
Psychometric Properties of the Childbirth Expectation Questionnaire in a Sample of Spanish Pregnant Women
[Las propiedades psicométricas del Cuestionario de Expectativas sobre el Parto en una muestra de mujeres españolas gestantes]
Verónica Martínez-Borba1, Carlos Suso-Ribera1, Patricia Catalá2, Dolores Marín3, and Cecilia Peñacoba-Puente2
1Jaume I University, CastellĂłn, Spain; 2Rey Juan Carlos University, Madrid, Spain; 3Hospital Universitario de Fuenlabrada, Madrid, Spain
https://doi.org/10.5093/clysa2021a10
Received 28 July 2020, Accepted 22 January 2021
Abstract
Childbirth expectations during pregnancy are important factors related to birth satisfaction. The aim of this study is to validate the Childbirth Expectation Questionnaire (CEQ) in a sample of Spanish pregnant women; 231 women responded to the CEQ during their first trimester of pregnancy and 106 of them completed a re-test at the third trimester. Exploratory analyses with 1-to-6 factor solutions were carried out to investigate the internal structure of the CEQ. The three-factor solution (spousal support and control, medical support and environment, and labor pain and distress) showed the best properties in terms of model fit, number of items per factor, and item loadings. The internal consistency of scales was also good (.79 ≥ α ≤ .93). Test-retest analyses showed significant intercorrelations between expectations from the first to the third trimester of pregnancy. There is a need to assess childbirth expectations, and our results suggest that the CEQ is a valid and useful instrument to be used among Spanish pregnant women.
Resumen
Las expectativas sobre el parto (evaluadas durante el embarazo) constituyen factores relevantes relacionados con la satisfacción del parto. El objetivo de este estudio es validar el Cuestionario de Expectativas sobre el Parto (CEQ según las siglas del nombre inglés) en una muestra de gestantes españolas. Un total de 231 mujeres cumplimentaron el CEQ durante el primer trimestre del embarazo y 106 de ellas cumplimentaron de nuevo el instrumento en el tercer trimestre. Se realizaron análisis exploratorios con soluciones factoriales de 1 a 6 factores para analizar la estructura interna del CEQ. La solución de tres factores (apoyo de la pareja y control, apoyo médico y ambiente y dolor durante el parto y malestar) mostró las mejores propiedades en cuanto a ajuste del modelo, número de ítems por factor y peso de los ítems. La consistencia interna de las escalas también fue buena (.79 ≥ α ≤ .93). Los análisis test-retest mostraron intercorrelaciones significativas entre las expectativas del primer y tercer trimestre del embarazo. Atendiendo a la necesidad de evaluar las expectativas sobre el parto, nuestros resultados sugieren que el CEQ es un instrumento válido y útil para ser utilizado en las gestantes españolas.
Palabras clave
Expectativas sobre el parto, Embarazo, Análisis factorial exploratorio, Propiedades psicométricas, ValidaciónKeywords
Childbirth expectation, Pregnancy, Exploratory factor analysis, Psychometrics, Validation studyCite this article as: Martínez-Borba, V., Suso-Ribera, C., Catalá, P., Marín, D., and Peñacoba-Puente, C. (2022). Psychometric Properties of the Childbirth Expectation Questionnaire in a Sample of Spanish Pregnant Women. ClĂnica y Salud, 33(1), 1 - 9. https://doi.org/10.5093/clysa2021a10
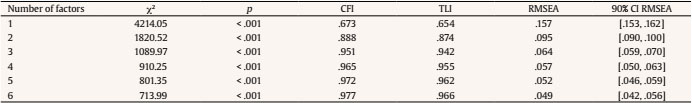
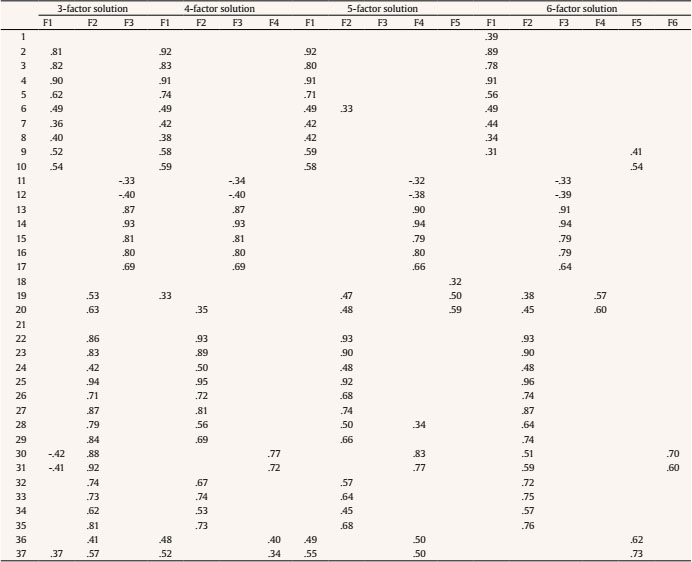
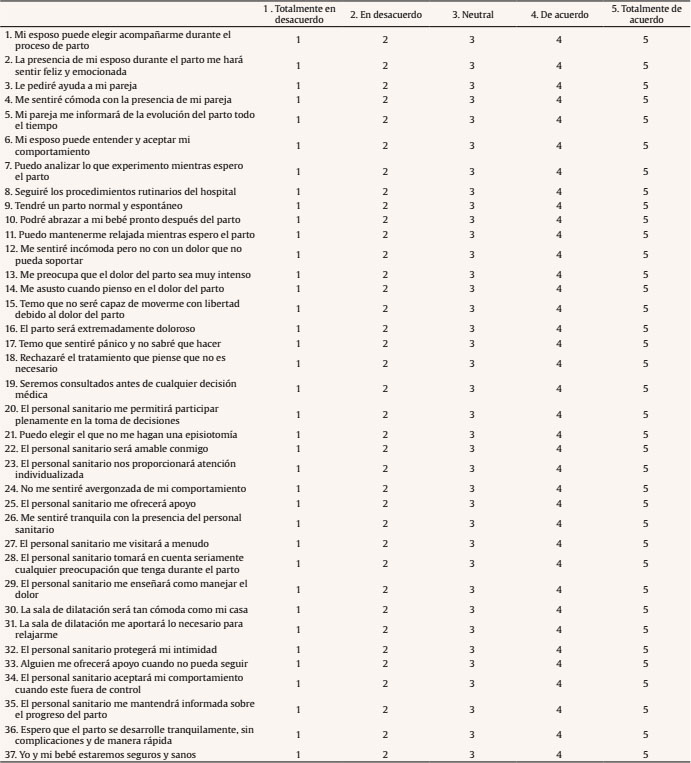
cecilia.penacoba@urjc.es Correspondence: cecilia.penacoba@urjc.es (C. Peñacoba-Puente).Childbirth expectations can be defined as the extent to which a mother feels that the needs associated with her and her baby’s well-being are met during childbirth (Iravani, 2015). These expectations are conceptualized as a complex construct which includes a lot of variables, such as physiological needs (e.g., nutritional needs or physical comfort), psychological needs (e.g., empathy, emotional support, and encouragement), informational needs (e.g., plan of care and procedures), social and relational needs (e.g., communication to health care professionals, familiar attendant), esteem needs (e.g., self-efficacy or participation in decision), security needs (e.g., coping with pain, domination of fear of childbirth), and medical needs (e.g., prevention of unnecessary intervention; Iravani et al., 2015). Research has shown that during pregnancy women anticipate their prospective childbirth experience, and it has been shown that these childbirth expectations are important predictors of childbirth outcomes (Camacho-Morell & Esparcia, 2019; Christiaens et al., 2008). In this sense, expectations play a fundamental role in satisfaction with birth experience (Camacho-Morell & Esparcia, 2019) and, when these are not met or are incongruent with childbirth experience, mothers tend to present decreased well-being (Camacho-Morell & Esparcia, 2019; Hollander et al., 2017). Specifically, research has shown that expectations regarding women’s ability to manage childbirth, pain, and partner support could be related to specific attitudes and behaviors during pregnancy. It has been suggested that perceived self-efficacy in managing childbirth has been shown to increase a mother’s motivation to do adequate efforts during pregnancy and has been suggested to impact women’s choices such as type of preferred