
Multicenter Randomized Clinical Trial of Brief Psychotherapy versus Usual Treatment for Common Mental Disorders in Adults
[La eficacia de la psicoterapia breve frente al tratamiento habitual de los trastornos mentales comunes en adultos. Ensayo clĂnico aleatorizado multicĂ©ntrico]
Marco A. Luengo-Castro1, Javier Fernández-Méndez2, José M. García-Montes3, Pedro J. Caunedo-Riesco4, Juan M. García-Haro2, Begoña Braña-Menéndez2, Dolores González-Díaz2, Andrés Cabero-Álvarez2, and Marcelino Cuesta-Izquierdo2
1Public Health Service of Asturias SESPA, Spain; 2Clinical Psychologist in the Mental Health Service of SESPA, Spain; 3Department of Psychology, University of AlmerĂa, Spain; 4Psychiatrist in the Mental Health Service of SESPA (Spain).
https://doi.org/10.5093/clh2025a2
Received 23 April 2024, Accepted 20 September 2024
Abstract
Background: This paper addresses the evaluation of the effectiveness of brief psychological treatment (BPT) for common mental disorders (CMD) in mental health centers (MHC), comparing it to treatment as usual (TAU). Method: 144 patients were randomly assigned to either the experimental treatment group (EG), receiving BPT, or the control group (CG), receiving TAU. Pre-treatment and up to 3-year assessments were conducted on clinical-administrative, symptomatic, disability, satisfaction, and psychopharmacological consumption. Results: The EG had an average of 7 sessions compared to 6.17 sessions for the CG. At 6 months, the CG – with 70% exclusively receiving psychopharmacological treatment – showed better symptomatic improvement than the EG, but worsened after one year. The EG initially exhibited a more modest improvement pattern, but continued and became more effective than TAU after one year. Conclusions: In the medium term, BPT proves to be more effective with longer-lasting effects.
Resumen
Antecedentes: El artículo aborda la evaluación de la efectividad de un tratamiento psicológico breve (TPB) para trastornos mentales comunes (TMC) en centros de salud mental (CSM), comparándolo con el tratamiento habitual (TH). Método: Se asigna 144 pacientes aleatoriamente al grupo de tratamiento experimental (GE), recibiendo TPB, o al grupo control (GC), recibiendo TH. Se realizan evaluaciones pretratamiento y hasta 3 años en variables de estado clínico-administrativo, sintomatológico, discapacidad, satisfacción y consumo de psicofármacos. Resultados: El GE tiene una media de 7 sesiones frente a 6.17 sesiones del GC. A los 6 meses el GC –que el 70% de los casos recibió exclusivamente tratamiento psicofarmacológico– obtiene mejores resultados que el GE en mejoría sintomatológica, pero a partir del año empeoran. El GE tiene un patrón de mejoría más modesto inicialmente, pero continuo, y a partir del año se muestra más eficaz que el TH. Conclusiones: A medio plazo el TPB resulta ser más eficaz y con efectos más duraderos.
Palabras clave
Tratamiento psicolĂłgico breve, Tratamiento psicofarmacolĂłgico, Tratamiento habitual, Trastornos mentales comunes, Ensayo clĂnico aleatorizado, Servicios pĂşblicos de salud mentalKeywords
Brief psychological therapy, Psychopharmacological treatment, Treatment-as-usual, Common mental disorders, Randomized clinical trial, Public mental health centersCite this article as: Luengo-Castro, M. A., Fernández-Méndez, J., García-Montes, J. M., Caunedo-Riesco, P. J., García-Haro, J. M., Braña-Menéndez, B., González-Díaz, D., Cabero-Álvarez, A., & Cuesta-Izquierdo, M. (2025). Multicenter Randomized Clinical Trial of Brief Psychotherapy versus Usual Treatment for Common Mental Disorders in Adults. Clinical and Health, 36(1), 9 - 18. https://doi.org/10.5093/clh2025a2
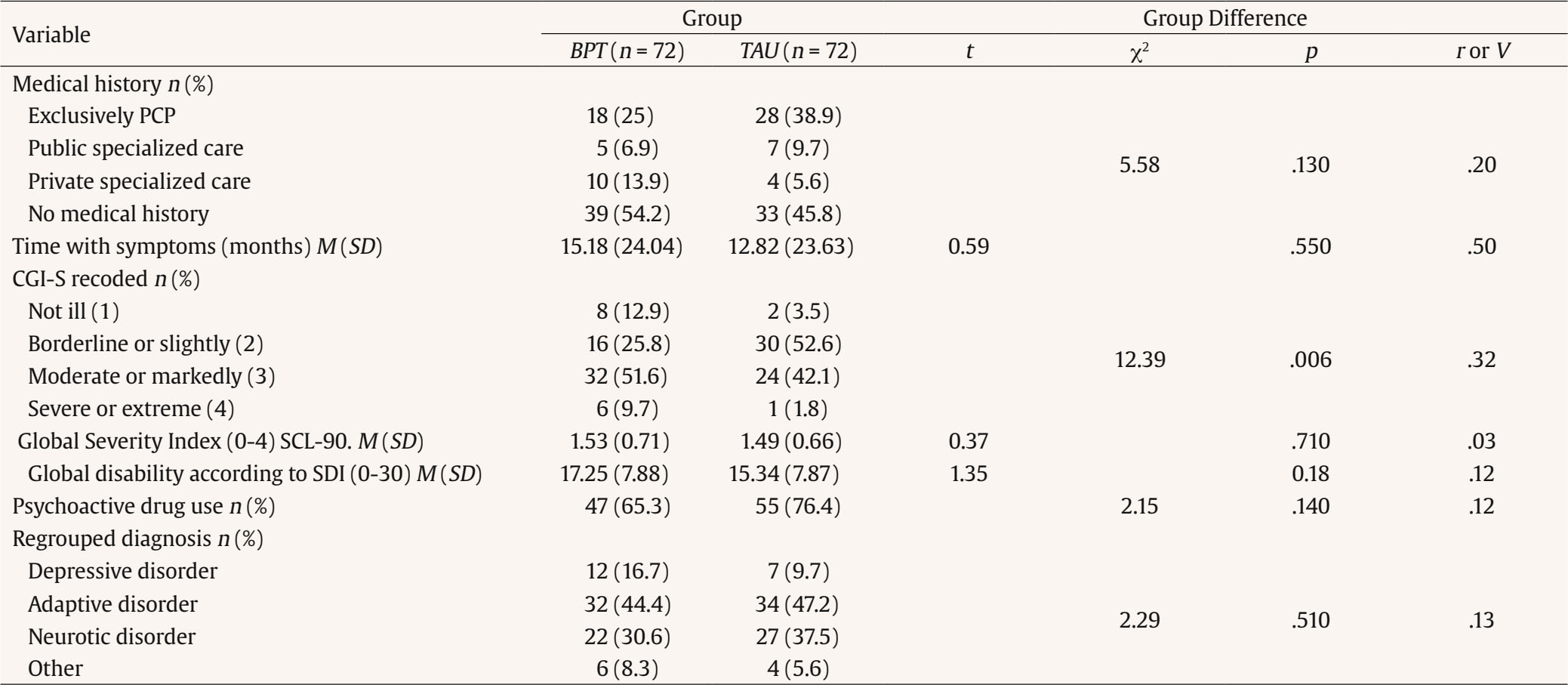
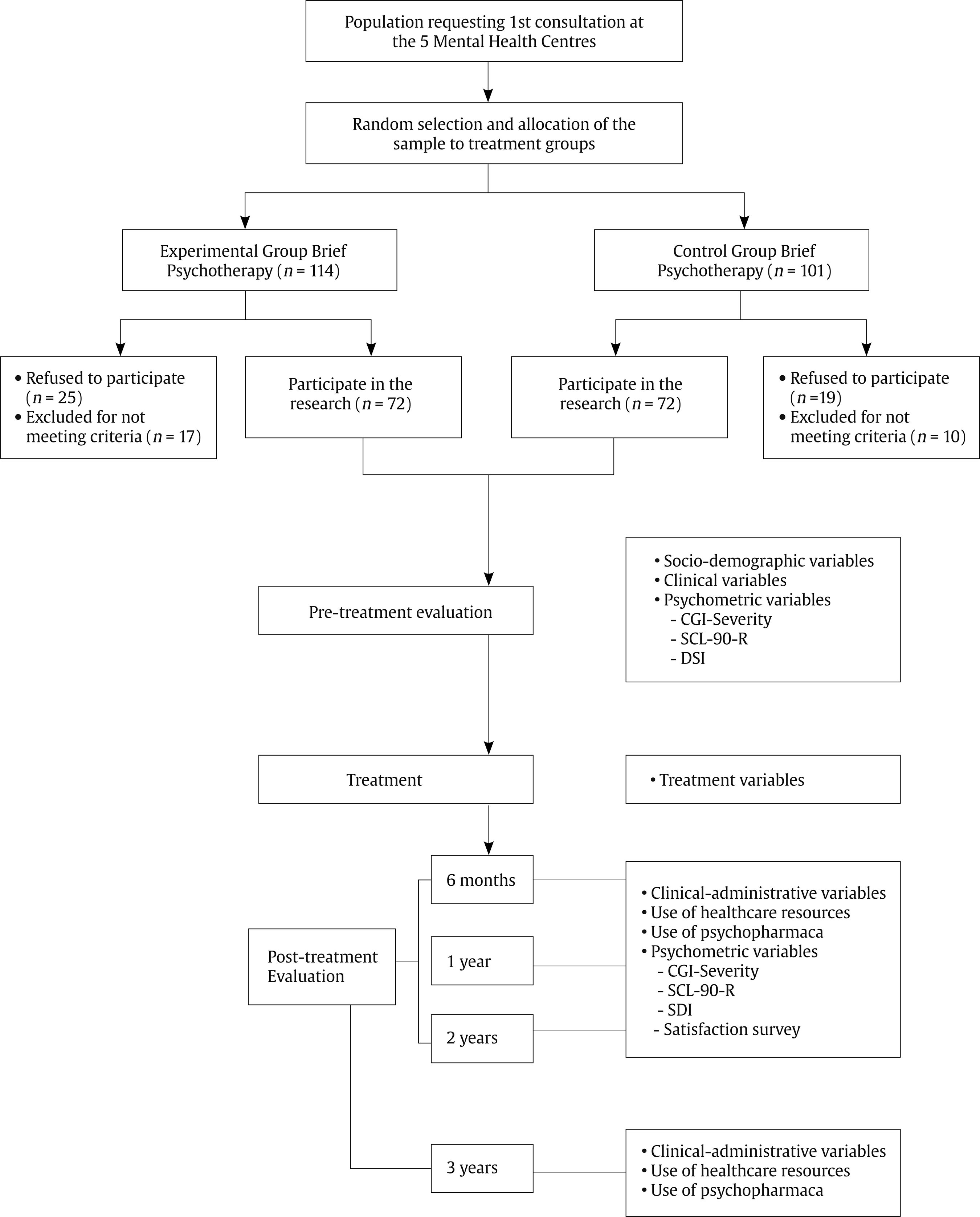
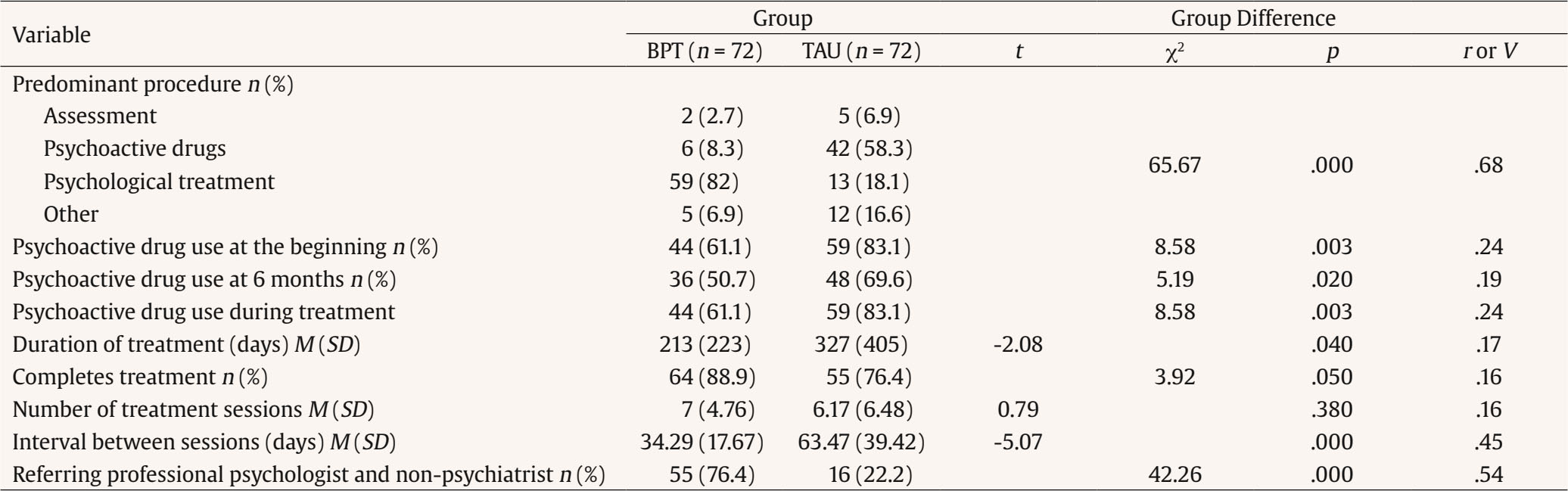
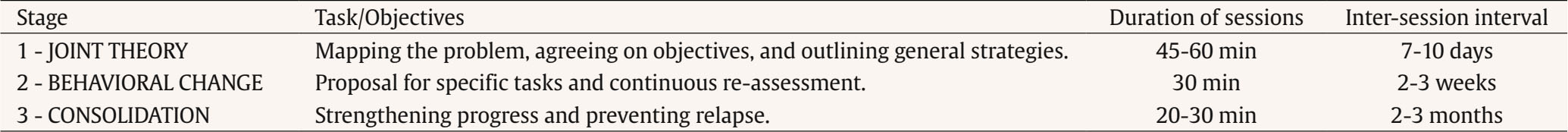
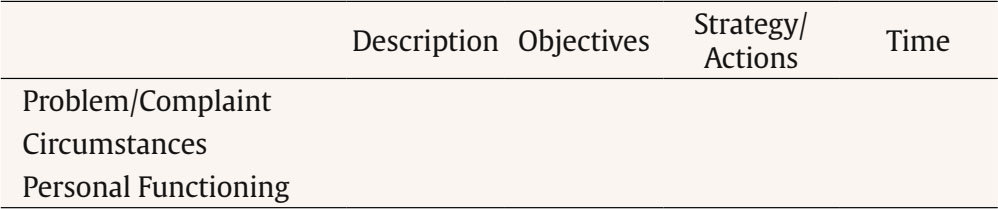
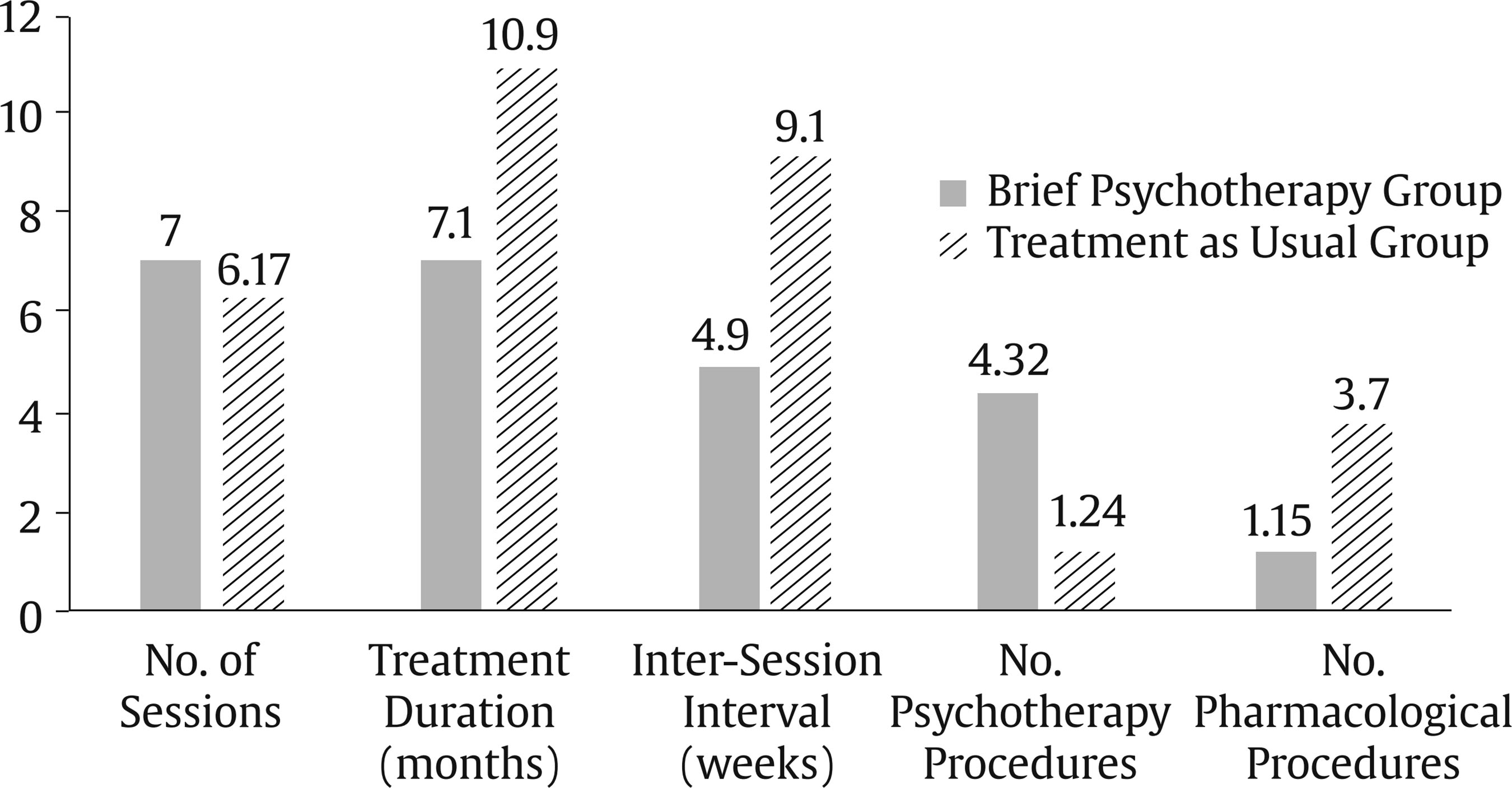
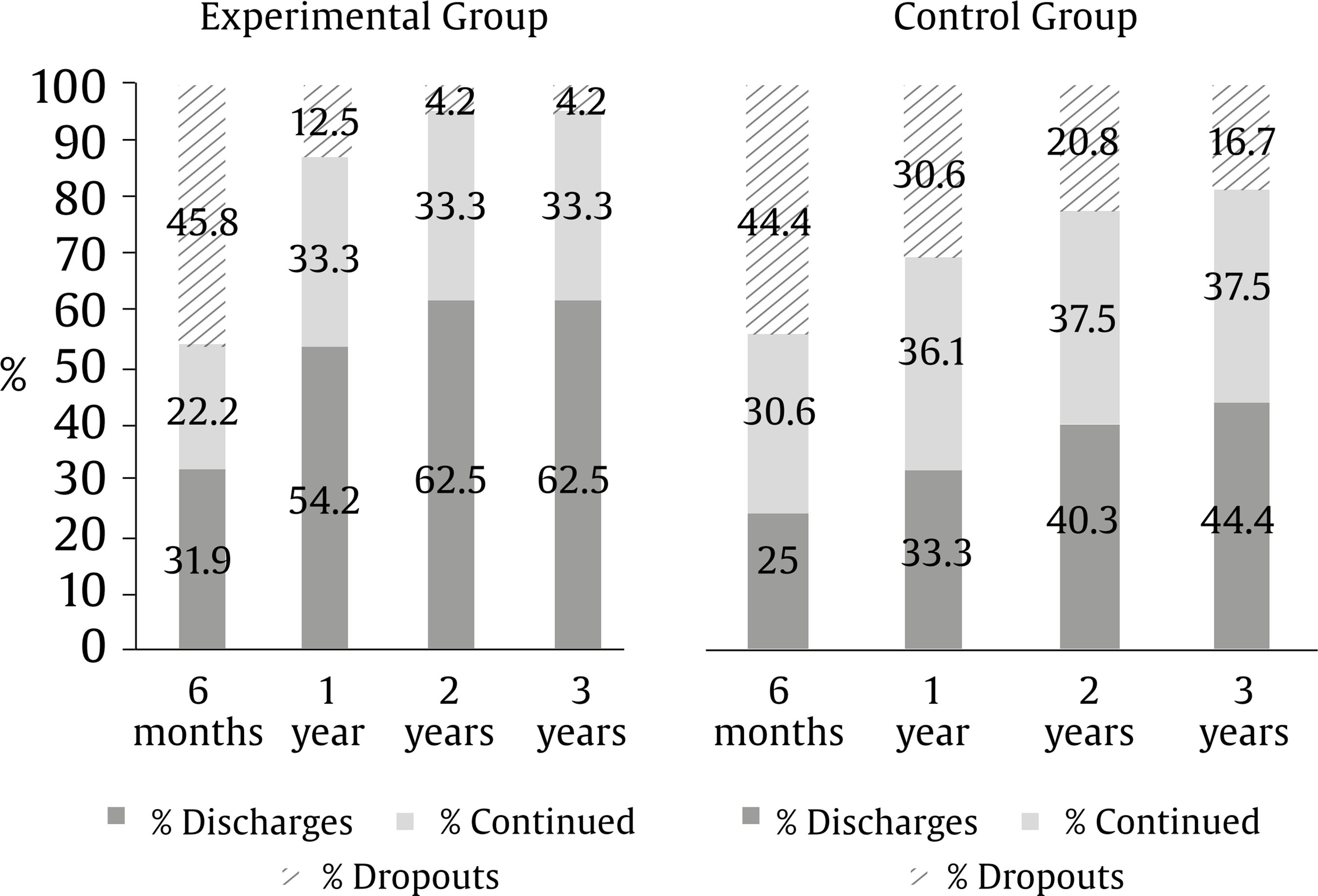
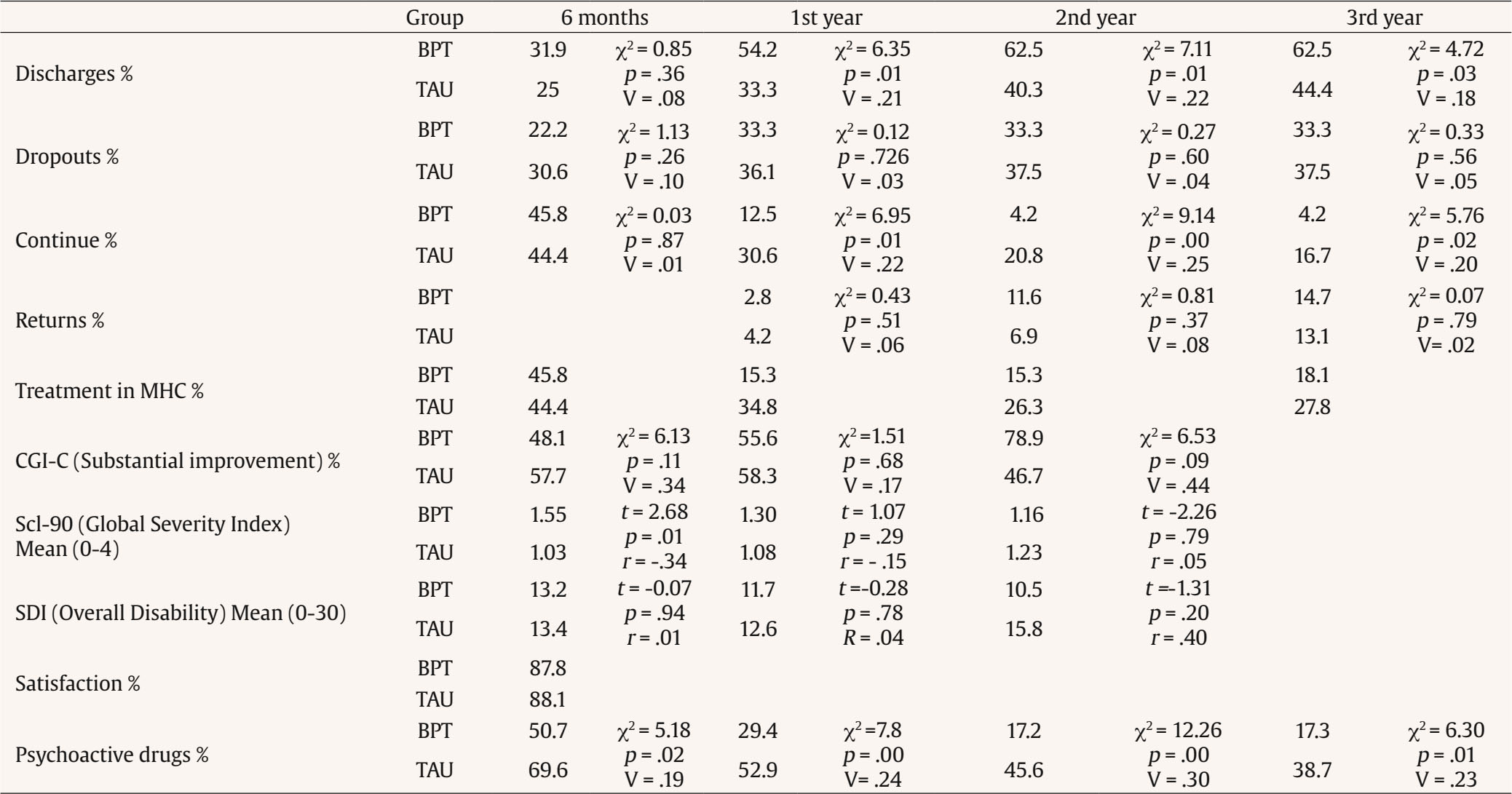
