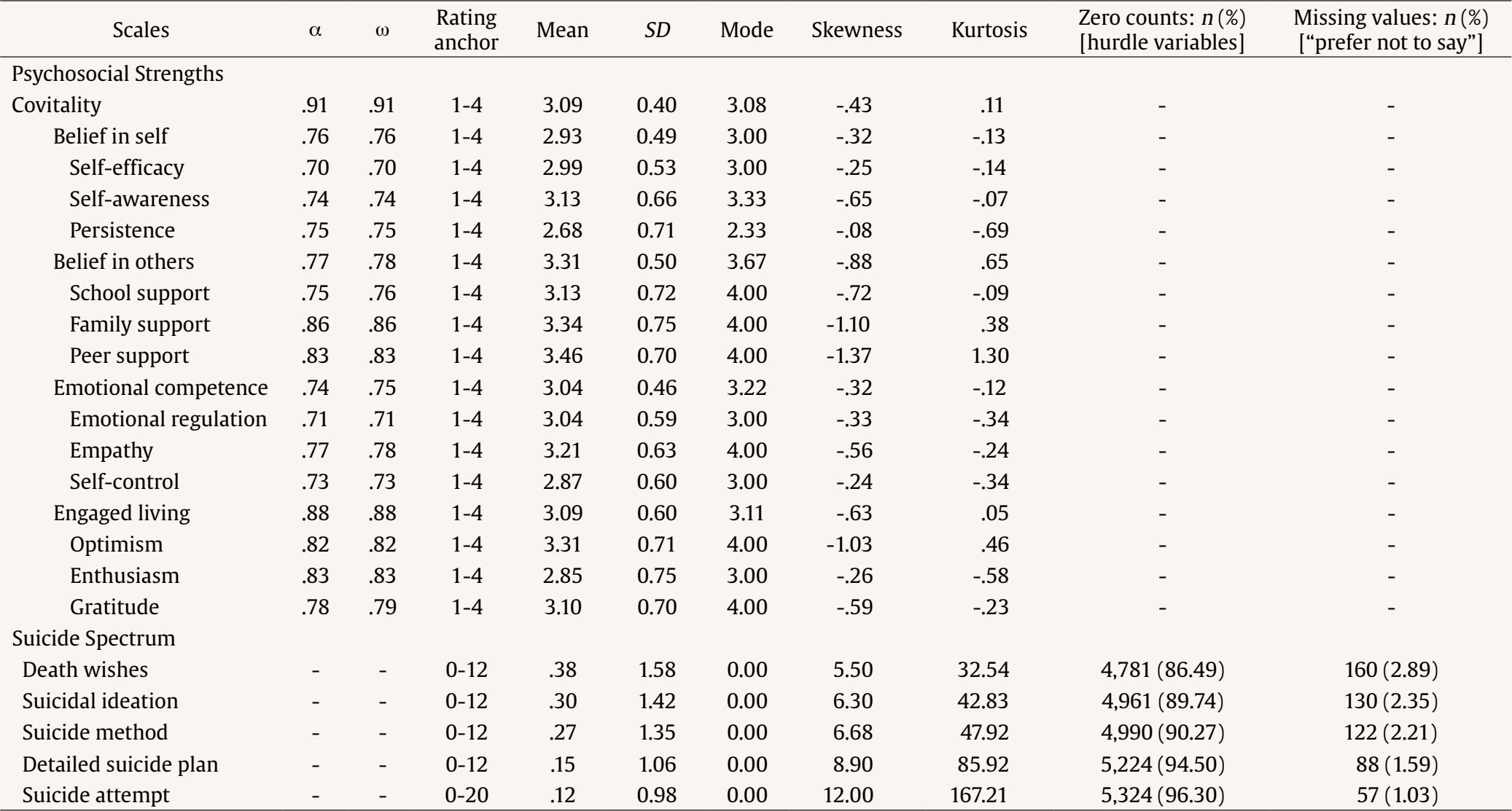 Note. Total sample: n = 5,528. α = Cronbach’s alpha; ω = McDonald’s omega; SD = standard deviation; - = not applicable. Data Analysis The descriptive statistic of the suicide spectrum showed a zero-inflated percentual distribution which divided the sample into two differentiated groups: adolescents with absence (= 0 months/attempts) or presence (> 0 months/attempts) of suicide indicators during the past year. Thus, the authors opted to test hurdle models (Cragg, 1971; Hu et al., 2011), a methodology especially recommended in suicidology since the outcomes are often count variables and have an unusually large number of zeros in their sampling distributions (Leikfer et al., 2021). Some authors suggest that this accounting for the truncation of the response variables provides more accurate estimates of regression coefficients (e.g., Yang et al, 2017). Figure 3 illustrates the hurdle models’ application to the present study’s double objective. The modeling transformed the dependent variable – i.e., each suicide indicator – into two new variables: a hurdle variable and a count variable (Muthén & Muthén, 2023). The first was a binary variable in which 1 denoted that an individual could not assume any value except zero: i.e., 0 months experiencing suicidality or 0 suicide attempts (never). The second was a discrete variable that include only individuals who could assume values of one or more: i.e., from 1 to 12 months experiencing suicidality or from 1 to 20 or more suicide attempts (at least one). Then, a logistic regression was performed with the hurdle variable and a negative binomial regression with the count variable. In this way, hurdle models provided two sets of estimates (Moffatt, 2005). The first equation sought to answer RQ1: “Which psychosocial strengths are associated with the ABSENCE (i.e., non-occurrence) of suicide indicators?”. Logistic regressions described how independent variables were associated with the likelihood of reporting a zero-response compared to a nonzero response (0 vs. any score > 0) on the outcome variable. In other words, they determined the probability of experiencing or not suicidal thoughts and/or behaviors in the past year - i.e., occurrence - according to the level of each psychosocial strength of the covitality model. The outcomes were represented by odd ratios (OR) and significance was determined using 95% CI that did not contain 1. In the case of having experienced suicidality during the last 12 months, the second equation sought to answer RQ2: “Which psychosocial strengths are associated with a lower PRESENCE (i.e., duration/quantity) of suicide indicators?”