birth (Ayers & Pickering, 2005; Iravani et al., 2015; Marques, et al., 2019; Rahmawati et al., 2019). Furthermore, a recent study in teenage mothers found that women who anticipated low pain relief or low partner support during childbirth showed a passive attitude when preparing for childbirth (Rahmawati et al., 2019). Several measures of childbirth expectations exist (Marques et al., 2020), though the Childbirth Expectations Questionnaire (CEQ; Beaton & Gupton, 1990; Gupton et al., 1991) received increased attention in the past decades because it evaluates expectations, as opposed to fear of childbirth, and because it includes a comprehensive set of childbirth-related domains (Iravani et al., 2015). While some studies have used the CEQ to assess childbirth expectations in the past (Farley, 1999; Kuo et al., 2010), the psychometric properties of the scale and their cross-cultural adequacy, however, have been rarely investigated and, as we will describe in more detail below, the scale has suffered important changes in factor structure and number of items since its initial development. When the CEQ was originally created (Beaton & Gupton, 1990), seven categories were identified after a series of interviews with 11 pregnant women. The categories created were: childbirth concerns (i.e., women expressed fear of the unknown), childbirth emotions (i.e., women expected to feel excited, tired, and anxious), pain and coping (i.e., they would cope with pain through activity, and relied on someone else to help them cope), role of support person (i.e., they hoped that their partner would help them to maintain control), role of health professionals (i.e., they expected that physicians would be present only if complications existed), intervention (i.e., women preferred not having many procedures or drugs), and childbirth environment (i.e., women who received a previous tour described the hospital as “home-like”, while women who had not visited the hospital previously described the place as “cold” and “impersonal”). Based on these reports, the authors created 100 statements that were grouped into five dimensions (i.e., pain, self-efficacy, intervention, significant other, and environment). A more in-depth analysis of the scale by experts and using statistical procedures resulted in a reduction from 100 to 36 items, grouped into 4 factors. For instance, pain and self-efficacy loaded on the same factor, so the authors concluded that these items were related to the same construct, namely, women’s expectations about their ability to cope with pain during childbirth. However, this scale was again revised and 14 items were added in a new 50-item version of the CEQ, which was considered to address 5 components of childbirth expectations, namely pain/coping, significant other, intervention, nursing support, and control. Subsequent analyses failed to demonstrate the existence of a control scale, so a reduction of the scale was carried out, this yielding a final version made up by 35 items, grouped into 4 subscales: coping with pain (11 items), support by the significant other (7 items), nursing support (8 items), and medical intervention (9 items; Gupton et al., 1991). To date, only one study has validated the CEQ and explored its psychometric properties and factorial structure, specifically in a Chinese population (Kao et al., 2004). In contrast to the original version (Gupton et al., 1991), the authors obtained a 5-factor solution of the CEQ, namely caregiving environment, labor pain expectation, spousal support, control and participation, and medical support. Because different factor solutions have emerged in previous studies with the CEQ (Gupton et al., 1991; Kao et al., 2004) and there is no Spanish adaptation of this questionnaire, the aim of this study has been to obtain a validated version of the CEQ to be used in Spanish women during pregnancy. A secondary goal has been to explore differences in expectations as a function of sociodemographic and obstetric characteristics. Because the psychometric properties of the 37-item version of the CEQ have only been studied by Kao et al. (2004), we expect to replicate the 5-factor structure obtained in a sample from China, even though cultural differences surely exist between eastern and western cultures (Kim et al., 2010). We also expect to find high test-retest indices (when assessed during the first and the third trimester) because childbirth expectations have been shown to be relatively stable during pregnancy (Peñacoba-Puente et al., 2016). Procedures and Sample In this prospective cohort study, midwifes made the first contact with the participants at the antenatal clinic of Hospital Universitario de Fuenlabrada in South Madrid on the day of their first planned ultrasound during the first trimester. Firstly, midwives checked the electronic clinical records of women who had an appointment planned at the clinic for the following days. Women who met the inclusion criteria, that is, being over 18 years of age, understanding Spanish, having low obstetric risk, and being pregnant, were approached with information about the study and were invited to voluntarily join during their appointment to perform the first pregnancy ultrasound. Women freely gave written informed consent before being enrolled in the study. This study is a secondary analysis, part of a larger