
Perfectionism, Intolerance of Uncertainty, and Fear of Childbirth in Pregnant and Non-pregnant Women
[El perfeccionismo, la tolerancia a la incertidumbre y el miedo al parto en mujeres embarazadas y no embarazadas]
Anđela Kuljanac1, Maja Brekalo2, and Sandra Nakić Radoš2
1Kindergarten Svemirko, Srebrnjak, Zagreb, Croatia; 2Department of Psychology, Catholic University of Croatia, Zagreb, Croatia
https://doi.org/10.5093/clysa2023a17
Received 19 July 2022, Accepted 24 May 2023
Abstract
Background: Fear of childbirth (FOC) has adverse effect on delivery, maternal and infant health. This study aimed to examine the prevalence of FOC and to examine the role of perfectionism, intolerance of uncertainty, and preparedness for childbirth in explaining FOC in non-pregnant and pregnant women, as well as the role of mode of delivery in multiparous women. Method: In the cross-sectional study, 197 non-pregnant, 168 nulliparous and 124 multiparous pregnant women filled out questionnaires on FOC (W-DEQ), perfectionism (PNPS), intolerance of uncertainty (IUS), and a question on preparedness for childbirth. Results: More important determinants of FOC were personality traits (perfectionism and intolerance of uncertainty) in non-pregnant and nulliparous pregnant women, as opposed to previous childbirth experience (emergency caesarean section) in multiparous women. However, preparedness for childbirth was associated with FOC in all three sub-groups. Conclusion: Preparedness for childbirth should be the target in prenatal classes in order to alleviate FOC.
Resumen
Antecedentes: El miedo al parto (MP) influye de un modo adverso en el mismo y en la salud materna e infantil. El estudio tiene por objeto analizar la prevalencia del MP y el papel del perfeccionismo, la intolerancia a la incertidumbre y la preparación para el parto para explicar el MP en mujeres embarazadas y no embarazadas así como el papel que juega el modo de alumbramiento en mujeres multíparas. Método: En el estudio transversal 197 mujeres no encintas, 168 embarazadas nulíparas y 124 multíparas cumplimentaron cuestionarios sobre MP (W-DEQ), perfeccionismo (PNPS), intolerancia a la incertidumbre (IUS) y una pregunta sobre preparación para el parto. Resultados: Los determinantes más importantes del MP fueron los rasgos de personalidad (perfeccionismo e intolerancia a la incertidumbre) en mujeres no encintas y en embarazadas nulíparas en oposición a la experiencia previa de parto (cesárea de emergencia) en mujeres multíparas. No obstante, la preparación para el parto se asociaba al MP en los tres subgrupos. Conclusión: La preparación para el parto debería abordarse en las clases prenatales para aliviar el MP.
Palabras clave
Miedo al parto, Perfeccionismo, Intolerancia a la incertidumbre, Preparación para el parto, CesáreaKeywords
Fear of childbirth, Perfectionism, Intolerance of uncertainty, Preparedness for childbirth, Caesarean sectionCite this article as: Kuljanac, A., Brekalo, M., & Radoš, S. N. (2023). Perfectionism, Intolerance of Uncertainty, and Fear of Childbirth in Pregnant and Non-pregnant Women. ClĂnica y Salud, 34(2), 65 - 70. https://doi.org/10.5093/clysa2023a17
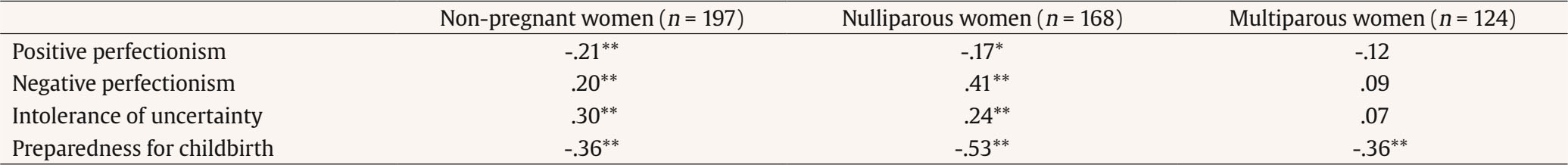
Correspondence: snrados@unicath.hr (S. Naki Radoš).Fear of childbirth (FOC) can be defined as an anxiety disorder or specific phobia (tokophobia), which can be primary or secondary. In women who still did not give birth, it is a primary phobia, while if it is developed after childbirth is called a secondary phobia (Nilsson et al., 2018). It is an emotional burden for women and could have adverse outcomes for both women and infants. For example, a systematic review showed that it is associated with longer labour duration, use of epidural, and some obstetric complications (Dencker et al., 2019). Also, FOC could heighten the risk for mental health issues (Rouhe et al., 2011). Around 80% of pregnant women report their concerns regarding pregnancy and delivery (Melender, 2002). The prevalence of FOC has been increasing in the last thirty years, and severe levels of FOC were found from 4% to 43%, depending on the country (O’Connell et al., 2017). Furthermore, the prevalence of FOC is higher in first-time pregnant women compared to multiparous women (Jokić-Begić et al., 2014; O’Connell et al., 2017), but some studies did not show differences in the FOC levels between nulliparous and multiparous women (Hall et al., 2009). In multiparous women, one of the predictors of FOC is previous negative birth experiences or operative delivery, as shown in a systematic review (Dencker et al., 2018). However, in FOC, fear could be observed as a personality disposition that activates a vicious cycle, so women experience what they were afraid of initially, which