. Negative binomial regressions described the association between independent variables and the likelihood of reporting higher scores on the outcome for the group of participants that did not report zero-response on this variable (> 0). Thus, in case of having experienced suicidal tendencies during the last year, they determined the number of months or attempts – i.e., duration or quantity – again considering the levels of psychosocial strength of the covitality model. The outcomes were represented by regression coefficients (β), and statistical significance was determined using 95% CI that did not contain 0. The effects of sex and age were controlled in both equations as covariates because of differences observed in previous studies (e.g., Falcó et al., 2020; Falcó, Santana-Monagas, et al., 2023). No missing values were obtained per se because the configuration of the app prevented the recording of blank items, but the response option “prefer not to say” to the suicide questions was considered as such. Consequently, the percentage of missing values was minimal considering the sample size (see Table 2) and was handled using the full information maximum likelihood estimator. This estimation method retrieves bias even when data are not missed at random (Little et al., 2014). Moreover, the analysis of outliers was previously performed by means of the graphical representation of the frequency distribution (i.e., box plots), although the authors decided not to remove them from the sample for reasons of ecological validity. The analysis plan was conducted using Mplus 8.7 software (Muthén & Muthén, 2023). Which Psychosocial Strengths are Associated with the ABSENCE of Suicide Indicators? Table 3 presents the outcomes of the logistic regressions that constitute step 1 of the hurdle models. Even controlling for the effect of the sociodemographic covariates, all psychosocial strengths of the covitality model were significantly associated with the absence of all indicators of the suicide spectrum. The higher the level of these assets, the greater the likelihood of not experiencing suicidal thoughts and behaviors during the past year. Surprisingly with one exception: empathy. The inverse probability warned that it was associated with the occurrence of death wishes (OR = 1.18) and suicide attempts (OR = 1.45). Table 3 Hurdle Models – Step 1: Which Psychosocial Strengths Are Associated with the ABSENCE (non-occurrence) of Suicide Indicators?  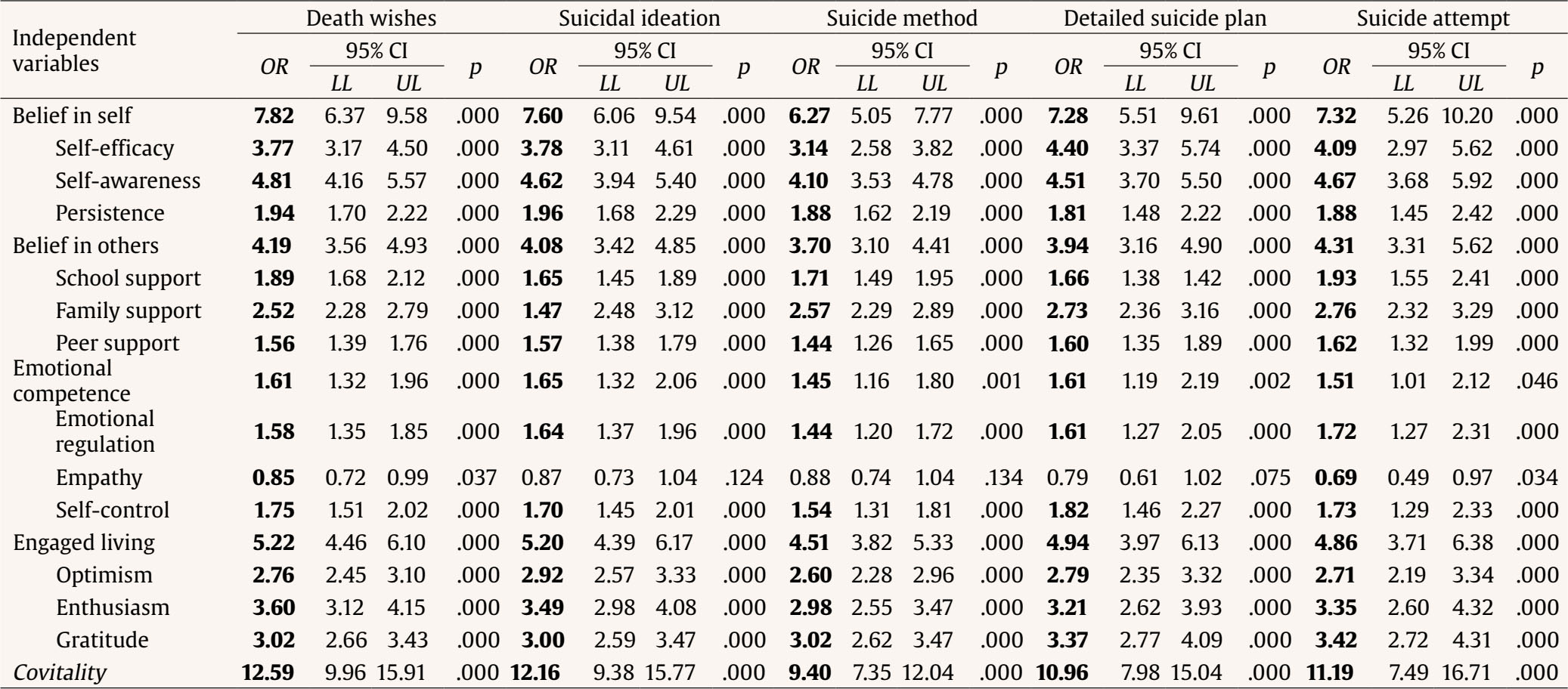 Note. Significance level: p < .05 or 95% CI that does not contain 1 (OR). OR = odd ratio; CI = confidence interval; LL = lower limit; UL = upper limit. The effects of sociodemographic covariates are available in the supplementary material (Appendix). Covitality, as representative of the co-disposition and synergy of psychosocial assets, was undoubtedly the variable that presented the stronger association with all levels of suicidality. From highest to lowest probabilistic power, the second-order factors were belief in self, engaged living, belief in