
Group Acceptance and Commitment Therapy (ACT) for Fibromyalgia Patients
[AceptaciĂłn grupal y terapia de aceptaciĂłn y compromiso con pacientes de fibromialgia]
Carmen Ramos1, Francisca López Ríos2, Gonzalo Peña Muñante1, and Jorge Ordóñez-Carrasco3
1Grade, AsociaciĂłn de Fibromialgia, AlmerĂa, Spain; 2Universidad de AlmerĂa, Spain; 3Universidad de Zaragoza, Spain
https://doi.org/10.5093/clysa2024a1
Received 20 March 2023, Accepted 22 September 2023
Abstract
Background: Previous studies have shown that catastrophizing and avoiding pain increase suffering and disability of patients with fibromyalgia (FM). Acceptance and Commitment Therapy (ACT) has demonstrated good results in the treatment of chronic pain. Method: This study applies a group ACT therapy for women with fibromyalgia, focusing on therapeutic components, such as acceptance, defusion, and personal values. An experimental design with control group was used; 57 women diagnosed with FM participated in this study (25 in the ACT group and 32 in the control group). The ACT group received five intervention sessions. Psychological symptoms, perceived health, mindfulness, catastrophic thinking, and cognitive fusion were evaluated at pre- and post-treatment and at six-month follow-up. Results: The results showed that the ACT group had significantly better results in mental health, social role and functioning, anxiety, depression, somatization, and obsession-compulsion, less catastrophic thinking, and improved capacity for mindfulness at six-month follow-up. Conclusions: The results are discussed in the light of previous interventions.
Resumen
Antecedentes: Estudios anteriores han demostrado que los pensamientos catastróficos y evitar el dolor aumentan el sufrimiento y la discapacidad de los pacientes con fibromialgia (FM). La terapia de aceptación y compromiso (ACT) ha tenido buenos resultados en el tratamiento del dolor crónico. Método: Este estudio aplica una terapia ACT grupal a mujeres con fibromialgia, centrándose en componentes terapéuticos, como la aceptación, la defusión y los valores personales. Se ha utilizado un diseño experimental con grupo control, participando 57 mujeres diagnosticadas de FM (25 en el grupo ACT y 32 en el grupo control). El grupo ACT recibió cinco sesiones de intervención. Se evaluaron los síntomas psicológicos, la salud percibida, la atención plena, el pensamiento catastrófico y la fusión cognitiva antes y después del tratamiento y a los seis meses de seguimiento. Resultados: Los resultados del grupo de ACT son significativamente mejores en salud mental, rol y funcionamiento social, ansiedad, depresión, somatización y obsesión-compulsión, pensamiento menos catastrófico y mejor capacidad de atención plena en el seguimiento a seis meses. Conclusiones: Estos resultados se abordan teniendo en cuenta los de intervenciones anteriores.
Palabras clave
Fibromialgia, Terapia de aceptaciĂłn y compromiso, Catastrofismo, AtenciĂłn plenaKeywords
Fibromyalgia, Acceptance and commitment therapy, Catastrophism, MindfulnessCite this article as: Ramos, C., Ríos, F. L., Muñante, G. P., & Ordóñez-Carrasco, J. (2024). Group Acceptance and Commitment Therapy (ACT) for Fibromyalgia Patients. ClĂnica y Salud, 35(2), 39 - 48. https://doi.org/10.5093/clysa2024a1
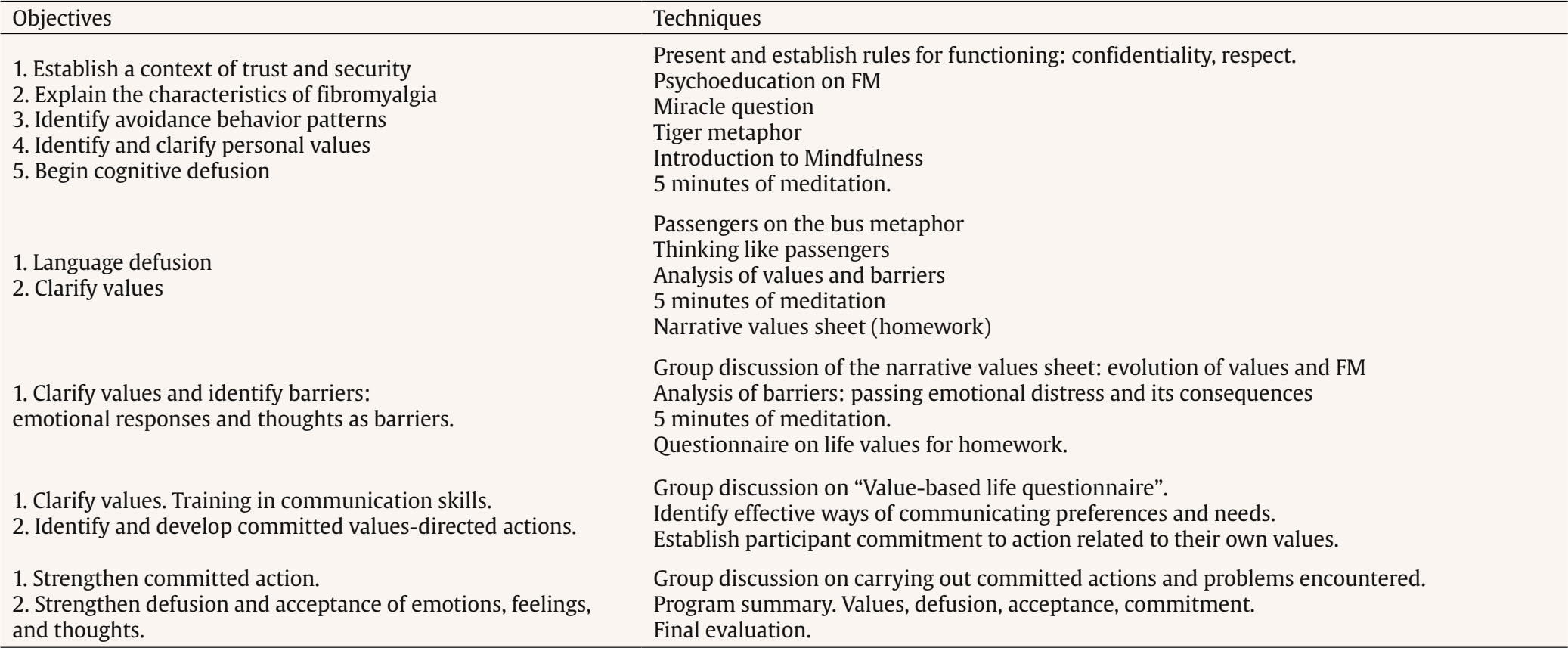