Correspondence: (marcoluengocastro@yahoo.es) (M. A. Luengo Castro).Mood disorders (dysthymia and unipolar major depressive episode) and anxiety disorders (generalized anxiety disorder, panic disorder, phobic disorders, and post-traumatic stress disorder), that do not usually require the intervention of more than one professional, are called common mental disorders (CMD) (National Institute for Health and Clinical Excellence [NICE, 2011]) and from a transdiagnostic perspective as “emotional disorders” (Barlow, 2002). It’s estimated that 1 in 3 women and 1 in 5 men will experience major depression in their lives (Dattani, 2022). Governments can hardly be comfortable with the human, social, and economic costs this entails. Taking an average European country like Spain as an example, the treatment provided for CMD is almost exclusively by prescription of psychotropic drugs, both in primary care and in mental health services, with twice as many women as men taking psychoactive drugs. Indeed, in 2021, 9.3% of people consumed anxiolytics and 9.7% antidepressants. It means 11.15% and 45% more than 2010 respectively (Spanish Medicines Agency, 2023). The COVID-19 crisis will only make these numbers increase 11 % (García et al., 2023). Table 1 Socio-Demographic Characteristics of the Sample  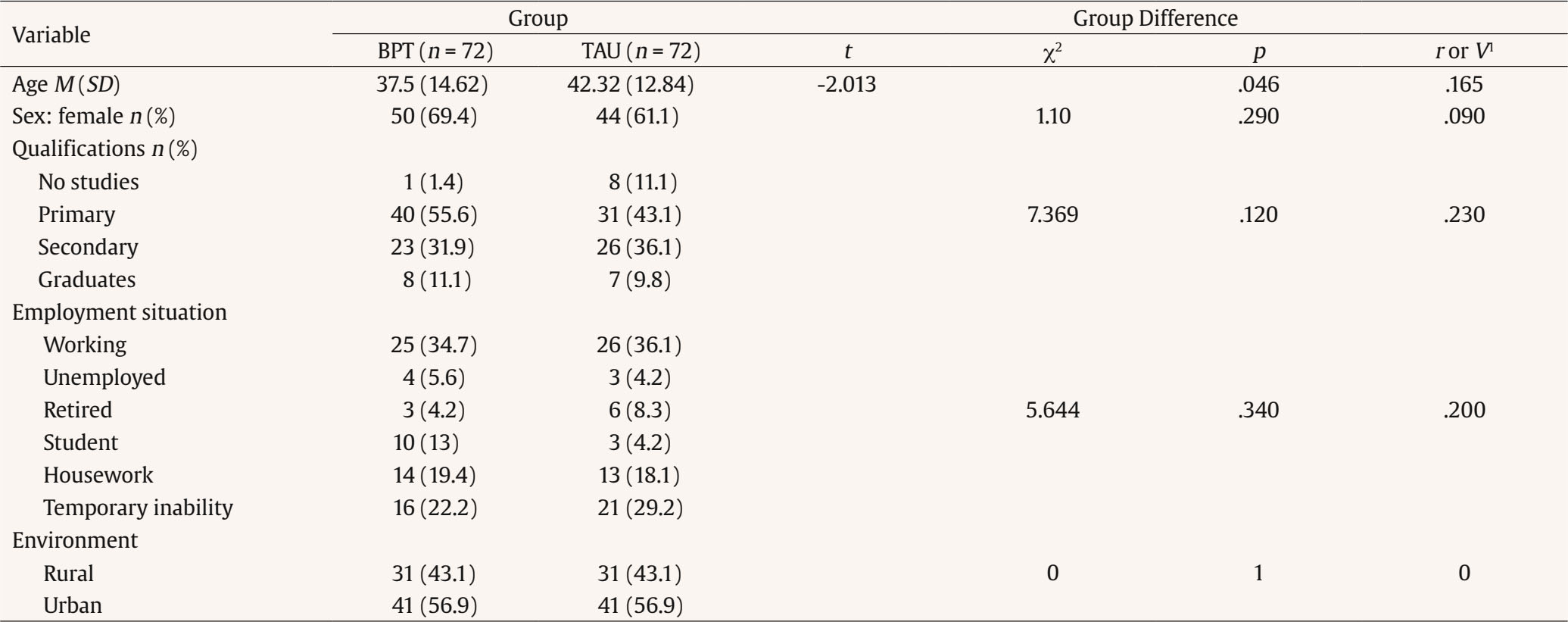 Note. 1Pearson’s r with t-contrast statistic. Cramer V with χ2 contrast statistic. The Health Promotion and Prevention Strategy of the National Health System (General Directorate of Public Health and Innovation, 2018) points out that the pharmacological treatment of emotional disorders results in a high rate of abandonment and relapse, which tends to become chronic, generates an enormous overfrequency of primary care physician (PCP) consultations, causes disability, as well as high economic, social and psychological costs. On the other hand, international organizations such as the UK National Institute for Health and Care Excellence (NICE, 2020, 2021) have collected such scientific evidence and developed clinical guidelines where they primarily recommend psychological treatments for various mental disorders. However, a key question to be answered is whether psychological treatments can be a feasible, effective, and efficient alternative for common mental disorders (CMD) in public health services characterized by high demand, high variability, limited resources, and free care. Improving access to psychological therapy (IAPT) can be considered an example of effective research in a community context (Barkham et al., 2021; Clark, 2018). In Spain, the first multicenter randomized clinical trial (RCT) on the efficacy of psychological treatments for CMD compared to the usual treatments provided in the public mental health services had an experimental design and provided post-treatment assessment (Fernández et al., 2010a, 2010b). The results were extremely revealing, with significant differences in favor of the experimental group (EG) at all times in terms of clinical variables, use of psychoactive drugs, use of services, and degree of disability. In the current RCT, a pre-treatment assessment is also carried out to guarantee the equivalence of both groups and to analyze intra-group evolution better. This RCT is a pragmatic trial defined as a randomized controlled trial whose purpose is to inform decisions about practice (Zwarenstein et al., 2008). The main goal of this RCT is to evaluate the feasibility and effectiveness of a brief psychological treatment (BPT) program compared with the treatment as usual (TAU) used to address CMD in public mental health centers (MHCs). The assumptions of the RCT are that: - BPT is at least as effective as TAU measured in terms of discharge, clinical status, disability level, satisfaction, use of psychotropic drugs, and resource use when treating CMD. - It is feasible to implement a BPT program as the treatment of choice for a large proportion of patients with CMD, even with the same professionals assigned to the centers. - BPT is more efficient than the TAU applied in MHCs to treat CMD, especially in the medium and long term. Participants The sample was randomly selected from among people referred by primary care physician (PCP) to five MHCs (4 urban and 1 rural) of the Principality of Asturias Health Services over a period of 18 months. The sample size was determined based on the human resources and time available for four months and not on the a priori calculation based on the desired effect size. Thus, it was determined to assign each therapist in the experimental group one subject per week for 4 months and at the same time one was assigned to the CG. In each MHC once a week nursing staff unrelated to the research group randomly selected two subjects from among the PCP referrals that had to be assigned that day. The referrals were placed in a random order, then the nurse threw the dice twice, the first time the number determined the referral