others, and emotional competence. Emotional self-awareness, enthusiasm, family support, and behavioral self-control stood out among their corresponding first-order factors. It should be mentioned that the probability values did not seem to respond to a pattern of association proportional to the level of severity of each suicide spectrum indicator. Which Psychosocial Strengths are Associated with a Lower PRESENCE of Suicide Indicators? Table 4 shows the outcomes of the negative binomial regressions that make up step 2 of the hurdle models. In this case, not all psychosocial strengths of the covitality model were significantly associated with a lower presence of all indicators of the suicide spectrum. In general, the higher the level of these assets, the shorter the period experiencing suicidal thoughts and behaviors, or the lower the number of attempts, during the past year. Table 6 Hurdle Models – Step 2: Which Psychosocial Strengths Are Associated with a Lower PRESENCE (duration/quantity) of suicide indicators?  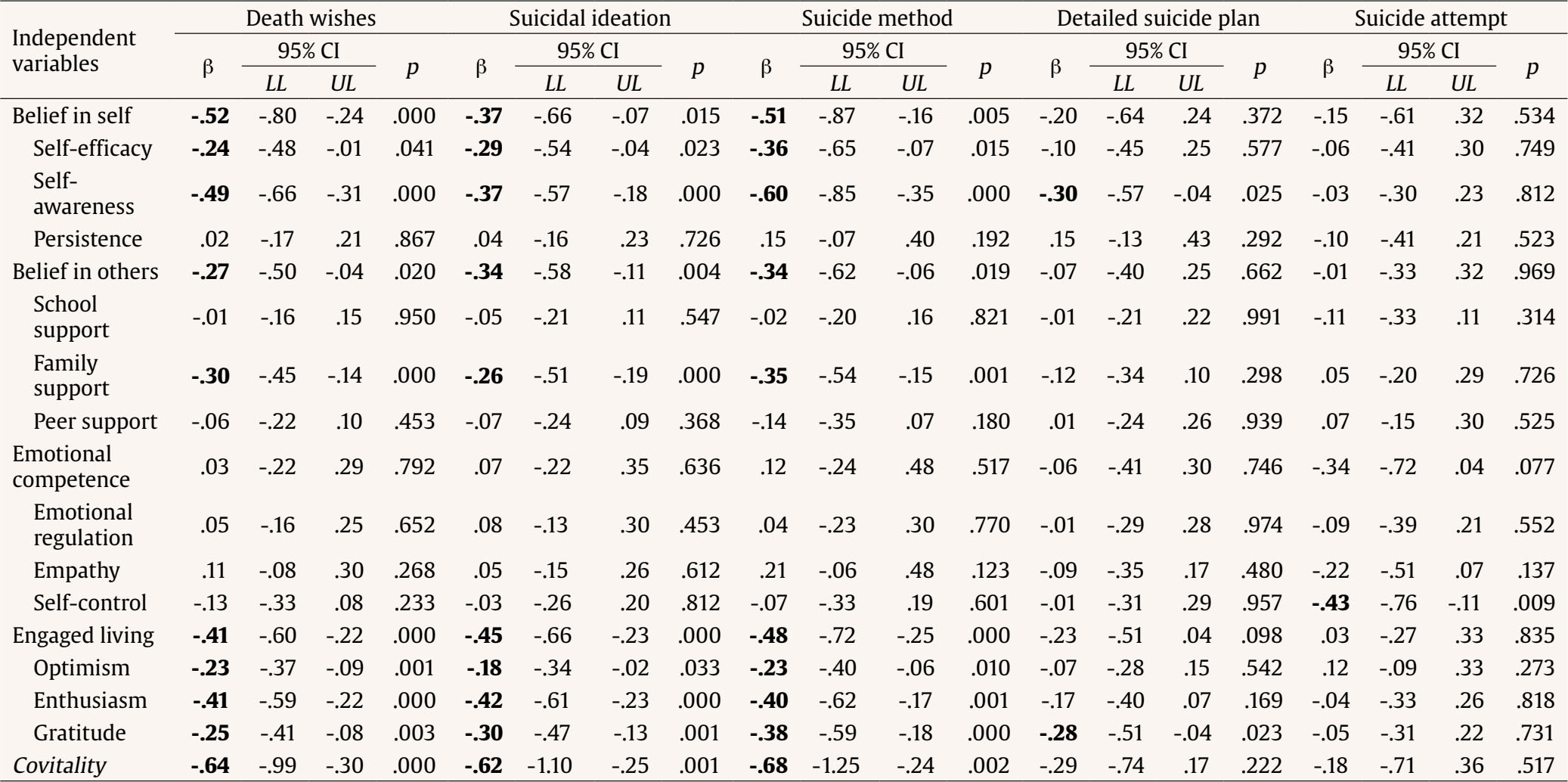 Note. Significance level: p <.05 or 95% CI that does not contain 0 (β in bold type); β = standardized coefficient; CI = confidence interval; LL = lower limit; UL = upper limit. The effects of sociodemographic covariates are available in the supplementary material (Appendix). Covitality was again the most outstanding variable, being significantly associated with a shorter temporal extent of death wishes, suicidal ideation, and determination of the suicide method. Specifically, belief in self, engaged living, and belief in others were the second-order factors that were significant for these suicide indicators, in decreasing order of associative value. Levels of emotional self-awareness, enthusiasm, and family support were respectively key strengths. Notably, gratitude and emotional self-awareness were also variables significantly related to less time spent elaborating a detailed suicide plan, while behavioral self-control was the only psychosocial strength linked with a significant decrease on the number of suicide attempts. The purpose of this study was to elucidate which psychosocial strengths of the covitality model, as independent assets, could most combat the adolescent suicide spectrum. Adopting an exploratory approach, the adequacy of the statistical methodology to the suicidological dataset allowed to obtain a double estimation: to distinguish between their association with the absence vs. the presence of suicide indicators. In the following, the main findings are again described in detail and their comparison with the available literature is discussed. First, positive intra/interpersonal self-schemas associated with the non-occurrence of suicidal thoughts and behaviors were identified. The results were unanimous, and all assets were positively and significantly associated with