perpetuates the cycle of fear (Zar et al., 2001). Indeed, several personality traits were found to be associated with FOC, such as higher neuroticism (Handelzalts et al., 2015), trait anxiety (Jokić-Begić et al., 2014), and anxiety sensitivity (Handelzalts et al., 2015; Jokić-Begić et al., 2014). Furthermore, it could be expected that women with perfectionistic tendencies want their labour and childbirth to be perfect and without complications, so one of the possible correlates of FOC could be perfectionism. At first, perfectionism was considered as a negative construct. However, perfectionism could be distinctive as positive (adaptive) and negative (non-adaptive). Individuals with high positive or adaptive perfectionism feel satisfied when they accomplish a goal. In contrast, individuals with negative perfectionism think they did not perform at an optimum level, so they set unrealistic goals (Buhr & Dugas, 2006). It was shown that negative perfectionism was related to depression, anxiety, anger, fatigue, and confusion in pregnant women (Macedo et al., 2009). Also, negative perfectionism predicted higher FOC in pregnant women, while positive perfectionism was a protective factor, especially in nulliparous pregnant women (Ercegovac, 2013). To our best knowledge, there is no evidence of a relation between perfectionism and FOC in non-pregnant women. Individuals with high perfectionism have less tolerance toward uncertainty, but it is unclear whether it is more related to positive or negative perfectionism (Buhr & Dugas, 2006). Intolerance of uncertainty describes how an individual perceives information and reacts in ambiguous situations. Persons with high levels of intolerance to uncertainty often perceive ambiguous situations as unfavourable and tend to avoid them (Buhr & Dugas, 2006). Also, intolerance of uncertainty was associated with anxiety-related psychopathology and was related (along with anxiety sensitivity) to the origin of the fear of the unknown (Carleton et al., 2007). Indeed, a previous study showed that intolerance of uncertainty predicted higher FOC in pregnant women (Rondung et al., 2018). However, this association has not been examined separately in nulliparous and multiparous women, which is essential because previous findings suggest that personality dispositions were critical for FOC in nulliparous women. In contrast, previous experiences were more important for multiparous women (Jokić-Begić et al., 2014). Moreover, this association still has not been examined in non-pregnant women. Indeed, FOC was more examined in pregnant rather than in non-pregnant women. However, studies show that FOC starts to develop before pregnancy, already in early adulthood (Stoll et al., 2014) and is associated with a history of anxiety disorders and experiences of other women (Nilsson et al., 2018). Furthermore, while severe FOC is present among 16% of nulliparous and 12% of multiparous pregnant women (O’Connell et al., 2017), it is concerning that one in four female students (26%) report severe FOC (Žigi Anti et al., 2019). Also, it is important to emphasize it because, due to FOC some adults do not plan to have children (Rondung et al., 2022). According to qualitative data, those women tend to use various strategies to avoid thinking about pregnancy and avoid becoming pregnant while simultaneously feeling pressured to decide about future pregnancy. Therefore, it is crucial to understand the mechanisms of FOC and its predictors in non-pregnant women to prevent adverse outcomes. Preparedness and education might have a protective role in decreasing FOC, especially since only one in five students think they are educated enough about childbirth (Hauck et al., 2016). Psychoeducation and psychological preparation and interventions were important for reducing FOC (Saisto et al., 2001; Toivanen et al., 2018). In summary, scarce literature shows that perfectionism and intolerance of uncertainty could be associated with FOC, but this is not examined separately in nulliparous and multiparous pregnant women, among which different mechanisms might lead to FOC. Additionally, the association between intolerance of uncertainty and FOC was still not examined in a sample of non-pregnant women. Also, perceived preparedness for childbirth was underexamined in non-pregnant and pregnant women. Therefore, the aims of this study were twofold: (1) to determine the prevalence of FOC in non-pregnant, nulliparous, and multiparous pregnant women, and (2) to examine whether positive and negative perfectionism, intolerance of uncertainty, preparedness for childbirth, and previous birth experiences (only in multiparous women) were associated with FOC. We expected that FOC would be the most prevalent in