study that explores changes in the mental well-being of women during the perinatal period and its correlates Fondo de Investigaciones Sanitarias PI07/0571. The Ethics Committee of Hospital Universitario de Fuenlabrada approved all procedures described in this study. Between October 2013 and April 2015, a total of 280 women were approached to participate in the study, among them a total of 234 (83.57%) agreed to participate in the study, signed the informed consent form and completed the CEQ. The completed questionnaire was returned directly to the researcher. Three of the participants suffered miscarriages during this period and were therefore excluded from the analysis, leaving 231 expectant mothers to make up the final sample at the initial data collection point (at the end of first trimester). In the third trimester (around week 30), the same questionnaire was mailed to women with a prepaid envelope for returning the completed questionnaire to the research team. Before being sent the questionnaire, each participant’s medical record was reviewed to confirm that there had been no alterations in the course of pregnancy. Five women had a spontaneous miscarriage during the first half of pregnancy after completing the first questionnaire. The remaining enrolled women received a telephone call in which they were asked to return the questionnaire upon completion. Thus, 226 questionnaires were mailed in the third trimester and 106 of these were returned (46.9%). Measures Sociodemographic and obstetric characteristics. Ad hoc questions were created to assess age, educational level, employment status, history of previous childbirth, history of previous miscarriages, and whether pregnancy was planned or not. Childbirth Expectation Questionnaire (CEQ; Beaton & Gupton, 1990; Gupton et al., 1991; see CEQ Spanish version in the Appendix). In this study, the most recent adaptation of this self-administered questionnaire was used (Kao et al., 2004). For this adaptation, a series of revisions were conducted by Kao et al. (2004). First, expectant parents in the third trimester of pregnancy were asked about childbirth expectations and 12 items were added to the original 35-item CEQ. Second, experts (i.e., doctorate scholars of obstetrics, obstetric clinical experts, and obstetricians) were consulted to assess content validity of items. Third, 200 pairs of expectant parents were asked to complete the scale, and an exploratory factor analysis and item-total correlations were conducted. As a result, the CEQ final version was composed by 37 items, whose response rate range from 1 = strongly disagree to 5 = strongly agree. The authors obtained a 5-factor solution of the CEQ; these factors were: caregiving environment (13 items; e.g., “The clinical staff will protect my privacy”), labor pain expectations (5 items; e.g., “I am scared when I think of my labor pain”), spousal support (6 items; e.g., “I will ask my husband for help”), control and participation (9 items; e.g., “I can keep myself relaxed while awaiting labor”), and medical support (4 items; e.g., “The medical staff will offer me encouragement”). Items 13, 14, 15, 16, and 17 are reverse-coded in order to interpret higher scores as more positive expectations. The total score for each subscale varies depending on the number of items included in each scale (e.g., caregiving scale scores range between 13 and 65, pain expectations scores range between 5 and 25, spousal support scores range between 6 and 30, control and participation scores range between 9 and 45, and medical support scores range between 4 and 20). A total scale score can also be obtained ranging from 37 to 185. Higher scores represent more positive childbirth expectations. CEQ scales have shown good psychometric properties in previous research (α = .87; Kao et al., 2004). A back-translation procedure involving two bilingual translators was used to obtain the current adapted version of the CEQ. Data Analysis First, the demographic and obstetric characteristics of the sample were analyzed. Next, an exploratory factor analysis (EFA) was carried out using MPlus version 6.12 (Muthén & Muthén, 2011) to determine the number of latent variables required to explain the correlations among items. Because items are ordered categorically (ordinal), the weighted least square mean and variance adjusted estimator (WLSMV) is preferred (Li, 2016). Default MPlus rotation, oblique Geomin, was used because factors were expected to correlate. The implementation of an EFA allows comparing the model fit of different factor solutions. Frequently reported fit indices are chi-square test (χ2), comparative fit index (CFI), Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA). CFI and TLI values over .95 are usually interpreted as revealing an excellent fit. RMSEA values smaller than .05 are argued to show an excellent model fit of the data to the model, while scores smaller than .08 are interpreted as indicating a good fit (Hu & Bentler, 1999; Schreiber et al., 2006). In the present study, all these fit indices were compared for all obtained factor solutions. Because previous data reduction efforts with the CEQ have either proposed a 4-factor (Gupton et al., 1991) or a 5-factor solution (Kao et al., 2004), tests were performed from 1 to up to 6 factor solutions for the data. Only if none of the tested models showed