the probability of not developing any suicidal phenotype, with one exception, empathy, a facet related to the onset of death wishes (OR = 0.85) and suicide attempts (OR = 0.69). These findings are consistent with the study by Fonseca-Pedrero et al. (2020), which presents an etiological network analysis of adolescent suicide and considers both risk and protective factors. These authors conclude that depressive symptomatology, positive affect, and empathic concern assume a nuclear role regarding strength, while self-perceived emotional intelligence is the most influential node in the network of interconnections. In the same line, Falcó et al. (2020) conducted predictive models between the psychosocial dispositions of the covitality model and affective-behavioral psychopathology, finding a positive link between empathy and internalizing symptoms (i.e., anxious-depressive). The analogy between publications suggests that this attribute maintains a non-linear connection with undesirable psychological phenomena, such as psychopathology and suicide, so that optimal levels provide protection and high levels vulnerability/risk. Although empathy appears to be a common ingredient in school-based social-emotional health interventions, experts suggest targeting training techniques to moderate the affective system (i.e., the ability to reflect and feel another person’s emotional state), avoiding overstimulation, and to enhance the cognitive system (i.e., the capacity to recognize and understand it intellectually) (e.g., Fullchange, 2022). Likewise, covitality – as a co-disposition of the strengths set – was the variable with the highest estimation power for all levels of suicidality (OR = 9.40-12.59). Not surprisingly, this data reinforces the conceptual foundations of the model that the research has subsequently validated. This basis establishes a parallelism between the “covitality” metaconstruct and the hypothesized “g” factor of intelligence, also alluding to the principle of holism in words of Aristotle: “The whole is greater than the sum of its parts” (Furlong et al., 2014; Renshaw et al., 2014). Thus, the creators of the model suggested that the combination of psychosocial strengths would have a greater impact on mental health than their isolated components. Lenzi et al. (2015) provided evidence in this regard noting that the configuration of the hierarchical model had important implications on its defensive role against suicidal ideation in adolescents, in terms of quantity (OR = 0.17 to 0.88), variety (OR = 0.40 to 0.88), and intra/interdomain equality (OR = 0.29 to 0.71). However, the results reflected a dysmorphic contribution in this regard. Positive beliefs about oneself (OR = 6.27-7.82) and about life (OR = 4.51-5.22) showed a stronger association than the perception of social support (OR =3.70-4.31) and the disposition of