assigned to the BPT and the second time the one assigned to the TAU. Subsequently, consent was requested to participate in the research without specifying to which group they had been assigned, so subjects were blind. Pre-treatment assessments were made by a person hired by mental health services that was also unrelated to the research group. The inclusion criteria followed were to be over 18 years of age, attend the MHC for the first time, have a CMD, require specialized care (those cases not requiring treatment were excluded), attend at least one consultation at the MHC and agree to participate in the research. The exclusion criteria were not be diagnosed based on ICD-10 criteria for organic mental disorders, psychosis, addictions, eating disorders, mental retardation, psychological developmental disorders, or severe personality disorders (paranoid, schizoid, dissocial, and emotional unstable), and not to have made a serious self-harm attempt in the previous six months. Of the subjects referred to the 5 MHCs, 215 were randomly selected and 87% met the inclusion criteria. The remaining 27 were ruled out, 18 because they had been diagnosed, and 9 because they did not require treatment. Of the 188 that met the inclusion criteria, 44 subjects did not participate: 14 because they failed to attend the first consultation, 17 refused to participate, and 13 for other reasons. In the end, 144 subjects participated. Comparing the subjects who finally participated in the research in both groups, the only socio-demographic variable with a statistical variation was age (Table 1). Regarding the pre-treatment clinical situation, in the CGI-S scale, the EG presented the most extreme scores while in the rest of the clinical variables, there were no significant differences (Table 2). Since this RCT is eminently pragmatic and evaluates the benefit of the treatments in daily practice, an “intention-to-treat” analysis was chosen. At mental health centers of Asturias treatments do not have a predetermined duration and neither does the BPT program. Therefore, we assumed that subjects who attended at least 3 consultations with a psychiatric or clinical psychologist at the MHC or fewer if the therapist discharged them were considered to have completed the treatment. Instruments The pre-treatment variables recorded were socio-demographic (10) and clinical (25). They were drawn from the medical records and the questionnaires given to the patients. There are more than 20 outcome or dependent variables and they were recorded at each follow-up. They analyze the clinical-administrative outcome, clinical and disability status, treatment in primary care, employment situation, consumption of psychoactive drugs, satisfaction, etc. The data was extracted from the clinical history at the MC, the primary care clinical history, the questionnaires, and the central case register of the health service of the Principality of Asturias. The following is a description of the fundamentals and the measuring instruments used: Clinical-administrative Outcome Consists of the following categories: ongoing treatment, discharge (patient has been discharged by their referring therapist), dropout (patient discontinues treatment against the therapist’s advice or without consultation with the therapist), return and other. Clinical Status according to the Patient Patients were assessed using three scales. The Severity Scale of the Clinical Global Impression of Severity (CGI-S; García-Portilla et al., 2022; Guy, 1976). Applied to the patient before starting treatment, it consists of a single item where the patient evaluates the degree of severity based on 7 alternatives: not ill, borderline ill, mildly ill, moderately ill, markedly ill, severely ill, and extremely ill. The Change or Improvement Scale of the Clinical Global Impression of Change (CGI-C; García-Portilla et al., 2022; Guy, 1976). Applied to the patient during telephone interviews, it consists of a single item in which the patient is asked how their condition has changed compared to the start of treatment, offering 7 response alternatives, scored from 1 to 7 (much better, better, somewhat better, no change, somewhat worse, worse, much worse). For the purpose of analysis and presentation of results, we grouped the values as follows: much better or better (1 or 2), somewhat better (3), no change (4), and worse (5, 6, or 7). Symptom Check List-90 (SCL-90-R; Derogatis, 1977; González de Rivera et al., 1989). Three