Correspondence: flrios@ual.es (F. López Ríos).Fibromyalgia (FM) is a syndrome characterized mainly by the presence of pain at several different points in the four body quadrants (trigger points), although there is no tissue damage or inflammation (Bennett, 2009). Other problems that increase pain and disability are hypersensitivity to sound and sensitivity to touch or pressure, odor and light, sleep problems, irritable bowel syndrome (IBS), chronic fatigue syndrome (CFS), bladder problems, numbness and paresthesia, slowed thinking, and “brain fog”, also called fibro-fog. Other reported problems are loss of appetite, dizziness, and falling, in addition to anxiety and depressive symptoms. The average prevalence worldwide is 2.1%, with 4.3% in women and 0.95% in men (Cabo-Messeguer et al., 2017). The origin of the fibromyalgia syndrome is unknown. Different etiological hypotheses have been proposed, although currently studies suggest a central nervous system dysfunction that debuts in viral infections, traumatisms, or periods of intense stress. There is no test for its diagnosis, and medical practitioners differ in their opinions of its psychosomatic origin or how severely disabling can become. In view of the heterogenous symptoms of fibromyalgia, there is a consensus on the advisability of multidisciplinary approaches, combining medical treatment with other physiotherapeutic and psychological approaches (Spaeth & Briley, 2009). Medical treatment for fibromyalgia includes pain relievers, anxiolytics, and antidepressants (García et al., 2016). Psychological intervention is directed mainly at adapting to the conditions imposed by the disease, reducing anxiety and depressive symptoms, and reinforcing adherence to treatment. The most common psychological approaches for fibromyalgia patients focus on techniques such as psychoeducation and progressive muscle relaxation (Sim & Adams, 2002). Hypnosis with specific analgesic suggestions has been used to lessen associated pain with positive results (Castel et al., 2007). Other results suggest that hypnosis strengthens the effects of intervention with cognitive-behavioral therapy (CBT) (Martínez-Valero et al., 2008). The psychological intervention most widely used, as in other areas, is CBT with such components as psychoeducation, achieving coping skills through cognitive restructuring of beliefs, training in social skills and problem-solving, scheduling daily leisure activities and physical exercise, and strategies for maintaining achievements and preventing relapse into disabling thoughts, inactivity, and isolation. In the nineties, several studies had already demonstrated that CBT significantly improved pain (Keel et al., 1998) and variables such as depression (Nicassio et al., 1999) and self-efficacy (Gowans et al., 1999). Along this line, Lera et al. (2009) compared multidisciplinary intervention programs for reducing fibromyalgia symptoms (with and without CBT). The results showed that CBT strengthened the effects of the multicomponent program, lowering scores on the Fibromyalgia Impact Questionnaire (FIQ) and increasing functionality, especially in patients with chronic fatigue. In a meta-analysis of psychological intervention for FM, Glombiewski et al. (2010) found significantly more short-term improvement with CBT than with other techniques, although with a relatively small effect size. Intervention with mindfulness has been widely studied in health problems with pain with positive results on quality of life and participant pain (Lauche et al., 2013). A clinical trial by Van Gordon et al. (2017) compared a second-generation mindfulness-based intervention (more focused on spirituality and detachment) with a cognitive-behavioral intervention, finding superior sustained