an adequate fit, a solution with more factors was explored. This, however, would be undesirable because the intention of EFA and other similar strategies is to reduce the number of observed variables into a manageable (i.e., reduced) set of latent factors. As recommended in the literature, factor loadings with an absolute value smaller than .32, which corresponds to less than 10% of shared variance, were ignored (Tabachnick & Fidell, 2014). When selecting factor solutions to be retained, a minimum of three items per factor were required, but more were preferred for replicability (Raubenheimer, 2004). Once a satisfactory factor structure of the CEQ was obtained, the scale sum scores were calculated and a multivariate analysis of variance (MANOVA) was computed to explore differences in expectations as a function of categorical sociodemographic and obstetric characteristics of the sample (i.e., educational level, employment status, history of previous childbirth, history of previous miscarriages, and whether pregnancy was planned). A Pearson correlation was conducted to explore associations between age and expectations because both were continuous variables. Next, longitudinal analyses were performed. Pearson correlations were computed to evaluate changes in rank, also known as test-retest reliability, and paired-samples t-tests were analyzed to explore group score changes at mean-level. Participants were 231 pregnant women who completed the CEQ at first trimester of gestation. As Table 1 shows, their mean age was 31.31 (SD = 4.03, range 22-42), and the majority of participants were working at the time of this first assessment (n = 155, 67.4%). Regarding educational level, 66 women had primary studies (28.7%), 98 had completed secondary education (42.2%), and 67 had a university or equivalent degree (29.1%). Half of the women reported having a previous childbirth (n = 116, 50.7%) and 64 (27.7%) had suffered a previous miscarriage. All women were in stable relationships and had mostly (n = 190, 82.3%) planned their pregnancy. A subsample of the women (n = 106) also completed a re-test at the third trimester of gestation. Table 1 Sociodemographic Characteristics of Women Included in this Study (N = 231)  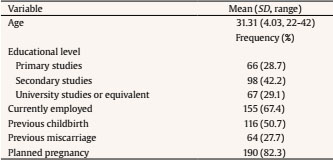 Note. 1N = subjects who enter the program; 2n = subjects who completed the program; 3obsessive-compulsive disorder; 4 substance-related disorders. CEQ Exploratory Factor Analysis The results of model fit for the 1-to-6 factor solutions of the CEQ are displayed in Table 2. Solutions with 3 to 6 factors obtained good to excellent fit indices (CFI and TLI over .90 and RMSEA below .08 in all cases). The model fit improved as the number of factors increased. Because 3-to-6 factor solutions had an adequate fit, the size of factor loadings and the distribution of items were investigated to choose the preferred model. These are presented in Table 3. Regarding the distribution of items (Table 3), the 6-factor and the 5-factor solutions were excluded because some of their factors had fewer than three items (i.e., factor 3 in the 5-factor solution and factors 4 and 6 in the 6-factor solution). The models with 3 and 4 factors were similar in terms of item distribution. However, one of the factors in the 4-factor solution was only composed of 4 items, two of which had higher loadings on a different factor. Therefore, the 3-factor solution was preferred due to parsimony. As seen in Table 3, some issues also emerged in this 3-factor solution. For example, items 1 (“My husband can choose to accompany me throughout the course of labor”), 18 (“I will refuse treatment I do not think is necessary”), and 21 (“I can choose not to have an episiotomy”) did not obtain sufficiently large loadings on any of the factors and some items had cross-factor loadings (items 30, 31, and 37). The same problems emerged in the other factorial solutions, so the decision to select the 3-factor solution remained unchanged. In fact, factor loadings in the items with cross-factor loadings were sufficiently large in one of the factors (factor 2) to suggest their inclusion in this factor only. After an analysis of item distribution and based on previous research with the scale (Kao et al., 2004), factor 1 was named “spousal support and control”, factor 2 was called “medical support and environment”, and factor 3 was labeled “labor pain and distress”. To assess the test-retest reliability of the questionnaire, the three factors were calculated based on factor loadings in Table 3. As noted earlier, when calculating scale scores, items 30, 31, and 37 were grouped into factor 2 only. Items 1, 18, and 21 were not included in any scale. Internal consistency was good in all three subscales: spousal support and control (α = .79) medical support and environment (α = .93), and labor pain and distress (α = .84). This internal consistency did not improve by removing any of the items. CEQ Differences as a Function of Sociodemographic and Obstetric Variables As shown in Table 4, there were significant differences in childbirth expectations in Factor 1 as a function of planned pregnancy (F = 6.07, p = .015) and differences in Factor 3 as a function of history of previous childbirth (F = 23.79, p < .001). Women whose pregnancy was planned had higher expectations regarding spousal support and control (mean = 