global indices are obtained, global severity index (GSI), positive symptom total (PST), and positive symptom distress index (PSDI). The GSI combines the number of symptoms present with their severity. It is the best indicator to summarize both the intensity and the degree of symptomatology. This index theoretically ranges from 0 to 4. Degree of Disability according to the Patient Assessed using the Sheehan Disability Inventory (SDI) (García-Portilla et al., 2022; Sheehan et al., 1996), which assesses disability based on three items scored from 0 to 10: work, social life, and family life. The sum of the scores provides an overall disability index. family life. The sum of the scores provides an overall disability index. User Satisfaction with the Treatment Evaluated by items selected from the Moré and Muñoz (2000) Satisfaction Questionnaire on the level of perceived benefit regarding the treatment and the degree of Satisfaction with the care received. It was collected at the first follow-up assessment (one month after discharge or dropout, or 6 months if still being treated). Use of Psychoactive Drugs It was used the equivalence in milligrams of Imipramine for antidepressants and in milligrams of Lorazepam for benzodiazepines. The outcome variables can involve different types of criteria or sources of assessment: therapist (clinical outcome), self-referred patient (clinical status, degree of disability, satisfaction), and consumption of psychotropic drugs. It is extremely important to have considered all sources of assessment because, as the psychometric outcome variables depended on patients completing the questionnaires and sending them by post, only 55.6% answered at some point during follow-up, 56.9% in the EG, and 54.2% in the CG. If we only took the psychometric data of the respondents into account, we would most likely be overestimating the effectiveness of the treatments (Clark, 2018). Procedure It has been designed a full-powered multi-center randomized clinical trial with an experimental group (EG) and a control group (CG), with pre- and post-treatment evaluation performed in 5 public MSCs and follow-up at 6, 12, 24, and 36 months. Prior to the start of the clinical trial, this research was authorized by the Research Ethics Committee of Asturias (Spain). A psychologist hired specifically by the Health Service of the Principality of Asturias, and external to the research group, conducted the evaluation interviews and collected and recorded the outcome variables at the beginning of the treatment, at 6 months, one year, two years, and three years. The research was also registered in an official Register of RCT. Figure 1 shows the research design, the various phases of the procedure, and the variables that were recorded at each stage. In Luengo’s (2015) doctoral dissertation the results of the comparative analyze of the subjects who refused to participate in the research, those who did not complete treatment, those who did not participate in the psychometric evaluation follow-ups and pretreatment variables in both groups are available (pp. 43-48, 67-73, and 111-114). Participants received two types of treatment: TAU and BPT. Interventions were developed in person, which possibly facilitated a faster change in the people attended, compared to other modalities, such as, for example, through video conferences (Fernández-Regueras & Calero-Elvira, 2024). A more accurate description of these procedures was made a posteriori, once the variables describing the type of intervention had been recorded de facto (Table 3). Brief Psychological Therapy Program The initial premise behind the selection of experimental therapy was to develop a general guide to define and give structure to the BPT based on a flexible model that would adjust to the variety of demands, patients, and the heterogeneity of therapists in public services. The initial reference point was a Zealand Brief Therapy Program (Rijnders, 2004). The main emphasis was on psychological treatment, although the use of pharmacotherapy was not ruled out. From a theoretical point of view, it draws on a competence-vulnerability balance model based on Jerome Frank’s demoralization hypothesis (Frank & Frank, 1991), who is one of the predecessors of the current transdiagnostic approaches that suggest the factors that are common to different emotional disorders (Hofmann & Barlow, 2014). Actually, psychotherapy makes up a unique relationship of a non-punitive