effects on fibromyalgia symptoms with the second-generation mindfulness-based intervention. The development of third generation behavioral therapies (Hayes, 2004), especially acceptance and commitment therapy (ACT) (Hayes, et al. 2012), focuses therapeutic objectives on processes leading to psychological flexibility as the health model. The components of ACT are acceptance of private experiences (e.g., pain), language defusion, concentration on the present moment, the self as context, and committed action in the direction of personal values. Its goal is to enable people to direct their behavior toward what is of value in their life, identifying psychological barriers, such as fusion, avoidance, or impulsive and/or disoriented behavior. ACT has been widely applied to chronic pain and has been recognized as one of the therapies with empirical validity in this field (Du et al., 2020; Hans & McCraken, 2014; Yu et al., 2022), where acceptance seems to be one of the key elements in pain, anxiety, depression, and physical and vocational functioning (Baranoff, et al., 2016; Du et al., 2021; Vowles & McCraken, 2008). ACT intervention focuses on identifying strategies avoiding private experiences (pain, despondency, thoughts, emotional responses, and so on) and through experiential exercises and mtaphors assists the patient in realizing that control strategies used to weaken pain are actually part of the problem, not the solution. From there on, unfolding therapeutic procedures enable language defusion, that is, thoughts and feelings (especially catastrophic thinking) are recognized as such, and not as truths to be adhered to, or as dictating action. Personal values are a guide in the direction of change, so that within their pain and suffering a person’s life can still make sense (Hayes et al., 2012). Studies have also been done on application of ACT to FM patients. For example, Simister et al. (2018) did a study of the change that occurs when a person enrolls in values-related activities and their effect on pain and disability. They found that the changes in ACT processes (defusion, acceptance, and values) correlated with less intense pain, less emotional stress, and less disability. The clinical trial by Vowles et al. (2008) analyzed result and process variables in an ACT and mindfulness group intervention program. The results showed a medium-to-large effect size in the result variables, as well as the empowering effect of acceptance and action in the direction of values, without thinking about the pain itself. The controlled trial by Luciano et al. (2014) also showed improvements in the ACT group over recommended medication and the waiting list group. Summarizing, while the many psychological interventions for fibromyalgia patients have had varied results, application of ACT and mindfulness is providing promising results in quality of life and functionality. In view of the above, the objective of this study was to test the effects of applying a short ACT group treatment to women with FM directed at reducing cognitive fusion and catastrophizing pain, improving functionality and psychological wellbeing and decreasing affectation of the illness in a trial with a control group. The study hypothesis was that intervention with ACT would facilitate change in avoidance processes and cognitive fusion and would improve patients’ general functionality and psychological wellbeing. Study Design This study used a pre-post-treatment experimental design with a waiting-list control group. Participants The sample