non-pregnant women. Still, due to the conflicting previous findings, we could not predict whether nulliparous pregnant women would have a higher prevalence of FOC than multiparous pregnant women. Also, we expected that lower positive, higher negative perfectionism, higher intolerance of uncertainty, and lower perceived preparedness for childbirth would be associated with higher levels of FOC in all three groups. In multiparous women, we expected that operative delivery of previous childbirth (emergency caesarean section or instrumental vaginal delivery) would be associated with FOC in the current pregnancy. Table 1 Sociodemographic Data and Differences between the Sub-groups (non-pregnant, nulliparous, and multiparous women)   Note. V = Cramers’ V. Participants and Procedure A convenience sample of non-pregnant women (n = 197) and pregnant women (n = 292) participated in the cross-sectional study. Non-pregnant women completed questionnaires online and were recruited by the snowball technique via personal contacts and social media posts. The main inclusion criteria were (1) age between 18 and 35 and (2) not being pregnant at the moment or ever before. The sample of pregnant women was recruited at the prenatal clinic of the University Hospital Centre while waiting for the regular prenatal check-up, where they filled out the questionnaires with pen-and-pencil. Of the pregnant women, 168 (57.5%) were nulliparous and 124 (42.5%) were multiparous. Both groups were, on average, at 33 weeks of pregnancy. A complete description of the subgroups is presented in Table 1. Most women were highly educated (or educating), were of average socioeconomic status, and lived in urban places. However, non-pregnant women were on average 5 to 8 years younger than pregnant women, most of whom were students. In contrast, pregnant women were mostly married or cohabiting and were mainly employed. The study was approved by the Ethics Committee of the Catholic University of Croatia and by the Ethics Committee of the University Hospital Centre Sisters of Mercy, where the study on pregnant women took place. Pregnant women signed the informed consent before completing the questionnaires. In contrast, e non-pregnant women read the informed consent and gave their consent by clicking the “Next” button as a prerequisite for entering the online study. Data were collected from April to June 2017. Instruments Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ, A-version; Wijma et al., 1998) The W-DEQ-A measures fear of childbirth and has two versions: version A – expectations before birth – and version B – experiences after birth. We used version A which was previously translated and validated into Croatian (Žigi et al., 2012). It consists of 33 items originally; however, the last two items regarding thoughts about death and harming the baby were removed for ethical reasons. Participants responded on a scale from 0 (not at all) to 5 (extremely), where opposite feelings and thoughts were presented. A total score was obtained by summing all items after reversing some items. A higher result indicates higher fear of childbirth. Results could range from 0 to 155, but clinically significant score was equal to 85 or above (Ryding et al., 1998). In this study, Cronbach α was .92, so internal consistency was high. Positive and Negative Perfectionism Scale (PNPS; Terry-Short et al., 1995) The PNPS is a 40-item questionnaire that measures positive (18 items; e.g., “My successes spur me on to great achievements.”) and negative perfectionism (22 items; e.g., “I feel guilty or ashamed if I do less than perfectly.”). The questionnaire was previously translated into Croatian and showed good psychometric properties (Lauri Korajlija, 2004). Answers were rated on a scale from 1 (strongly disagree) to 5 (strongly agree), and the total score was calculated by summing the corresponding items. The higher result indicates higher positive or negative perfectionism. In this study, Cronbach α was .87 for positive and .89 for negative perfectionism. Intolerance of Uncertainty Scale (IUS; Freeston et al., 1994) The IUS is an 11-item scale that measures intolerance to uncertainty. It was previously translated and validated into Croatian language (Mami, 2016). Responses were rated on a scale from 1 (not at all characteristics of me) to 5 (entirely characteristic of me). The scale consists of two subscales: prospective and inhibitory anxiety, but we obtained a one-factor solution and used only the total score. An example item is: “When it’s time to act, uncertainty paralyses me.”