nature, which is not conditioned by the past or the future (Al-Halabí, 2023). In our case, we chose to develop a strong contextual and active perspective in our therapy, applying the principles of brief systemic psychotherapy (de Shazer, 1988; Watzlawick & Nardone, 2014) as well as the common factors model (Kleinke, 1994). Psychotherapeutic treatment is structured in three phases (Table 4) and the intersession interval is also considered a key factor in the treatment. A generic problem-objective-task definition scheme is applied (Table 5). There is no maximum number of sessions, nor does the guide prescribe specific procedural techniques, these depending on the characteristics of the case and the therapist’s criteria. In practice, this would be comparable to an approach that considers different levels of treatment intensity on a case-by-case basis (stepped care model), such as the IAPT model. This premise is adapted to the service portfolio of the Spanish health system, and following the brief therapy model (Watzlawick & Nardone, 2014) we considered that the subjects who attended at least 3 consultations at the CSM with the therapist completed the treatment or at least if the therapist discharged them. In our program, however, it is possible to use techniques from different theoretical models (Fernández et al., 2010a) based on a contextual approach (González-Pardo & Pérez-Álvarez, 2007; Pérez-Álvarez, 2013). In this particular research and given that most therapists had systemic training and orientation, psychotherapy has mainly followed brief systemic therapy techniques (Rodríguez-Arias & Venero, 2006; Watzlawick & Nardone, 2014), complemented with cognitive-behavioral techniques as cognitive restructuring techniques (Wenzel, 2021). At the end of the three years, the mean duration of the brief psychotherapy program was 213 days (Mdn = 170), with an average of 7 sessions (Mdn = 5.5). Intersession interval was 34.29 days (Mdn = 31.37). Psychological treatment was the predominant procedure in 82% of cases. Treatment as Usual Subjects assigned to the CG were treated as usual at the MHC in the Principality of Asturias; 67.2% of the cases received only psychopharmacological treatment and 11.9% only psychological treatment. The average duration of treatment was 327 days (Mdn = 116), with 6.17 sessions on average (Mdn = 3.5). Inter-session interval was 63.47 days (Mdn = 59). Figure 2 shows the empirical description of both treatments. Therapists The profiles of the 6 therapists in the brief therapy group were as follows: 5 clinical psychologists and one psychiatrist, 4 men and 2 women. The average age was 42.15 (SD = 9.3), with 16 years of experience (SD = 8.7) and an average of 745 hours of psychotherapy training (SD = 374). The predominant theoretical approach was systemic-eclectic. Prior to the start of the research, therapists-researchers were trained in the psychotherapy script through seminars, and case-monitoring sessions lasting 45 hours. A distinguishing feature of this trial was that all the therapists belonged to the MHCs and were not external professionals with highly specific training in the treatment model to be implemented. The CG cases were attended by all the therapists at the MHCs where the research was being conducted. In total, there were 7 clinical psychologists and 15 psychiatrists; 16 cases (21.6%) had a clinical psychologist as their referral therapist and 58 (78.4%) had a psychiatrist. Transparency and Openness All data is available in a public Database at https://osf.io/nxuqz/?view_only=ff556c1988f944a08b16b400842aa9c5 Data Analysis Statistical analyses were carried out using SPSS (Statistical Package for Social Sciences) version 15.0. In addition to descriptive analyses, the chi-square (χ2) test was used to compare categorical variables and the Student’s t to compare the quantitative variables Cramer’s V and Pearson’s r were used to measure effect size, respectively. Luengo’s (2015) doctoral dissertation is available in Spanish and provides a detailed account of the research variables and outcomes. In addition, the clinical trial was registered in the ISRCTN Register https://doi.org/10.1186/ISRCTN11895027 The outcome variables and time points are shown in Figure 1. Table 6 shows the main results at different points in time with the corresponding contrast statistics. Clinical-Administrative Outcome The evolution of both groups was different. In the EG, significant results were already achieved in the first year. In total, 18.1% of the cases were under treatment after 3 years. In the CG, the progression of discharges was slower, 27.8% of the cases were under treatment at the 3-year point. Figure 3 shows evolution over the three years. Symptomatological Status On the ICG Change Scale at 6 months, 48% of the EG subjects reported feeling slightly better or much better. At one year the figure was 56% and at two years it was 79%. This is a continuing positive trend Figure 4. Figure 4 ICG-C Symptomatological Evolution in Both Treatment Groups. Percentage of Subjects Displaying Substantial Improvement.  