39.17, SD = 0.33) than women who did not plan their pregnancy (mean = 37.49, SD = 0.64). Also, women who had previously given birth had lower expectations regarding labor pain and distress (mean = 20.42, SD = 0.45) compared to primiparous women (mean = 23.03, SD = 0.48). There were no significant differences in expectations as a function of age, job, educational level, or previous miscarriage (all p >.050). Table 4 Differences in Expectations as a Function of Sociodemographic and Obstetric Characteristics  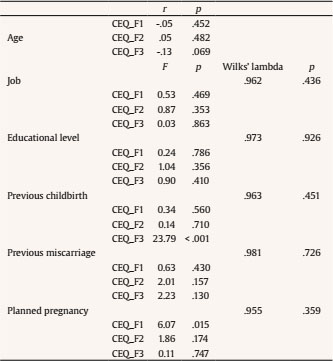 Note. CEQ_F1 = spousal support and control; CEQ_F2 = medical support and environment; CEQ_F3 = labor pain and distress. Changes in Order and Mean-level in the CEQ during Pregnancy Analyses of changes in the CEQ are presented in Tables 5 and 6. Pearson correlations were computed to evaluate changes in order/rank, also known as test-retest reliability, and paired-sample t-tests were analyzed to explore group score changes at mean-level. Moderate-to-strong associations were obtained for test-retest intercorrelations between the CEQ scales (all r > .50, p < .001). Factors 1 and 2 were also moderately correlated both at first (r = .48, p < .001) and third trimester (r = .67, p < .001). Factors 2 and 3 and factors 1 and 3 were mildly correlated (all rs ≤ .20). Table 5 Intercorrelations and Test-retest Correlations of the CEQ Scales (n = 106)  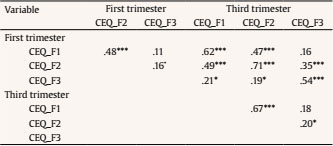 Note. CEQ_F1 = spousal support and control; CEQ_F2 = medical support and environment; CEQ_F3 = labor pain and distress. ***p < .001, **p < .01, *p < .05. The analysis of changes at mean level indicated that F1 and F2 remained unchanged (all ps > .05), while F3 slightly increased in the third trimester (t = -2.38, 95% CI [-1.35, -0.12], p = .019). Table 6 Means, Standard Deviations, and Mean-level Changes in CEQ Scales (N = 106)  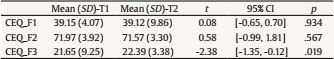 Note. CEQ_F1 = spousal support and control; CEQ_F2 = medical support and environment; CEQ_F3 = labor pain and distress. The current study presents a Spanish validation of the CEQ, a childbirth expectations questionnaire that could be used by Spanish nurses, midwifes, gynecologists, and psychologists working in the field of perinatal care. As a secondary objective, we aimed to explore differences in expectations as a function of sociodemographic and obstetric variables. Overall, our exploratory factor analyses showed a good fit adjustment of 3-to-6 factor solutions, which again supports the idea that childbirth expectations are a multidimensional concept. However, differently to the Chinese adaptation of the CEQ (Kao et al., 2004), the three-factor solution was preferred after considering the number of items per factor and their corresponding factor loadings. A longitudinal design was implemented, following the recommendations by CEQ authors (Gupton et al., 1991), and results supported test-retest reliability of the scale. In our study, the first factor was named “spousal support and control”. Consistent with the original development of the CEQ (Gupton et al., 1991), our analyses failed to reveal an isolated “control” factor. In our sample, these items were found to be related to other factors. Specifically, when compared with the Chinese adaptation of the CEQ (Kao et al., 2004), our “spousal support and control” scale grouped together the spousal support factor (6 items) and control scales (3 items), but also added an item which had previously been assigned to caregiving environment (Kao et al., 2004). In relation to the latter, it seems that Spanish women understand item 10, “I can hold my baby soon after childbirth”, as an expectation about their own capacity to control childbirth situation, as opposed to an item reflecting caregiving environment. Thus, it is possible that they think that they will have some control over the moment when they will be able to be in contact with their baby. Because this item was categorized into “caregiving environment” in the study by Kao et al. (2004), it is possible that Chinese women think that being with their baby largely depends on a medical decision that is somehow out of their control. As suggested in a recent study, it seems that the definition of “control” is culture-dependent and women in different cultures understand this in different ways (Moore, 2016). As lack of control seems to be one of the factors most strongly associated to bad or traumatic childbirth experiences (Hollander et al., 2017), it is important to provide pregnant women with information about childbirth procedures and to discuss their choices with them at different stages during birth. Preparation of a woman throughout her pregnancy includes biological but also social, psychological, and cultural factors (Nereu et al., 2013). Our results also showed that the second factor, namely “medical support and environment”, included items from both “nursing” and “intervention” factors of the original CEQ (Gupton et al., 1991). Similarly, compared to the Chinese version, current “medical support and environment factor” was composed of almost all caregiving environment items, all medical items, and 2 control and participation items from the Chinese adaptation of the CEQ (Kao et al., 2004), which justifies scale’s name. To discuss this second factor solution, we need to explain the concept of “control” as defined