consisted of 57 women with FM who were members of the Asociación de Fibromialgia de Almería [Almeria Fibromyalgia Association]. They were randomly divided into two groups: intervention group (IG), n = 32, and; control group (CG), n = 25. All the participants completed pre-, post-treatment and follow-up evaluation questionnaires. Participants were distributed into IG and CG groups by drawing at random from among those who had completed the questionnaires and given their consent to the intervention. In the IG, seven participants completed the original questionnaires, but did not take part in the treatment stage for various personal problems. The CG received treatment after the six-month follow-up. The mean participant age was 52 in a range of 30 to 66 years. Forty of the participants were married (70.2%), ten of them divorced (17.5%), five single (8.8%), and two were widowed (3.5%). Of the total sample, 41.1% had a primary school education, 31.6% secondary school, and 26.3% had a university education. Sixteen of the women (28.1%) were employed but on leave of absence, 13 (22.8%) were actively employed, 12 (21.1%) were unemployed, 11 (19.3%) were housewives, and five (8.8%) were retired. Measures The participants filled in a brief questionnaire for demographic data and a battery of self-report measures. Psychopathological symptoms were evaluated using the Spanish version of the Symptom Assessment-45 Questionnaire (SA-45; Davison et al., 1997) by Sandín et al. (2008). This self-report instrument on psychopathological symptoms has 45 items derived from the SCL-90. It consists of nine five-item scales, which evaluate the same dimensions as the SCL-90. Each item is answered on a five-point scale (0 to 4) and scores may be calculated by symptom frequency, overall severity index or for each of the following nine subscales: hostility, somatization, depression, obsession/compulsion, anxiety, interpersonal sensitivity, phobic anxiety, paranoid ideation, and psychoticism. The authors of the Spanish adaptation found a high reliability coefficient with a Cronbach’s alpha of about .95 (Sandín et al., 2008). Catastrophic thinking was evaluated with the Pain Catastrophizing Scale (PCS; Sullivan et al., 1995). This13-item self-report rates pain on a Likert-type Scale of 0 to 4. The total score shows how much the patient catastrophizes pain. It has three dimensions: a) rumination (constant worry and inability to inhibit thinking about pain), b) magnification (exaggeration of unpleasantness of painful experiences and expectations for negative consequences), and c) helplessness (inability to face painful experiences). High scores show a higher level of catastrophizing. Internal consistency of the Spanish version of the scale scores was .79 and test-retest reliability was .84 (García-Campayo et al., 2008). Mindfulness was evaluated with the Spanish version of the Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2003). This self-report provides a single score evaluating an individual’s ability to pay attention to and be aware of what is taking place in the present moment in daily life. Its 15 items are scored on a Likert-type scale ranging from 2 (almost always) to 6 (almost never). The Spanish validation showed good results with a Cronbach’s alpha of .89 and a total variance of 42.8% with the unidimensional structure, similar to the original scale (Soler et al., 2012). Cognitive fusion, that is, the extent of a person’s psychological involvement with the shape and content of thoughts, was evaluated using