. The total score was calculated by summing all items, so the theoretical range is from 1 to 55. A higher result indicates higher intolerance of uncertainty. In this study, Cronbach α was .92. The general datasheet for pregnant and non-pregnant women comprised questions on age, marital status, education level, employment, socioeconomic status, and place of living. Also, preparedness for childbirth was estimated with the same question, “How prepared do you feel for childbirth?”, with a 5-point rating scale (1 = not at all, 5 = completely) in all three groups. In addition, non-pregnant women were asked about the pregnancy plans (e.g., “I do not plan pregnancy”; “I want pregnancy but not in the next year”; “I would like to become pregnant as soon as possible”; “I am pregnant”). Those responding with the option “I am pregnant” were excluded from the sample. On the other hand, pregnant women were asked about the gestational week, parity, and the type of previous delivery for multiparous women (vaginal delivery, instrumental vaginal delivery, planned caesarean section, and emergency caesarean section). Statistical Analysis Before conducting the research, power analysis was performed in order to estimate the number of participant and G-Power 3.1.9.2 software was used. It was calculated that the minimum number of participants for each group should be 74. Descriptive data, correlational analysis, and multiple regression analysis were conducted in software SPSS 21.0 for Windows. Three regression analyses were conducted for each group: non-pregnant women, nulliparous, and multiparous women. Dependent variable in regression analysis was FOC, while predictors were positive perfectionism, negative perfectionism, intolerance of uncertainty, preparedness for childbirth, and type of delivery for multiparous women. Results were estimated with 95% of confidence, and confidence interval for B regression coefficients were showed. The chi-square and Cramer’s V, that estimates strenght of association between rows and columns, was estimated using the online calculator VassarStats 2023. Among non-pregnant women, one in five (20.3%) had clinically significant FOC, while the prevalence in nulliparous and multiparous pregnant women was 15.5% and 7.3%, retrospectively. The statistically lowest prevalence of FOC was in sample of multiparous women compared with non-pregnant, χ2(1) =10.01, p < .05; Cramer’s V = .177, and nulliparous, χ2(1) =4.57, p < .05; Cramer’s V = .125. However, there was no difference in FOC prevalence between non-pregnant and nulliparous pregnant women, χ2(1) =1.43, p > .05; Cramer’s V = .063). Next, associations between the FOC levels and psychological variables were examined (Table 2). Across all groups, higher FOC was significantly correlated with lower preparedness for childbirth. In the sample of non-pregnant and first-time pregnant women, higher FOC was weakly but significantly correlated with lower levels of positive perfectionism and higher levels of negative perfectionism and intolerance of uncertainty. However, in multiparous pregnant women, these correlations were non-significant. Additionally, in multiparous women, the correlation between FOC and the mode of previous delivery was examined. Multiparous pregnant women who had emergency caesarean section in previous pregnancy had significant higher FOC (r = .24, p = .007). However, there was no correlation between FOC and planned caesarean section (r = .00, p = .998) or instrumental vaginal (r = -.08, p = .364). Separate multiple regression analyses were conducted for all three sub-groups to examine predictors of FOC (Table 3). In non-pregnant women, significant predictors of high levels of FOC were lower positive perfectionism, higher negative perfectionism, intolerance of uncertainty, and lower preparedness for childbirth. These predictors explained 25% of FOC variance in non-pregnant women. In nulliparous pregnant women, significant predictors of higher levels of FOC were lower positive perfectionism, higher negative perfectionism, and lower preparedness for childbirth, but not intolerance of uncertainty. Predictors explained 43% of the variance in nulliparous pregnant women. Finally, in multiparous women, significant predictors of higher levels of FOC were low preparedness for childbirth and having an experience of emergency caesarean section in a previous pregnancy, explaining 23% of the variance. Additionally, it is important to mention that low preparedness for childbirth was the strongest predictor of higher levels of FOC across all groups. Table 3 Multiple Regression Analysis Predicting Fear of Childbirth for All Groups   Note. c. s. = caesarean section; LB = lower bound of 95% confidence interval for B; UB = upper bound of 95% confidence interval for B. *p < .05, **p < .01. The results of this study showed the prevalence of clinical levels of FOC was highest in the sample of non-pregnant women and