by Cheung (2002). This author proposed that control and choices are a result of the interplay between five factors: maternity professionals, social context, body/baby, obstetric technology, and women. The 2 items from the “control” factor in the Chinese adaptation of the CEQ (“We will be consulted before any medical decision-making” and “The medical staff will allow me to fully participate in labor decision making”) seem to be understood by our Spanish sample as related to external decisions which mostly depend on maternity professionals. A second important consideration in relation to this second factor is the fact that environment items (e.g., “The delivery room is as comfortable as my home”) were perceived as corresponding with professional care items (e.g., “The medical staff will offer me encouragement”). The fact that women understand these environmental items as part of the medical decisions factor leads us to think that women perceived little control over childbirth environment, but they expected that this environment would allow them to feel comfortable. Thus, in an attempt to provide a greater sense of control and familiarity to women, visits to the hospital could be made to familiarize mothers with the medical context in which childbirth will occur and, therefore allowing their expectations to be adjusted (Camacho-Morell & Esparcia, 2019). Finally, although previous CEQ versions showed a separate pain factor (Gupton et al., 1991; Kao et al., 2004), our results showed that our third factor, named “labor pain and distress”, was composed of all items from the “labor pain expectations” factor and 2 items from the “control and participation” factor found in the Chinese adaptation of the CEQ (Kao et al., 2004). In our sample, items 11 (“I can keep myself relaxed while awaiting labor”) and 12 (“I will feel uncomfortable but not with pain I cannot endure”) appear to be interpreted as feelings of relaxation and comfort and are more strongly related to distress and pain expectations than to a sense of control. Congruent with this idea, in this factor we found other items that were related to distress, such as item 17, “I am afraid I will panic and not know what to do”, which supports the idea that these items correspond to distress and not to control. This could also indicate that women perceive pain as something unavoidable (Kao et al., 2004), so they might hope to successfully cope with pain and to be relaxed but might not believe that they can avoid feeling pain. Education could be useful in this sense. For example, operative deliveries have been argued to be a risk factor for negative birth experience because they are often not explained previously to childbirth and women feel they are unprepared for the pain they can experience before, during, and after these scenarios (Hollander et al., 2017). In Spain, pregnant women rated professional sources (i.e., midwifes, gynecologists, and childbirth preparation) as being sources of best quality and most useful information (Camacho-Morell & Esparcia, 2019). Therefore, it would be preferable if midwives and nurses explored women’s expectations, such as in the CEQ, to detect unrealistic or problematic expectations and to provide accurate information that helps women to reduce maladaptive fears. With the exception of items 1, 18, and 21, which did not obtain sufficiently strong loadings to justify their inclusion in any of the factors, our results suggest that CEQ is a useful and valid instrument for the evaluation of expectations in Spanish pregnant mothers. Items 1 and 18 have also obtained relatively lower factor loadings in previous research compared to other items in their corresponding scale (Kao et al., 2004). Regarding item 21, it is possible that some women do not understand what an episiotomy is, which might explain the results. We suggest changing the item to “I can choose not to have an episiotomy (an incision between the vagina and the anus)”. In our study we decided to remove items 1, 18, and 21 from the scale because including them would affect internal consistency of the scale. The original CEQ also found that 6 items did not load on any factor, and some scale items appear to work better than others (Gupton et al., 1991). Future studies in similar sociodemographic populations are needed to replicate these findings and to provide further evidence on the exact items that should be removed from the scale. Our analyses also revealed that three items, that is items 30, 31, and 37, loaded both on factors 1 and 2. Because cross-loadings are psychometrically and conceptually problematic, we decided to assign items to the “medical support and environment” factor after considering the size of factor loadings and the conceptual correspondence between factors and item content. For example, items 30, “The delivery room is as comfortable as my home”, and 31, “The delivery room can provide soft music and help me relax”, are related to room characteristics (e.g., comfort and relaxation). While these items were partly linked to the “spousal support and control” factor, probably because of their reference to control, women were more likely to understand these items as referring to environmental or medical factors according to factor loadings, which is also consistent with item content. Regarding item 37, “I and my baby will be safe and healthy”, this