the Spanish version of the Cognitive Fusion Questionnaire (CFQ; Gillanders et al., 2014) by Romero-Moreno et al. (2014). This scale has seven items with answer choices on a seven-point Likert-type scale from 1 (never) to 7 (always). The final score was calculated as the sum of all the elements, where higher scores show stronger fusion with the content of cognitive events. In the original study, the CFQ showed good internal consistency in five different samples, with Cronbach alphas of .88 to .93 (Gillanders et al., 2014). Cuestionario de Salud (Health Survey Questionnaire, SF-36; Jenkinson et al., 1993) was used to measure perceived health in the previous four weeks. The instrument consists of 36 items with a Likert-type answer format, which is transformed into a score of 0 (worse quality of life) to 100 (better quality of life). It is comprised of eight dimensions: physical functioning, social functioning, role-physical, role-emotional, mental health, vitality, pain, and general health perceptions. The validity of this scale has been demonstrated in previous studies with a Cronbach’s alpha coefficient > .70 in all of its dimensions (Alonso et al., 1995). Procedure First, we contacted the Almeria Fibromyalgia Association (AFIAL) and informed them of the characteristics of the intervention program at an introductory meeting. Inclusion criteria were: women diagnosed with fibromyalgia according to the American College of Rheumatology (Wolfe et al., 1990), speaking and understanding Spanish, being of legal age, not under any psychological treatment, and agreeing to participate by signing the informed consent form. The 66 women who were interested, met the inclusion criteria, and agreed to participate in the study were distributed into two randomized groups, 25 in an intervention group (IG) and 32 in a control group (CG). Both the participants in the IG and CG were evaluated with the same instruments before and after the intervention program with a follow-up at six months from the end of intervention. None of the intervention program components were applied in the CG. After the six-month follow-up, the GC received the ACT treatment. All the program of treatment was applied from an Almeria Fibromyalgia Association psychologist specialized in ACT assisted by a Master’s student. This study was approved by the Fibromyalgia Association Ethics Committee and the University of Almeria. The intervention was applied in a group ACT treatment program in five weekly two-hour sessions. The therapeutic objectives of the sessions focused on psychological acceptance and cognitive defusion, values and the behaviors involved in those values. The treatment was applied in the IG divided into three smaller groups of eight, eight and nine participants. Table 1 shows the order of the sessions and the techniques used. Data Analysis A repeated measures general linear model (GLM) was implemented to evaluate the intervention’s impact on the variables studied throughout the trials (pre-intervention, post-intervention, six-month follow-up) and for between-group comparison (intervention group vs. control group). Pillai’s trace, a multivariate test statistic, was used to describe the overall effects of the variables analyzed. Partial eta-squared effect sizes (ηp2) were also reported as an indicator of effect size (.02 was considered small, .13 medium, and .26 large). Post-hoc multiple comparison tests were performed to determine differences between means (p ≤ .05). The Bonferroni test was used to adjust the level of significance observed in the multiple comparisons. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (SPSS 26.0, SPSS Inc., Chicago, USA). Table 2 Participant Sociodemographic Characteristics  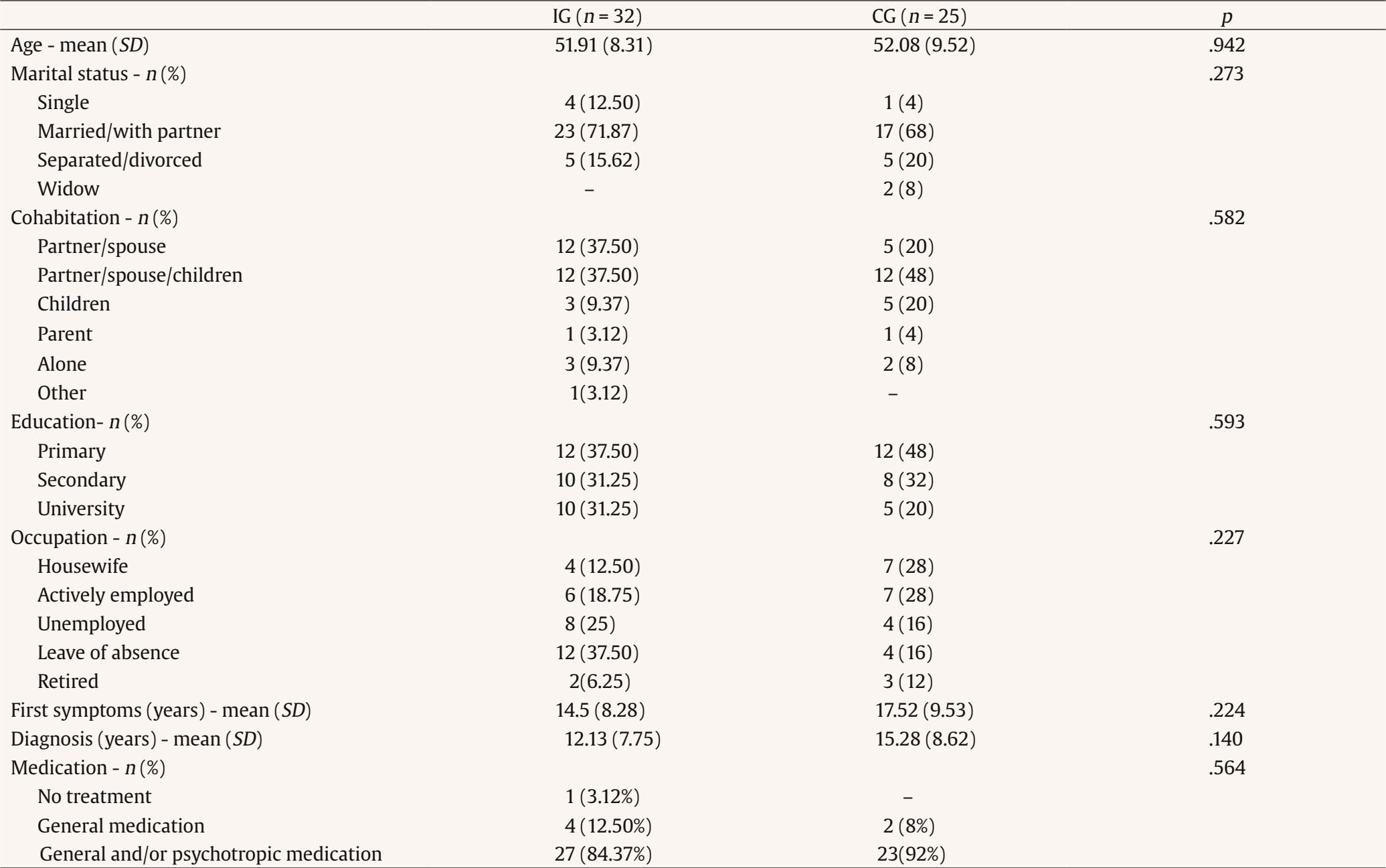 Note. IG = Acceptance and commitment therapy group; GC = control group. Data are shown as means (standard deviation) or n (%). The sociodemographic characteristics of the participants in the IG and the CG are shown in Table 2, where statistically significant differences between the sociodemographic variables in the two groups may be observed. As no between-group differences were found in age, marital status, education, occupation, time since the appearance of the first symptoms, or type of medical treatment prescribed, the two groups of participants were homogeneous with respect to those variables. The effect of treatment was analyzed by comparing the IG and CG means on the various scales of the evaluation instruments used, both in pretreatment and posttreatment and at the six-month follow-up. The results (means, standard deviations, significance, and Cohen’s d effect size) are shown in Table 3. Statistically significant between-group differences were found in the means of the SF-36 Health Survey Questionnaire at posttreatment and at the six-month follow-up in the role-emotional, mental health, and social functioning subscales, while the pain, vitality, role-physical, and physical functioning subscales had statistically significant means only at the six-month follow-up. In all cases the differences in means had effect sizes (Cohen’s d) over 0.5. Table 3 Comparison of Means of the Variables in the Two Groups at the Three Measurement Times (continued)  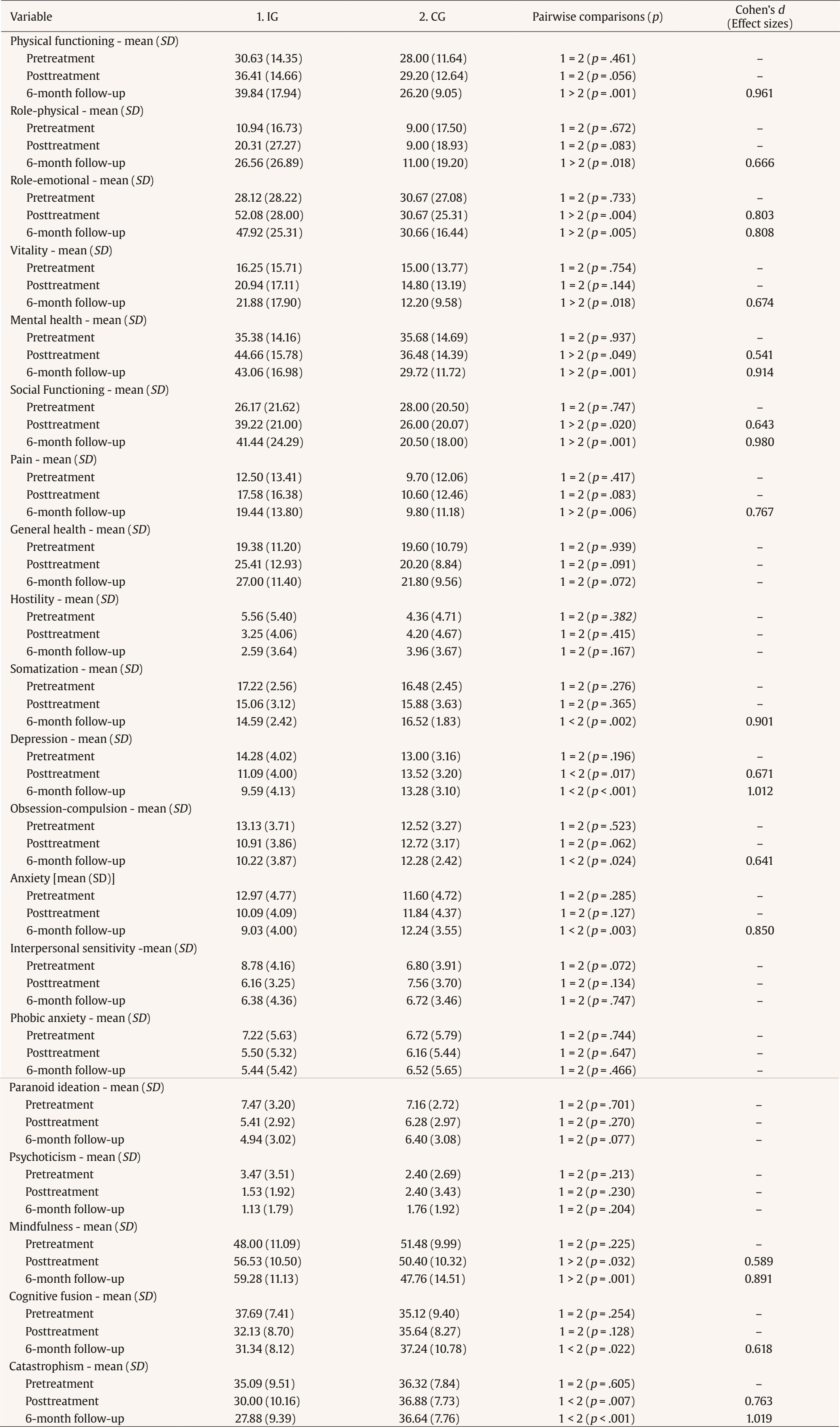 Note. IG = Acceptance and commitment therapy group; GC = control group. Data are shown as means (standard deviation) or n (%) The results of the SA-45 Symptom Assessment-45 Questionnaire showed statistically significant differences in means on depression both at posttreatment and at the six-month follow-up. The between-group differences on somatization, obsession-compulsion, and anxiety scales were significant at the six-month follow-up. In all cases, IG scores were lower than CG scores. There were no differences at the end of treatment nor at the follow-up on psychoticism, paranoid ideation, phobic anxiety, nor interpersonal sensitivity subscales. The Mindful Attention Awareness Scale (MAAS) results showed statistically significant differences between IG and CG at both posttreatment and six-month follow-up with a large effect size of over 0.5 in both cases. The results for cognitive fusion (CFQ) were statistically significantly lower in IG than CG only at six-month follow-up. However, for catastrophizing, between-group differences were significantly lower at both post-treatment and at six-month follow-up. Effect sizes were variable as shown in Table 3, where the best were for the depression and somatization subscale and the Mindfulness Questionnaire. On the contrary, there were no statistically significant differences between any of the study variables in CG. Table 4 presents the results of the intragroup comparison for IG and CG at pretreatment, posttreatment, and follow-up (six months). It may be observed that there were statistically significant improvements in the IG from pretreatment to posttreatment and from posttreatment to follow-up on the SF-36 Health Survey Questionnaire physical functioning, role-physical, role-emotional, mental health, social functioning, and