socioemotional skills (OR = 1.45-1.65) against the genesis of suicide. Specifically, emotional self-awareness (OR =4.10-4.81), perceived self-efficacy (OR = 3.14-4.40), enthusiasm (OR = 2.98-3.60), and gratitude (OR = 3.00-3.42) led as key attributes among their first-order factors. It is worth mentioning that the magnitude of association with each suicidal phenotype does not seem to obey a pattern of severity or lethality. Taken together, these findings teleport us to Baumeister’s (1990) motivational theory, conceptualized under the contextual-existential approach to suicidal behavior (González-González et al., 2019; Michel, 2011). From this perspective, the causal chain begins with a combination of self-perceived inefficacy – i.e., rupture of the self with itself – and lack of vital meaning – i.e., rupture of the self with the world, leading to a state of “aversive self-consciousness”, traditionally known as a sense of defeat and entrapment (O’Connor & Kirtley, 2018) or hopelessness (Beck, 1986). Against such suffering, the person tries to reach a state of cognitive deconstruction that brings with it irrationality and disinhibition, which makes drastic measures seem acceptable and suicide can be contemplated as an escape route. Therefore, in response to the first research question, it seems justified to bet on a pilot training program in all components of the covitality model as a universal prevention method against (adolescent) suicide, focusing especially on the promotion of positive beliefs about oneself and about life. Moreover, based on the conclusions of the PSICE project – Psychology based on Evidence in Educational Contexts – we can affirm that the schools are the preferred setting for implementing this type of protocolized actions (Fonseca-Pedrero, Díez-Gómez, Pérez-Albéniz, Lucas-Molina, Al-Halabí, et al., 2023). Renowned authors, such as Garaigordobil (2023), advocate making every school a center for the fostering of mental health, assuming services for the promotion of psychological well-being and the prevention of psychopathology and suicide during childhood and adolescence. Fonseca-Pedrero Díez-Gómez, Pérez-Albéniz, and Lucas-Molina (2023) provide an exhaustive review of the main strategies for preventing adolescent suicidal behavior in educational context, including a compilation of evidence-based programs for training some of these competencies. Second, positive intra/interpersonal self-schemas associated with a lower presence (i.e., duration/quantity) of suicidal thoughts and behaviors were identified. On this occasion, not all the strengths took an active role. Covitality was again the variable with the greatest magnitude of association, although only with a lower temporal extent of suicidality in its initial stages (β = from -.62 to -.68). Belief in self (β = from -.37 to -.52), engaged living (β = from -.41 