refers to safety for mother and baby and could be interpreted in two ways: (i) women perceive having control over the situation, so they expect being healthy and safe (factor 1: spousal support and control), (ii) women perceive that their own and baby’s safety depends on healthcare professionals (factor 2: medical support and environment). Given that item 37 loaded more on the latter, we suggest that mothers’ expectations about being healthy and safe are understood as largely dependent on healthcare professionals as opposed to their own behavior. A novel analysis in the present study relates to CEQ test-retest stability. Our analyses showed moderate-to-high correlations in mothers’ expectations from first to third trimester of pregnancy. This indicates that women who had higher expectations early during pregnancy continue to have similarly high expectations later on during pregnancy. In addition, the analysis of change at mean level showed that factor 1 and 2 remained stable from first to third trimester of pregnancy while factor 3 expectations increased. This means that expectations remain relatively stable across pregnancy (Peñacoba-Puente et al., 2016), especially regarding spousal support, control, medical support, and environment. Overall, these results suggest that prenatal care should include the assessment of expectations early during pregnancy in order to address them as soon as possible. In contrast to the remaining factors, however, mean-level increase in factor 3 (labor pain and distress) appears to suggest that, as childbirth gets closer, women become more prepared and relaxed about childbirth pain and distress, that could be due to their interactions with professionals. Regarding psychometric properties of the CEQ, in the present study we also investigated the internal consistency of its subscales and factor loadings of items for each subscale. Past research had revealed a Cronbach’s alpha coefficient of .87 for the whole CEQ (Kao et al., 2004). This study also obtained factor loadings over .32 for all items, which is the recommended cutoff for absolute values of factor loadings (Tabachnick & Fidell, 2014). In contrast to findings by Kao et al. (2004), the present study found that Cronbach’s alphas were calculated for subscales, which is more consistent with the factorial solution proposed. Obtained alphas were between .79 and .93, which are similar values to the ones indicated in the aforementioned study. Furthermore, in a similar manner to what was found by Kao et al. (2004), all factor loadings presented in the current study were above .32 cutoff. Regarding sociodemographic variables, our results indicated that women with planned pregnancies expected more support from their partner and more control over childbirth process, which is consistent with the idea that pregnancy was agreed between the two and, therefore, the partner should be actively involved in the process. Given that support during pregnancy is associated to better mental health during pregnancy (Friedman et al., 2020), special attention should be paid to women with unplanned pregnancies, according to our findings. Our results also show that multiparous women had lower expectations regarding labor pain and distress. This means that women who have previously given birth expect childbirth to be more painful and distressful than primiparous women. Previous studies have found that primiparous women have lower childbirth expectations, specifically it was found that they perceived childbirth as more difficult than multiparous women (Christiaens et al., 2008; Hauck et al., 2007; van Bussel et al., 2010). In the light of our results, it seems that women acquire experience with childbirth (Stevens et al., 2011) and develop more realistic expectations, at least regarding labor pain and distress. The present study is not without limitations. First, the study sample is composed by heterosexual women with a partner, which might limit the generalizability of our results. Future research should explore if our findings are replicated in women with different sociodemographic characteristics (i.e., single mothers or homosexual couples). In this regard, the CEQ includes non-inclusive wording when referring to partner support (e.g., “my husband”). This is problematic as single women or homosexual couples might feel excluded. Future CEQ developments should be more inclusive, for instance by changing “my husband” to “my partner” or “my family”. As some women prefer being assessed for perinatal mental health alone (Osma et al., 2020), we did not include their partners in our assessments. Previous studies have found that women expect high partner support during childbirth (Kao et al., 2004); therefore, by assessing both parents’ expectations we could ensure that partners are aware of their role and this would help by providing them with useful skills (i.e., communication abilities or birth instructions) to use during labor. Another shortcoming was that only 106 from the 231 initial sample responded to re-test assessment, so the sensitivity to group change could only be calculated in these participants. Another limitation is that we did not explore relationships between psychological status and expectations. While anxiety or depressive symptoms could affect childbirth expectations (Chen et al., 2000), it is important to explore