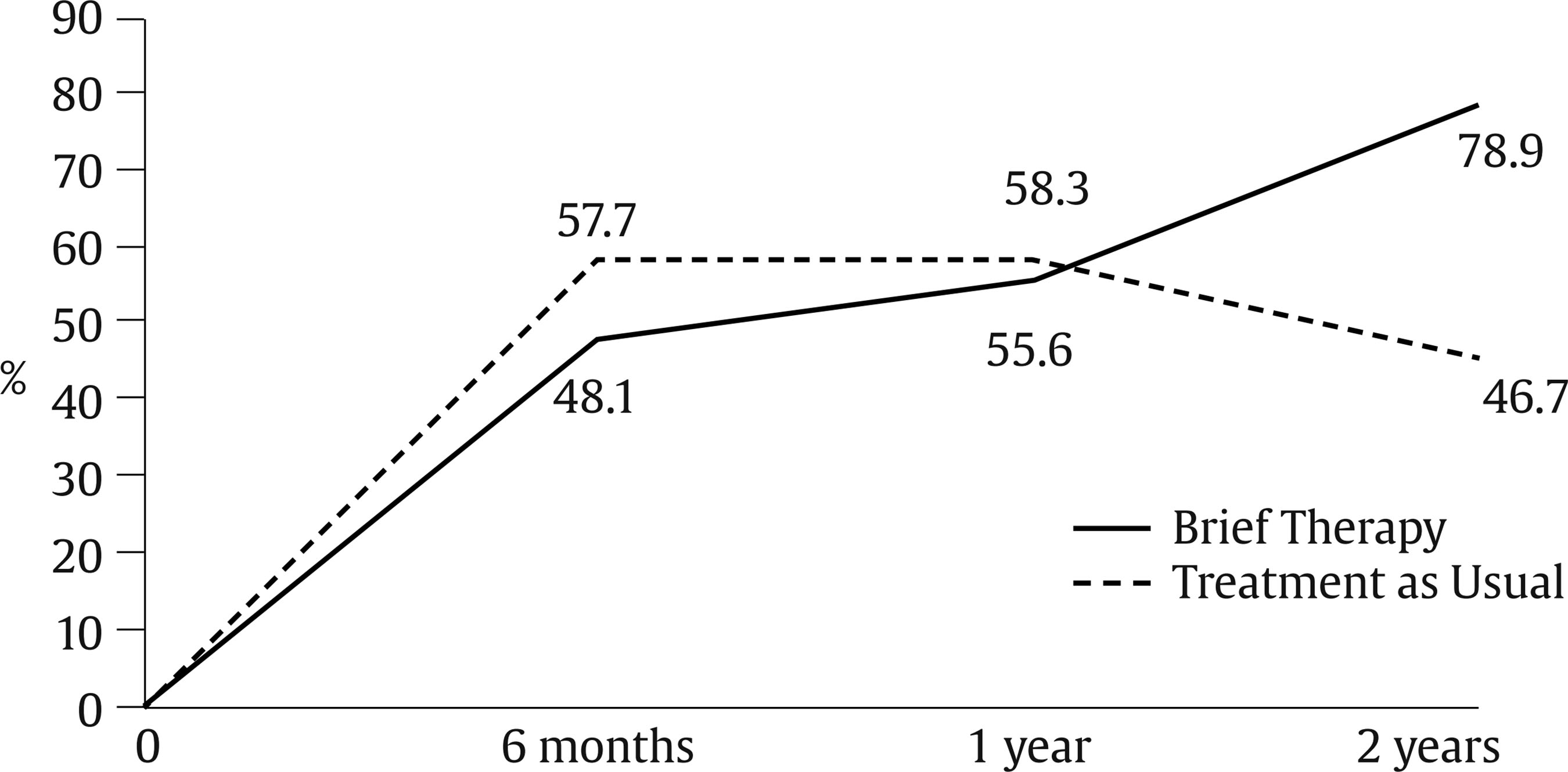 However, at 6 months 19% of subjects reported feeling worse than at the start of treatment (Figure 5). Figure 5 ICG-C Symptomatological Evolution in Both Treatment Groups. Percentage of Subjects the Same or Worse.  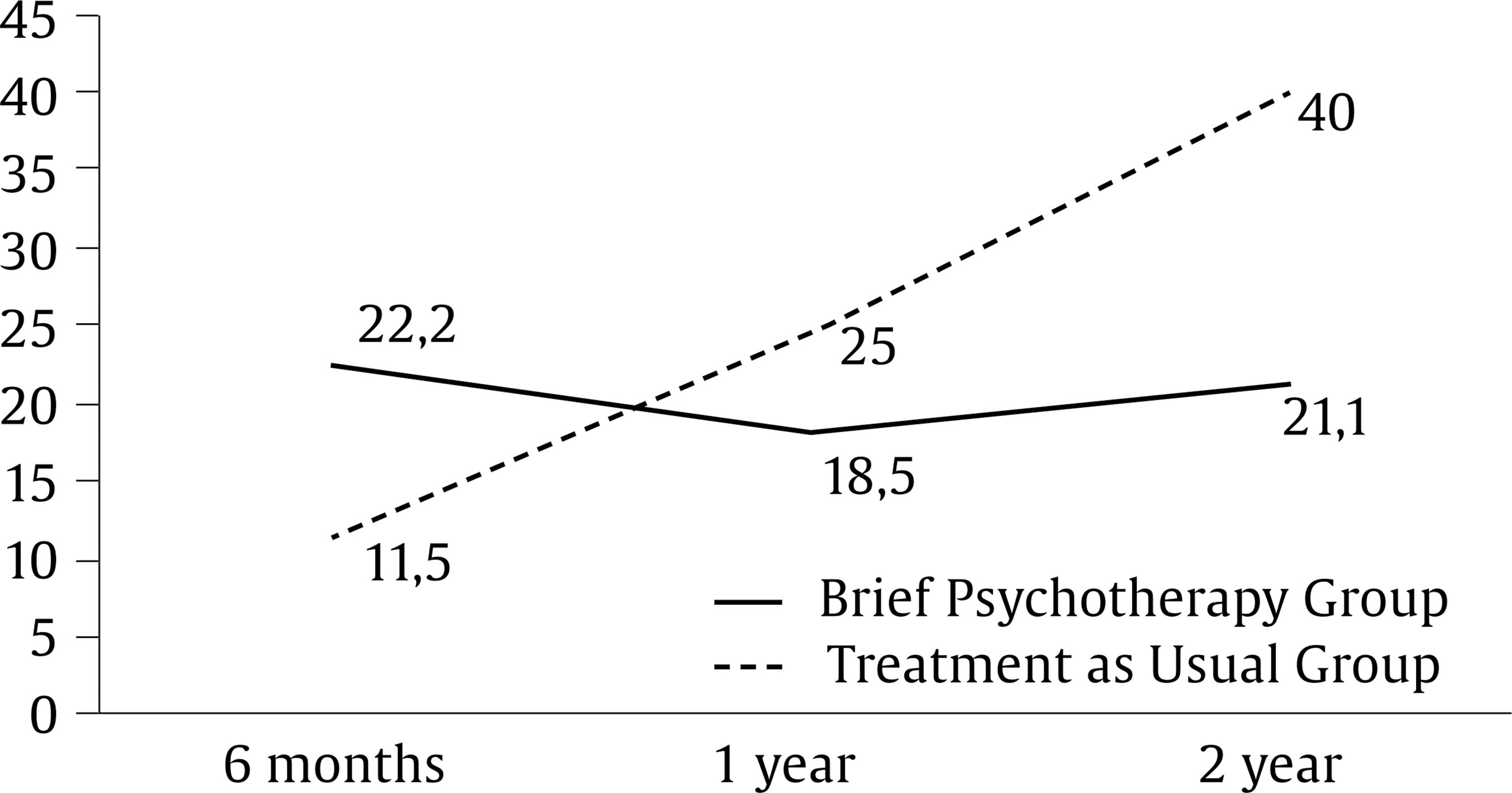 In the CG, at 6 months, the results were better; 58% of the cases said they felt slightly better or much better, but after one year the percentage remained the same and after two years it dropped to 47%. In other words, the best results are achieved during the first few months, but after that the improvement is not sustained (Figure 4). After two years, 27% of subjects reported feeling worse than at the start of treatment (Figure 5). In the SCL-90 Scale, the symptomatology begins after six months to progressively improve in the EG group. Until then, symptoms even worsen slightly compared to the start of treatment (Figure 6). Figure 6 Evolution of the Global Severity Index of the SCL-90-R Questionnaire in Both Treatment Groups.  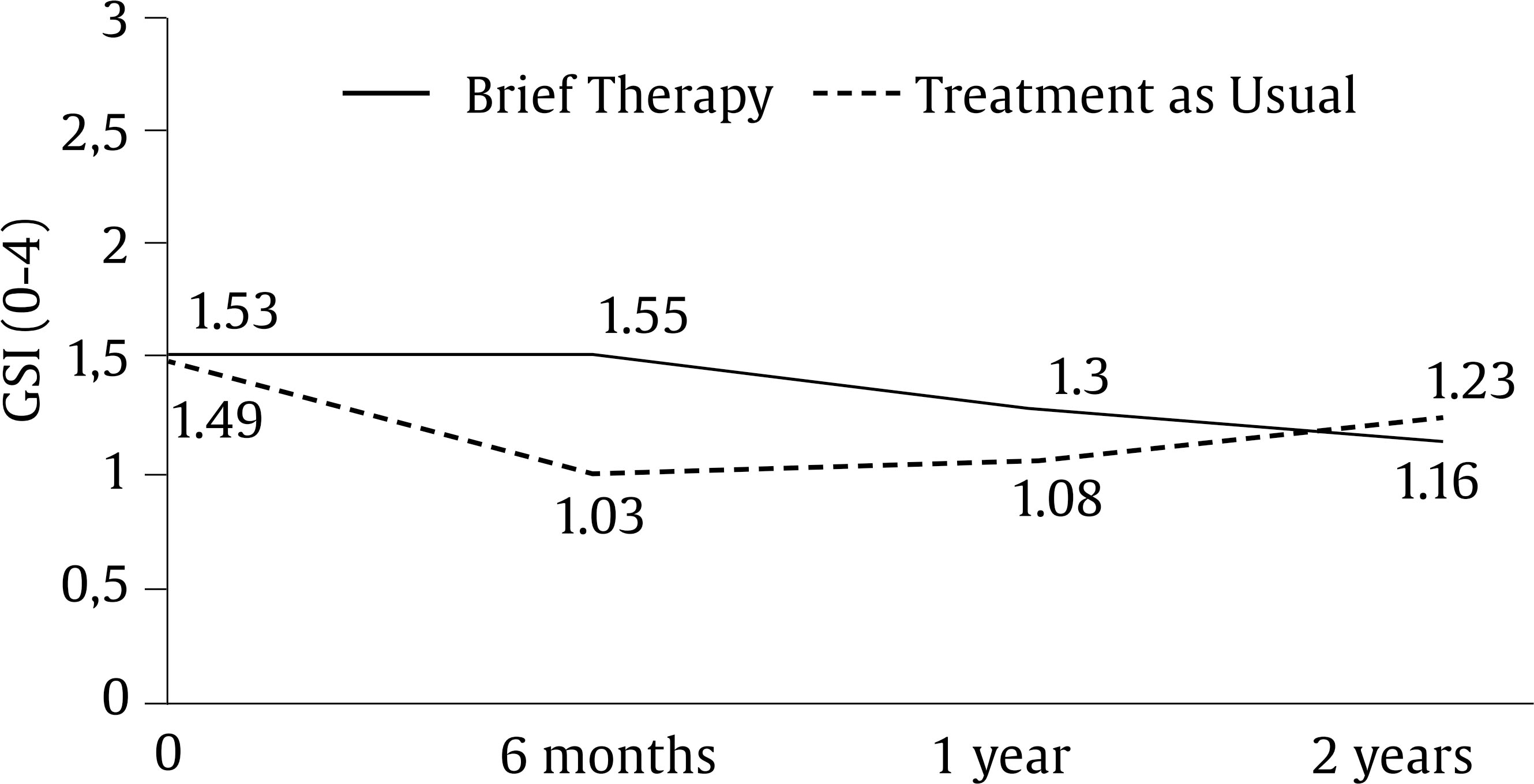 However, the opposite happens in the CG. Symptoms improve considerably in the first six months, but thereafter the trend toward improvement is not sustained (Figure 6). Disability Level The EG shows a continuous decline in SDI Scale disability scores (Figure 7). Figure 7 Evolution of the Global Disability Level of the SDI Questionnaire in Both Treatment Groups.  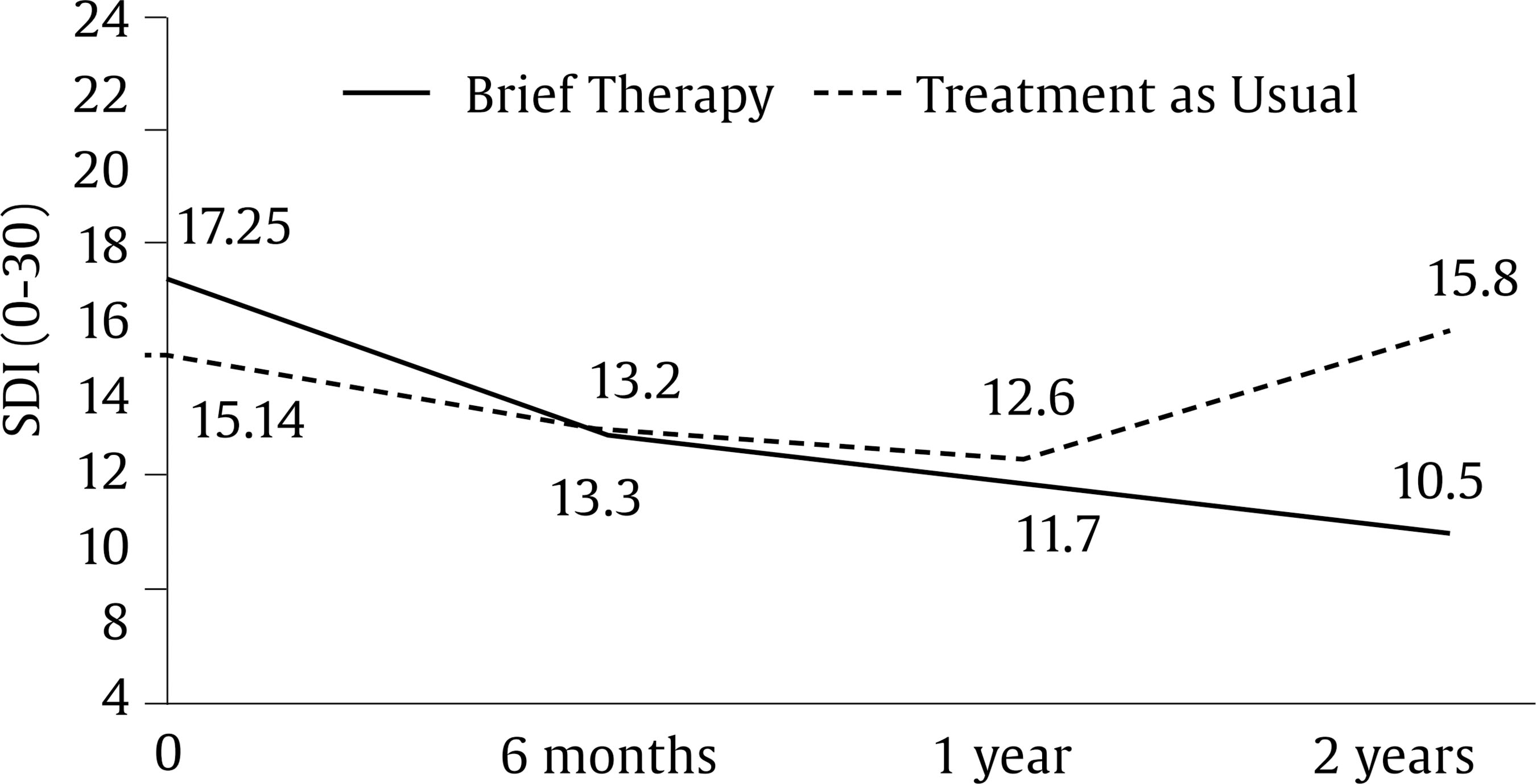 The CG improves at 6 months and also at one year, but at two years it worsens significantly, displaying an even greater level of disability than at the start of the treatment (Figure 7). Consumption of Psychoactive Drugs A 70.8% of the subjects were taking psychoactive drugs before coming to the MHC. After the first few weeks of starting treatment at the MHC, the percentage of subjects in the EG taking psychoactive drugs decreased by 4% while in CG it increased by almost 7%. The differences remained at the following points in time. However, in both groups the number of people taking psychoactive drugs gradually decreased (Figure 8). Figure 8 Evolution of the Percentage of Subjects Using Psychoactive Drugs in Both Treatment Groups at Each Time Point.  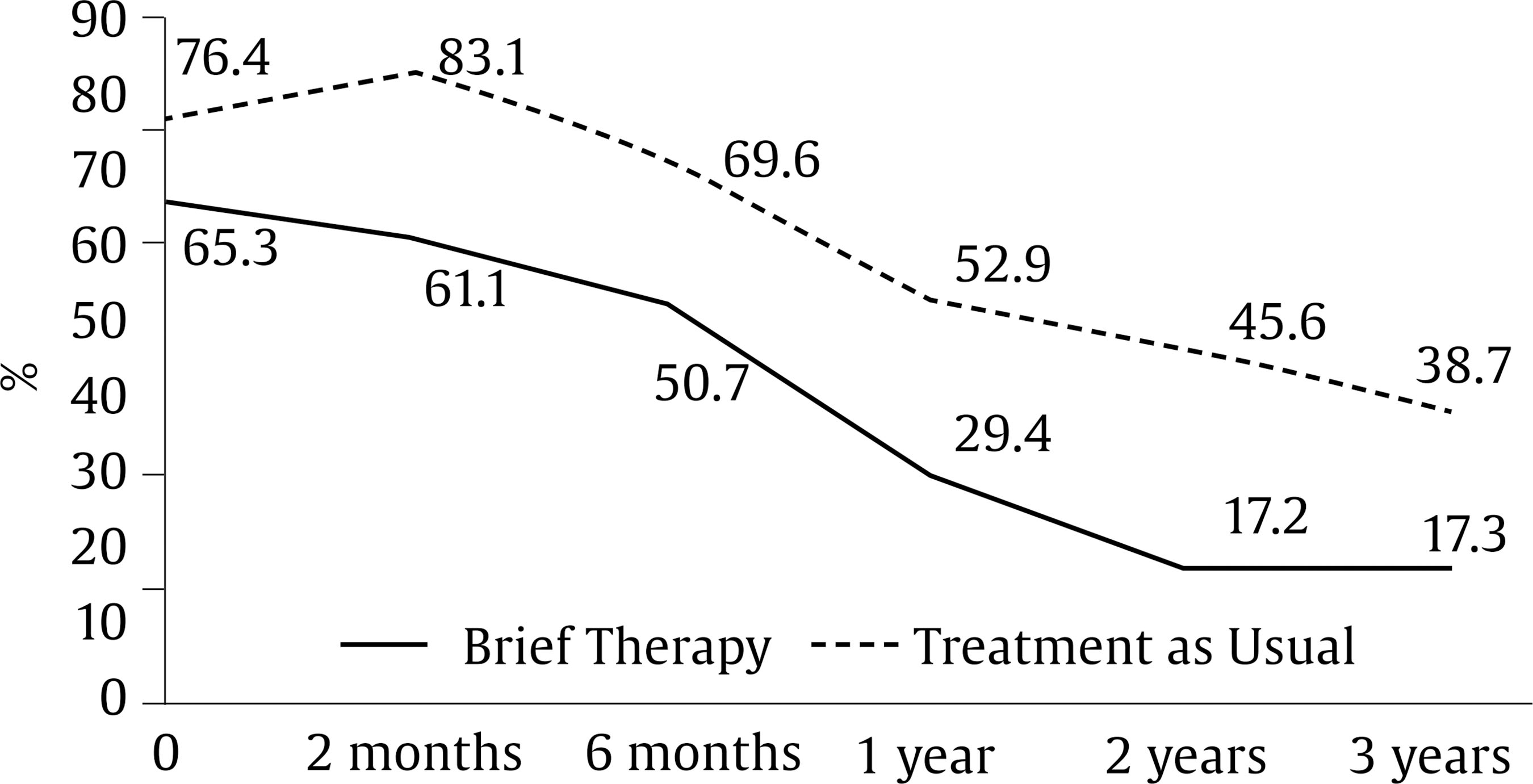 Satisfaction with the Treatment Both groups showed a high level of satisfaction. The percentage of subjects reporting that the treatment was beneficial was 87.8% in the EG and 88.1% in the CG. In addition, 92.9% of the subjects in the EG compared to 85.7% in the CG reported being satisfied with the assistance received. However, we must be cautious with this data as satisfaction information was collected after approximately 6 months, and there was no subsequent measurement. The present study aimed to evaluate the feasibility and effectiveness of a brief psychological therapy (BPT) program compared with the treatment as usual to address CMD at MHCs in the Principality of Asturias. In the medium-term the BPT program proved to be more effective and had longer-lasting effects in terms of discharge, clinical condition, level of disability, and use of psychoactive drugs. The evolution of each group and the difference between them can be related to the bases and premises of the theoretical model of each type of treatment. Thus, psychopharmacological treatments place special emphasis on the biological aspects and symptomatology as the cause and object of treatment and focus the results on those aspects. In contrast, psychological treatment applied is contextual and assumes that the symptomatology improves once subjective circumstances and functioning allow the person to adapt better to their environment; hence symptomatology takes some time to begin to decrease, but then this improvement is sustained and increases after the first year. This view would also help us