general health subscales. On the vitality and pain subscales, differences between pretreatment and follow-up were statistically significant. The results show improvement in vitality and severe pain. However, in the CG, mental health fell significantly from pretreatment to follow-up and from posttreatment to follow-up. Table 4 Comparison of Means of Each Variable in the two Groups   Note. IG = aceptance and commitment therapy group; GC = control group. Data are shown as means (standard deviation) or n (%). Scores on the variables in the SA-45 dropped statistically significantly on hostility somatization, depression, obsession-compulsion, anxiety, interpersonal sensitivity, phobic anxiety, paranoid ideation, and psychoticism subscales. Furthermore, scores rose significantly in mindfulness, and were lower in catastrophizing and in cognitive fusion between pretreatment and follow-up. Our findings showed significant changes in the IG in the variables evaluated. Improvements were found in perception of health and functionality, and psychopathological symptoms decreased. Mindfulness improved, cognitive fusion decreased, and catastrophizing was lessened, showing that treatment with ACT is useful for fibromyalgia patients. Another positive result was the stability of the changes which were still maintained at the six-month follow-up. The effect sizes varied, but were large in general. In the CG, mental health worsened, which could be related to the time that passed without specific psychological intervention and problems involved with fibromyalgia. The SF-36 subscales include functionality in such vital areas as pain and vitality. In this case, there were significant differences between pretreatment and follow-up in vitality, pain, and anxiety. These long-term outcomes show incubation of the effects of ACT application previously found in other studies (González-Menéndez et al. 2014), consistent with advances or improvements in the patient scores observed at follow-up or that increased during it. This result could be indicating increased general functionality in their lives, although their health indicators remained similar. It should be emphasized that mental health and social functioning variables showed significant differences at the end of treatment and at follow-up. That is, even though patient health did not change after the treatment period, their emotional state and social relations did. These results are in line with ACT goals of promoting a meaningful life in spite of adverse health conditions. The different SA-45 subscale results showed changes in the variables related to affective problems (somatization, obsession-compulsion, depression, and anxiety), which are the most prevalent in the FM population, and strong presence of private events (emotional experiences) that tend to be avoided. Therefore, intervention for psychological acceptance could be especially useful. There were no changes in other variables, such as hostility, phobic anxiety, interpersonal sensitivity, paranoid ideation, or psychoticism. This could be interpreted as previous scores not having been clinically significant and, moreover, neither the duration of the intervention nor its objectives were directed at these variables. Therefore, the results are positive, especially in view of the fact that the therapeutic objective of ACT is not to decrease pain or any other symptom, but for the person to live a valuable life. These results are in agreement with those found by Luciano et al. (2014), who compared ACT with