mental health in pregnant mothers so as to be able to provide adequate interventions focused on these symptoms. It is also necessary to note that all women with low obstetric risk who were in care at Hospital Universitario de Fuenlabrada were included in this study. Major physical problems (i.e., chronic pain), however, were not assessed in the eligible sample. This could be problematic as chronic pain is a major problem during the perinatal period that may make labor even more difficult and can impact women’s expectations (i.e., women with chronic pain express anxiety of delivery due to the anticipation of pain) (Ray-Griffith et al., 2018). Due to the importance of pain in labor, it has been proposed that women suffering chronic pain conditions should develop a pain management plan for labor and delivery in collaboration with professionals (Ray-Griffith et al., 2018). Other high risk medical conditions, such as having a multiple pregnancy, have been shown to affect childbirth expectations (Fenwick et al., 2005). In the present study, however, all women had low obstetric risk and none presented multiple pregnancies. Therefore, the results might not be generalizable to women at high obstetric risk. Finally, results correspond to women who were in care at Hospital Universitario de Fuenlabrada so the findings may not be generalizable to other settings as private hospitals. As place of birth (home vs. hospital) seems to affect childbirth expectations (Christiaens et al., 2008), it is possible that difference in hospitals could also translate to differences in expectations, for instance, women would not expect to have a water birth if the hospital does not offer it. While acknowledging previous limitations, this is the first study to explore the internal structure and psychometric properties of the CEQ in a Spanish sample of pregnant women. Childbirth expectations are important in the construction of the mother’s role (Marques et al., 2020) and professionals who are in constant contact with pregnant women should assess these expectations to favor a correct adjustment to motherhood. The validation of the CEQ conducted in the present study might facilitate the aforementioned goal by providing Spanish midwifes and nurses with a psychometrically sound tool for the assessment of childbirth expectations in pregnant women. Once the assessment is made, childbirth programs may help to discuss these expectations and to promote realistic ones while maintaining positive emotions. The administration of the currently validated CEQ before and after these programs would be important to reveal their effectiveness. Nowadays, perinatal interventions are patient-centered and their principal aim is to increase maternal comfort during birth (Kao et al., 2004; van Bussel et al., 2010). In Spain different efforts are emerging to promote perinatal psychology assessments and treatment (Rodríguez-Muñoz et al., 2016). In light of our results, women’s childbirth expectations appear to be key factors associated with birth experience. Childbirth dissatisfaction has been associated with negative consequences for mother and baby, so we must help women to achieve their goals as well as to adjust expectations about labor in order to reach a better adjustment in postpartum. According to women’s reports (Camacho-Morell & Esparcia, 2019), some changes in our healthcare system could include: giving more time during antenatal appointments, being more emphatic and delivering personalized treatments, flexibility in preparation classes, visiting the birthing center, using information and communications technologies (ICT; i.e., telephone, e-mail, or app-based solutions) to solve doubts, and providing information on the emotional aspects of the perinatal period. In this sense, ICT could help to overcome some of the traditional face-to-face barriers and could be developed to support information delivered by healthcare professionals. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgement We want to thank all the participants of the present study. Funding: The study was funded by the Health Research Fund [Fondo de Investigaciones Sanitarias, FIS], grant number PI07/0571 from the Instituto de Salud Carlos III (Spain). Cite this article as: Martínez-Borba, V., Suso-Ribera, C., Catalá, P., , Marín, D., & Peñacoba-Puente, C. (2021). Psychometric properties of the childbirth expectation questionnaire in a sample of Spanish pregnant women. Clínica y Salud, 33(1), 1-9. https://doi.org/10.5093/clysa2021a10 References Appendix Childbirth Expectation Questionnaire - Spanish Version A continuación, se muestran una serie de afirmaciones que describen posibles modos de concebir el parto y el nacimiento de un/a hijo/a. Se trata de que describa cómo siente estos fenómenos en este momento. Para ello debe indicar en cada una de las afirmaciones hasta qué punto se identifica con ellas de acuerdo a las siguientes categorías: |
Cite this article as: Martínez-Borba, V., Suso-Ribera, C., Catalá, P., Marín, D., and Peñacoba-Puente, C. (2022). Psychometric Properties of the Childbirth Expectation Questionnaire in a Sample of Spanish Pregnant Women. ClĂnica y Salud, 33(1), 1 - 9. https://doi.org/10.5093/clysa2021a10
cecilia.penacoba@urjc.es Correspondence: cecilia.penacoba@urjc.es (C. Peñacoba-Puente).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