to -.48), and belief in others (β = from -.27 to -.34) were the second-order factors, related to a lower presence of death wishes, suicidal ideation, and choice of a suicide method, with emotional competence remaining in the background (p > .05). Again, self-awareness (β = from -.37 to -.60), self-efficacy (β = from -.24 to -.36), enthusiasm (β = from -.40 to -.42), and gratitude (β = from -.25 to -.38) stood out as key attributes for the above-mentioned suicidal elements, with family support (β = from -.26 to -.35) and optimism (β = from -.18 to -.23) joining the list. These data continue to point in the same direction, corroborating the literature described above and providing two new findings. On the one hand, it emphasizes the importance of granting social support, especially family support, when the adolescent has begun to experience suicidality (e.g., Soto-Sanz et al., 2019). A recent study shows that the parental style based on rejection and indifference is positively related to adolescents’ silence during bullying dynamics and even to suicidal ideation (Estévez-García et al., 2023). And, on the other hand, it warns of the limited action of covitality to the mildest phenotypic manifestations of suicide. This implies that selective or indicated prevention requires the simultaneous adoption of other evidence-based strategies beyond the promotion of psychosocial strengths. For example, community-level screening and monitoring, gatekeeper training, limiting access to means of suicide, and/or individual psychotherapy, among many others (e.g., Fonseca-Pedrero Díez-Gómez, Pérez-Albéniz, Lucas-Molina, Al-Halabí, et al., 2023). However, it is worth highlighting that gratitude (β = -.28) and emotional self-awareness (β = -.30) were also variables significantly related to less time spent in developing a detailed suicide plan. Bono et al. (2022) compiled multiple studies on gratitude in the youth population, emphasizing its capacity to buffer adverse events and resist transitory psychopathological conditions, so this protective function is not surprising. In addition, the psychological treatment par excellence for reducing self-destructive behaviors is dialectical behavioral therapy (e.g., McCauley et al., 2018), which comprises cognitive-behavioral techniques and mindfulness (Linehan, 1993). Exercises aimed at stimulating full awareness have shown, on their own, that they can reduce – not achieving remission – (non)suicidal self-injury (Elices et al., 2016). Behavioral self-control, meanwhile, was the only attribute significantly linked to a lower number of suicide attempts (β = -.43). It represents the antithesis to the impulsivity that classical research has held responsible for multiple suicide attempts (e.g., Abascal-Peiró et al., 2023). Thus, in response to the second research question, it again seems feasible to implement a