understand why the improvement achieved with psychopharmacological treatments is not sustained in many cases. The effect of treatment would fade as it does not foster a change in how people deal with their life conditions in a more adaptive manner. This could also partly explain two extremely significant phenomena, the long duration of psychopharmacological treatments, and the high rate of return of patients to the public mental health centers (Spanish Ministry of Health, 2007). Another element that could have been key in the BPT results was that the intersessions interval was adjusted to the conditions required for psychological treatments (Bruijniks et al., 2020; Erekson et al., 2015). Although the main goal of our work was to study the effectiveness of brief psychotherapy, one of the main conclusions refers to the effectiveness of psychopharmacological treatments and how its effectiveness is not sustained over time. Data points to something highly relevant and underresearched, which is that the positive effect of psychoactive drugs progressively diminishes after six months, although this is not usually reflected in studies on the effectiveness of psychopharmacological and psychological treatments, because most of them focus on short-term results and do not carry out subsequent follow-ups (González-Pardo & Pérez-Álvarez, 2007; Smith, 2005). The RCT has also confirmed that it is a viable treatment choice in public services: the procedure has been implemented in a real context without any structural changes and has been delivered by the public service professionals themselves; 87% of the cases that arrived at the MHCs met the criteria for the program and the average number of sessions was 7, only one more than the treatment as usual. This does not preclude that actions for the improvement of mental health should not be limited to the field of psychological treatments but should also extend to the realm of prevention during school age (Fonseca-Pedrero et al., 2023). Focusing on the necessary comparison with other studies (Gambara et al., 2021), the results presented in this RCT are consistent with other studies and clinical recommendations. The Centre for Economic Performance’s Mental Health Policy Group Report (Layard, 2006, p. 6) has already concluded that “The general finding is that therapy is as effective as drugs in the short-run, and that both are better than no treatment. In the longer run therapy has more long-lasting effects than drugs.” The same conclusions are driven by other major RCTs and metaanalyses (Nathan & Gorman, 2015; Roth & Fonagy, 2005) and the most recent IAPT outcomes (Clark, 2018; Wakefield et al., 2020). Added to this is the increasing preference of patients for psychological rather than pharmacological treatments (McHugh et al., 2013). We compare the results presented mainly with those of the IAPT project as, although it is not an RCT, it is a study in the public context and the size and standardization of the results make it highly valid. In the IAPT, the clinical significance of improvement in patients is higher in terms of symptomatology reduction than at the functional level and quality of life level (Knapstad et al., 2020; Wakefield et al., 2020), although they do not report results of over a year. In our RCT, during this time frame, the BPT achieved rather modest improvements at the symptomatological and functional levels. Even symptomatological improvements are almost non-existent in the first 3-6 months, and certainly less than in the TAU and in the outcomes reported in the IAPT (Clark, 2018). It is at two years that a significant clinical and functional improvement is identified, although, due to the high sample loss of psychometric data in this time period, we must be very cautious and analyze the consistency with other more objective outcomes, such as psychotropic drugs consumption. Another highly relevant aspect of the results of our RCT is that the beneficial effects of TAU do not last beyond one year and there is a worsening trend thereafter. This is difficult to contrast with other studies as the follow-up does not usually exceed one year, but it is consistent with the high prevalence, relapse, and return rates of CMD. Furthermore, mental health issues carry a high degree of stigma, even among the professionals who treat them (Zamorano et al., 2023). Recent research shows that the positive effect of antidepressants is due to a temporary increase in neuronal plasticity (Casarotto et al., 2021; Umemori et al., 2018), but it is possible that if no new learning occurs as in psychotherapy, this plasticity will not be exploited in the medium term. It is worth introducing a final reflection regarding the uncertainty already noted in several metaanalyses concerning the superiority and specificity of some psychological treatments over others, based on classical diagnostic criteria. This explains that the same treatment works for different diagnoses and that different treatments work for the same diagnosis. In this sense, and unlike somatic illnesses, contextual, transdiagnostic, and common principles-based approaches to psychotherapy seem much more successful and realistic in addressing mental disorders (Elkins, 2012; Pérez-Álvarez, 2013) and our BPT program is an example of this. Limitations and Strengths of the Study The maximization of external and ecological validity has been a priority element in the design of this RCT, given that there are already studies of high methodological quality that demonstrate the efficacy of brief psychotherapies under ideal conditions, but it is as difficult as it is necessary to generalize these treatments and results to real public mental health services contexts (Moriana et al., 2022). It has also been very important to compare this program with TAU in the MHC knowing that this is very heterogeneous. Consequently, the internal validity of the study is affected, mainly for the poor definition of the treatments, particularly of the TAU, because in the end there would have been at least three different types of treatment: pharmacological, combined, and only psychological treatment. (See Table 3 and Figure 2). External validity was also affected by the high sample loss during the psychometric assessment follow-ups. However, the outcome variables are based on different sources of assessment: therapist (clinical outcome), patient (clinical condition, degree of disability, satisfaction), and consumption of psychotropic drugs. Analysis of the data reveals consistency in the outcomes obtained from the different sources of information (Fernández-Rodríguez et al., 2023), in spite of the the methodological weaknesses of the study. Another factor that we consider extremely relevant in favor of the consistency of the study results is the coherence and similarity with the outcomes of the previous clinical trials carried out (Fernández et al., 2010b). Implications Psychological treatments should be considered as the first treatment option for common disorders in public health services since, although in the first few months the results are similar to those of psychopharmacological treatments, in the medium term they are more effective and have longer-lasting effects. The fact that in MHC the most appropriate intervals between sessions are not being respected is most likely reducing the effectiveness of the psychological treatments and therefore should be reviewed in MHC programs. In contrast, primarily psychopharmacological treatments achieve good results at 3-6 months, but thereafter begin to lose effectiveness and many patients even deteriorate to initial levels. For this reason, clinical trials should monitor effectiveness for at least 3 years. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Luengo-Castro, M. A., Fernández-Menéndez, J., García-Montes, J. M., Caunedo-Riesco, P. J., García-Haro, J. M., Braña-Menéndez, B., González-Díaz, D., Cabero-Álvarez, A., Cuesta-Izquierdo, M. (2024). Multicenter randomized clinical trial of brief psychotherapy versus usual treatment for common mental disorders in adults. Clinical and Health, 36(1), 9-18. https://doi.org/10.5093/clh2025a2 Funding This research has been financed exclusively by the Health Service of the Principality of Asturias and by the authors themselves. It has not received funding from other public agencies, commercial sectors or non-profit entities. References |
Cite this article as: Luengo-Castro, M. A., Fernández-Méndez, J., García-Montes, J. M., Caunedo-Riesco, P. J., García-Haro, J. M., Braña-Menéndez, B., González-Díaz, D., Cabero-Álvarez, A., & Cuesta-Izquierdo, M. (2025). Multicenter Randomized Clinical Trial of Brief Psychotherapy versus Usual Treatment for Common Mental Disorders in Adults. Clinical and Health, 36(1), 9 - 18. https://doi.org/10.5093/clh2025a2
Correspondence: (marcoluengocastro@yahoo.es) (M. A. Luengo Castro).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