nulliparous pregnant women compared with multiparous pregnant women. When examining correlates of higher FOC, the essential variable across sub-groups was low preparedness for childbirth. In non-pregnant and nulliparous pregnant women, personality traits had a more prominent role for FOC, while previous delivery experience, specifically an emergency caesarean section, was crucial in multiparous women. The prevalence of FOC in non-pregnant women (20%) was similar to the prevalence in nulliparous women (15%), while a significantly lower prevalence was found in multiparous women (7%). Our results were in line with previous findings about the higher prevalence of FOC in nulliparous women compared with multiparous (Jokić-Begić et al., 2014; Størksen et al., 2013). Moreover, women who were still not pregnant had a somewhat lower prevalence (20%) prevalence than previously established in Croatian female students (26%) (Žigi Anti et al., 2019). This slight difference may come from the fact that in the latter study, only students participated. In contrast, in the current study, 58% of the non-pregnant sample were students and was somewhat older. Therefore, it seems that the younger the women, the more prevalent the FOC. According to a meta-analysis, the prevalence of FOC in nine European countries (including Croatia), the USA, Canada, and Australia was between 6 and 15% (Nilsson et al., 2018). However, a systematic review from O’Connell et al. (2017) showed an even wider prevalence range across countries, i.e., 4% to 43%. These results suggest that there are cultural differences in experiences of childbirth (Nilsson et al., 2012), which is not surprising due to the various perinatal care in different countries. However, differences may also be due to the differences in the samples included, with lower prevalence if more multiparous women are involved. Results suggest that perfectionism was significantly associated with FOC in non-pregnant and nulliparous pregnant women. More specifically, higher levels of FOC were correlated with lower positive and higher negative perfectionism. These findings align with the study conducted with Croatian pregnant women showing that adaptive perfectionism was associated with lower FOC, while non-adaptive perfectionism was associated with higher FOC (Ercegovac, 2013). It seems that in first-time pregnant women, adaptive perfectionism was a protective factor for FOC. Intolerance of uncertainty was a significant predictor of FOC in non-pregnant women only. To the best of our knowledge, the relationship between intolerance of uncertainty and FOC in non-pregnant women has not been examined yet, so the results could not be compared. However, intolerance of uncertainty was a predictor of FOC, along with pain catastrophising, in pregnant women in Sweden (Rondung et al., 2018). This is not in line with our results because intolerance of uncertainty was no predictor of FOC in neither nulliparous nor multiparous pregnant women. Further studies are needed to examine the relationship between intolerance of uncertainty and FOC, with possible mediators of that relationship. It is especially worthy of looking into intolerance of uncertainty, knowing that was related to anxiety, depression (McEvoy & Mahoney, 2012), and anxiety sensitivity (Carleton et al., 2007) that can lead to negative consequences on well-being. Among multiparous women, previous childbirth experience was a significant correlate of FOC. More detailed, women who previously had emergency caesarean section had higher FOC in the subsequent pregnancy. This result was in line with previous studies suggesting that previous negative experiences imposed higher fear of upcoming childbirth (Jokić-Begić et al., 2014; Størksen et al., 2015). Additionally, some findings indicated that for future FOC, previous obstetric complications and negative experiences during childbirth were important (Nilsson et al., 2012; Størksen et al., 2013). However, overall negative experiences had a more considerable impact on FOC than obstetric complications (Størksen et al., 2013). Qualitative studies showed that multiparous women with high FOC reported a lack of support, pain, and negative experiences with staff during the previous childbirth(s) (Nilsson et al., 2010; Nilsson & Lundgren, 2009). Such adverse experiences were very vivid in women’s memory, diminishing their ability to give birth (Nilsson et al., 2010). However, one more possible explanation is that women who experience more FOC during the pregnancy may experience more complications during childbirth that could lead to negative and even traumatic experiences (Wijma et al., 2002). Perceived preparedness for childbirth was a significant predictor of lower FOC across all groups. This