pilot training program in covitality assets as a selective and indicated prevention method against [adolescent] suicide, with special emphasis on positive beliefs about oneself, about others and about life. Furthermore, fostering emotional self-awareness, gratitude, and behavioral self-control could reduce the exponential mortality rate of the suicide phenomenon among adolescents. Limitations and Future Perspectives Although the present study provides new evidence on the relationship between covitality and suicide, it is not without limitations that invite caution. Its cross-sectional nature prevents establishing cause-effect relationships and ensuring the temporal stability of the findings, so that we can only speak of mere association between constructs (Maxwell et al., 2011; Montero & León, 2007). The geographic delimitation of sampling restricts the generalization of results to other territorial areas or population groups. The exclusive use of the self-report method entails inherent response biases that detract from the objectivity of the data collected on the variables of interest (Kimberlin & Winterstein, 2008). Finally, the non-inclusion of other biopsychosocial factors in the hurdle models overestimates and questions the accuracy of the values provided, considering the complex etiology underlying the suicidal phenomenon (O’Connor & Pirkis, 2016). In this regard, it is worth mentioning that the statistical plan initially contemplated the level of psychopathology and subjective well-being, as they are nuclear factors in the genesis of adolescent suicide (Fonseca-Pedrero et al., 2020), but the previous correlational analysis warned of multicollinearity diagnosis among explanatory variables (r > .70; Tabachnick & Fidell, 2013). As a counterpart, future research could benefit from a repeated measures design, a representative sample of adolescents, a contrast measurement – i.e., multisource, and multimethod – and/or an etiologically multifactorial equation that, taken together, provide more accurate estimates of the scope of covitality as a suicide prevention strategy. Strengths and Practical Implications Despite the limitations described above, this study also has important theoretical and practical connotations. It brings together positions between Positive Psychology and Suicidology, granting prominence to a preventive approach based on individual strengths (Renshaw et al., 2014). It uses a frequency scale for the assessment of suicidal tendencies, beyond its dichotomous categorization in terms of no-yes/absence-presence of markers (Harmer et al., 2021). It employs a statistical methodology especially suited for the processing of suicide related data (Leifker et al., 2021). It provides results controlling for the effect of sociodemographic variables that have traditionally shown a strong influence on suicidality (Miranda-Mendizábal