Recommended Medication and Waiting List. Nevertheless, the use of different evaluation instruments prevents from an accurate comparison, except for “catastrophizing”, for which the effect size was higher in our study at six-month follow-up. In the analysis of specific components of the ACT protocol used, the introduction of mindfulness showed significant changes at posttreatment that were maintained with a large effect size at follow-up. Thus, the inclusion of mindfulness in intervention with ACT as one of the therapeutic components for facilitating acceptance and distancing from one’s thoughts can promote life functioning in spite of pain, as shown in previous studies, where acting with awareness and focusing attention on the present benefited functioning in chronic pain patients (McCracken & Thompson, 2009). One of the most important problems in patients with chronic pain is their catastrophic thinking, that is, proneness to ruminating, magnifying, and feeling defenseless against pain (Sullivan et al., 1995). Catastrophizing is fusion of thought related to feeling more pain, more emotional distress, and worse life adjustment (Severeijns et al., 2002). Practicing mindfulness in addition to other defusion/acceptance exercises (passengers on a bus metaphor) can weaken the tendency to catastrophize and facilitate acceptance of private experiences, such as catastrophic thoughts or pain. Thus, acceptance seems to be the mediating component of change in patients with chronic pain (Baranoff et al., 2016; Cederberg et al., 2016; Vowles et al, 2008; Yu et al., 2022). Another key ACT therapeutic component is personal values, that is, achieving patient behavior guided by what is important to them. Our protocol worked on each patient identifying relevant life directions and commitment to behaviors enabling progress in those directions. Previous studies have shown that acceptance and tolerance of pain increase noticeably when values are introduced in therapy (Branstetter-Rost et al., 2009). Among the limitations of this study, we should mention that the evaluation instruments used did not allow an accurate comparison with other studies. In addition, the CG had no therapeutic contact, which would have been necessary to isolate the effect of intervention with ACT. Furthermore, in order to evaluate the change in specific processes, it would have been advisable to introduce evaluation of acceptance and values. Therefore, future studies on the usefulness of group ACT for FM patients should consider these limitations, and also use designs comparing ACT with CBT to confirm the differences found between acceptance-based treatments and treatments for eliminating symptoms. Conclusion Group intervention with ACT, including acceptance, defusion, and action components directed at values, was useful in improving the social and physical functionality, diminishing affective symptoms and pain in fibromyalgia patients. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Lopez Rios, F., Ramos, C., Ordóñez, J., & Peña Muñante, G. (2023). Group acceptance and commitment therapy (ACT) for fibromyalgia patients. Clínica y Salud, 35(2), 39-48. https://doi.org/10.5093/clysa2024a1 References |
Cite this article as: Ramos, C., Ríos, F. L., Muñante, G. P., & Ordóñez-Carrasco, J. (2024). Group Acceptance and Commitment Therapy (ACT) for Fibromyalgia Patients. ClĂnica y Salud, 35(2), 39 - 48. https://doi.org/10.5093/clysa2024a1
Correspondence: flrios@ual.es (F. López Ríos).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