result highlights the importance of preventive treatments that prepare women for delivery. This goes in line with some previous findings showing that psychoeducation about childbirth increases maternal preparedness for childbirth (Salmela-Aro et al., 2011), but psychological interventions are even more important. For example, an intervention that combined psychoeducation and cognitive therapy had better results in reducing childbirth-related anxiety than psychoeducation only (Saisto et al., 2001). Also, counselling and group interventions could decrease FOC (Toivanen et al., 2018; Waldenström et al., 2006). Despite the scientific contribution of this paper, some limitations should be considered. First, this study was cross-sectional correlational, so causal conclusions could not be made. Future studies should have a longitudinal design and follow participants from a period when they do not think about pregnancy to the time when they are pregnant and after childbirth. The second limitation is the homogeneity of the sample. Most of the non-pregnant women were students, so they could differ from the general population of emerging/young adults (e.g., they can be more educated and have more information about pregnancy and childbirth). Also, pregnant women were highly educated, employed, living in an urban region, and with perceived average socioeconomic status. Third, the cut-off score on the W-DEQ questionnaire was not validated in the Croatian sample using a clinical interview. Mentioned cultural differences may impact the cut-off score. Additionally, further studies should examine other constructs related to FOC. It would be beneficial to explore a relationship with a partner and social support. Particular attention should be focused on detecting predictors of FOC in women who are not pregnant, especially those who do not want to be pregnant because of the FOC. It could be that some personality traits, but also negative experiences from other women (especially significant ones) are related to FOC. In conclusion, the results of this study imply that predictors of FOC are personality traits in non-pregnant and nulliparous women, in contrast to previous negative childbirth experiences (having emergency caesarean section) in multiparous. Thus, the current study extends the conclusions of the previous research by Jokić-Begić et al. (2014), showing that non-pregnant women share similar mechanisms as pregnant nulliparous women – where in both groups personality traits prevail. However, perceived preparedness for childbirth was important for diminishing FOC in all groups of women, which provides strong support for preventive interventions regarding FOC. First, it is necessary to identify all women at risk for high FOC – those who are still not pregnant and pregnant. Examining childbirth experiences in perinatal settings is recommended (Martínez-Borba et al., 2022). For young women who are still not pregnant preventive programs should be focus on psychoeducation in high school and from reliable sources (e.g., practitioners, gynaecologists, etc.) (Stoll et al., 2014; Žigi Anti et al., 2019). Special attention should be given to non-pregnant women with severe FOC that is preventing them to become pregnant. They feel abandoned by the system and left to struggle alone trying to educate themselves while constantly negotiating with themselves about pregnancy decision (Rondung et al., 2020). Pregnant women should also be well informed about childbirth. Preventive programs should aim to restructure negative and maladaptive cognitions, diminish catastrophising, and use relaxation techniques. However, particular focus should be on multiparous women who have previously experienced negative experiences during childbirth, had an emergency caesarean section or obstetric complications. To sum up, programs regarding psychoeducation, counselling and psychotherapy should be implemented to diminish FOC in non-pregnant and pregnant women. Finally, programs should help participants to face their fear, feel empowered, and heighten their sense of security (O’Connell et al., 2021). Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Kuljanac, A., Brekalo, M., & Naki Radoš, S. (2023). Perfectionism, intolerance of uncertainty, and fear of childbirth in pregnant and non-pregnant women. Clínica y Salud, 34(2), 65-70. https://doi.org/10.5093/clysa2023a17 References |
Cite this article as: Kuljanac, A., Brekalo, M., & Radoš, S. N. (2023). Perfectionism, Intolerance of Uncertainty, and Fear of Childbirth in Pregnant and Non-pregnant Women. ClĂnica y Salud, 34(2), 65 - 70. https://doi.org/10.5093/clysa2023a17
Correspondence: snrados@unicath.hr (S. Naki Radoš).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