et al., 2019; Voss et al., 2019). It expands knowledge about an emerging model that theoretically integrates the facets that WHO recommends training to combat youth suicide (WHO, 2021a, 2021b). It allows differentiating between the role of psychosocial assets against the absence vs. the presence of suicide indicators, laying the groundwork for imperative multilevel action: universal vs. selective and indicated prevention, respectively (Glenn et al., 2019). And finally, it disaggregates the covitality model, but also the suicide spectrum with the intention of offering personalized interventions in the face of each phenotypic manifestation (Sufrate-Sorzano et al., 2023). Conflict of Interest The authors of this article declare no conflict of interest Author Contributions R. Falcó: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Data curation, Writing - Original draft. S. Falcon: Conceptualization, Methodology, Formal analysis, Writing – Review & Editing. B. Moreno-Amador: Investigation, Resources, Data curation, Writing – Review & Editing. J. A. Piqueras and J. C. Marzo: Writing - Review & Editing, Supervision, Project administration, Funding acquisition. Acknowledgments The authors would like to thank the participants and the schools for their invaluable contribution to this research project. Cite this article as: Falcó, R., Falcon, S., Moreno-Amador, B., Piqueras, J. A., & Marzo, J. C. (2024). Which psychosocial strengths could combat the adolescent suicide spectrum? Dissecting the covitality model. Psychosocial Intervention, 33(3), 133-146. https://doi.org/10.5093/pi2024a9 Funding: This work was supported by the Spanish Ministry of Science, Innovation and Research (AEI/FEDER, UE) under Grant No. PSI2017-88280-R; the Ministry of Economy, Industry, and Competitiveness of the Spanish Government under Grants No. PSI2015-70943-REDT and PSI2017-90650-REDT; and the European Social Fund and the Regional Ministry of Education, Research, Culture and Sport of the Generalitat Valenciana under Grants No. ACIF/2019/052 and ACIF/2019/055. References Appendix Supplementary Materials Table A1 Influence of the Covariates Sex and Age on Psychosocial Strength Levels  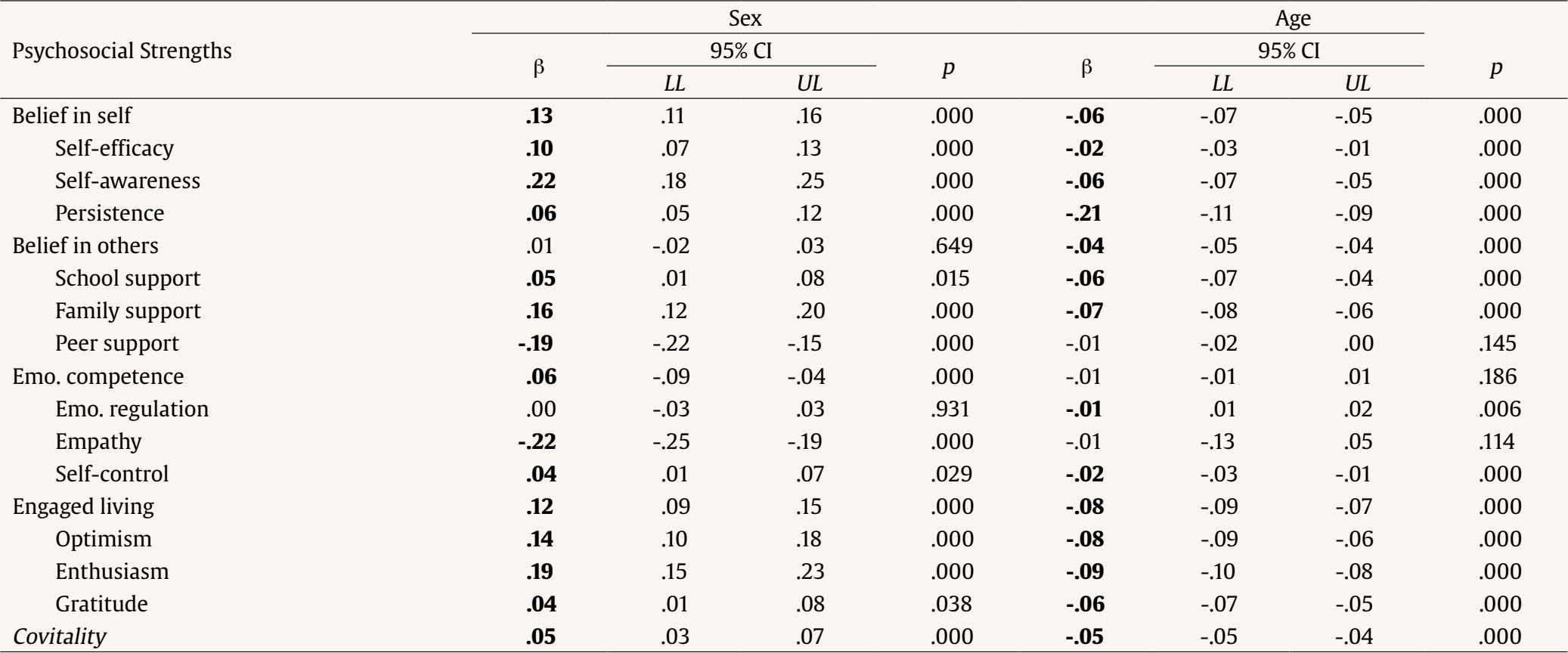 Note. Significance level: p < .05 or 95% CI that does not contain 0 (β in bold type). Sex was coded as 0 = female and 1 = male. β = unstandardized coefficient; CI = confidence interval; LL = lower limit; UL = upper limit; Emo. = emotional. |
Cite this article as: Falcó, R., Falcon, S., Moreno-Amador, B., Piqueras, J. A., & Marzo, J. C. (2024). Which Psychosocial Strengths Could Combat the Adolescent Suicide Spectrum? Dissecting the Covitality Model. Psychosocial Intervention, 33(3), 133 - 146. https://doi.org/10.5093/pi2024a9
Correspondence: jc.marzo@umh.es (J. C. Marzo).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






