
Certified Midwives and Nurse-Midwifes’ Knowledge and Attitudes about Peripartum Depression Management – The Effectiveness of a Peripartum Depression Management Training
[Los conocimientos sobre gestión de la depresión puerperal de las matronas y enfermeras obstetras acreditadas y su actitud – la eficacia de la formación en gestión de la depresión puerperal]
Magdalena Chrzan-Dętkoś, Natalia Murawska, and Marta Łockiewicz
University of Gdansk, Poland
https://doi.org/10.5093/clysa2024a12
Received 9 September 2023, Accepted 1 March 2024
Abstract
Background: In many countries, midwives and nurses play a vital role in supporting effective perinatal mental health (PMH) care, including peripartum depression (PPD) management. In our study, we aimed to evaluate the effectiveness of PMH training in increasing certified midwives (CMs) and certified nurse–midwives (CNMs)’ knowledge about PPD management in primary care settings. The training was a part of postpartum depression (PPD) prevention programme implemented by Polish Ministry of Health. Additionally, we investigated the link between the CMs and CNMs perception of systemic difficulties, attitudes toward work with patients with mental health problems, and the adherence to PPD screening procedures. Method: A total of 379 CMs and CNMs from primary health centres and hospitals who participated in a PPD management training completed the Test of Antenatal and Postpartum Depression Knowledge before and after PMH training and the REASON scale after the training. Results: Before the training, only 17% (n = 66) of CMs and CNMs considered themselves to be educated for PPD management. The participants’ knowledge about PPD significantly increased after the training, by three points on average. The effect size was very strong, d = 0.84. However, the prevalence of perinatal mental disorders and the suicide rate among persons with PPD remained misestimated. We also found that age had a substantial influence in controlling the relationship between perceived educational preparation for PPD management, job tenure, and actual knowledge about PPD management. Self-reported higher levels of perceived systemic problems in the workplace and having more negative attitudes toward working with persons experiencing emotional difficulties were associated with declared lower frequency of measuring the severity of PPD, using screening tools, counselling, and making referrals to specialists. Discussion: Even though the training turned out to be effective, a tendency to underestimate the negative consequences of PPD was observed. The participants’ perception of systemic problems and personal attitudes were associated with an adherence to PPD screening procedures. The implementation of an obligatory PPD screening may not be enough to change the everyday practice of CMs and CNMs. Further training, taking into account personal attitudes of health care professionals, and systemic changes are required to ensure an optimal management for persons with PPD.
Resumen
Antecedentes: En muchos países las comadronas y enfermeras juegan un papel fundamental con su ayuda a la asistencia eficaz a la salud mental perinatal (SMP), como por ejemplo la gestión de la depresión puerperal (DPP). En este estudio nos hemos propuesto analizar la eficacia del entrenamiento en SMP para aumentar los conocimientos de matronas acreditadas y enfermeras obstetras acreditadas en gestión de la DPP en el contexto de atención primaria. La formación era parte del programa de prevención de la depresión posparto que ha puesto en marcha el Ministerio de Sanidad Polaco. Además, investigamos el nexo entre la percepción de las matronas acreditadas y las enfermeras obstetras acreditadas de las dificultades sistémicas, las actitudes hacia el trabajo con pacientes con problemas de salud mental y el seguimiento de los procedimientos para descartar la DPP. Método: Un total de 379 matronas acreditadas y enfermeras obstetras acreditadas de centros de atención primaria y hospitales que habían participado en la formación en gestión de DPP cumplimentó la Prueba de Conocimientos de la Depresión Antenatal y Posparto antes y después de la formación en atención en salud mental perinatal y la escala REASON tras el entrenamiento. Resultados: Antes del entrenamiento solo un 17% (n = 66) de las matronas y enfermeras obstetras consideraban que hubieran sido formadas para gestionar la DPP. Los conocimientos de las participantes en DPP aumentaron significativamente un promedio de tres puntos porcentuales después del entrenamiento. El tamaño del efecto era muy elevado (d = 0.84), aunque seguía subestimándose la prevalencia de trastornos mentales perinatales y el índice de suicidio entre las personas con DPP. También observamos que la edad influía mucho en el control de la relación entre la percepción de la preparación educativa en gestión de DPP, la antigüedad en el empleo y el conocimiento real de la gestión de la DPP. El mayor nivel autoinformado de los problemas sistémicos percibidos en el puesto de trabajo y las actitudes más negativas hacia el trabajo con personas que experimentaban dificultades emocionales se asociaba con menor frecuencia declarada de medición de la gravedad de la DPP, de utilización de instrumentos diagnósticos y de orientación y derivación a especialistas. Conclusiones: Aunque el entrenamiento resultó ser eficaz, se observó una tendencia a subestimar las consecuencias negativas de la DPP. La percepción de los participantes de los problemas sistémicos y de las actitudes personales se asociaba con el seguimiento de los procedimientos de diagnóstico. Puede ser que la aplicación de un diagnóstico obligatorio de la DPP no sea suficiente para cambiar la práctica diaria de las matronas y enfermeras obstetras acreditadas. Se necesita más entrenamiento, teniendo en cuenta las actitudes personales de los profesionales de atención en salud mental y cambios sistemáticos para garantizar una gestión óptima del trabajo con personas que padecen DPP.
Palabras clave
Salud mental, DepresiĂłn puerperal, Matronas, GestiĂłn de la depresiĂłn puerperal, DiagnĂłsticoKeywords
Mental health, Peripartum depression, Midwives, Peripartum depression management, ScreeningCite this article as: Chrzan-Dętkoś, M., Murawska, N., & Łockiewicz, M. (2024). Certified Midwives and Nurse-Midwifes’ Knowledge and Attitudes about Peripartum Depression Management – The Effectiveness of a Peripartum Depression Management Training. ClĂnica y Salud, 35(2), 63 - 75. https://doi.org/10.5093/clysa2024a12
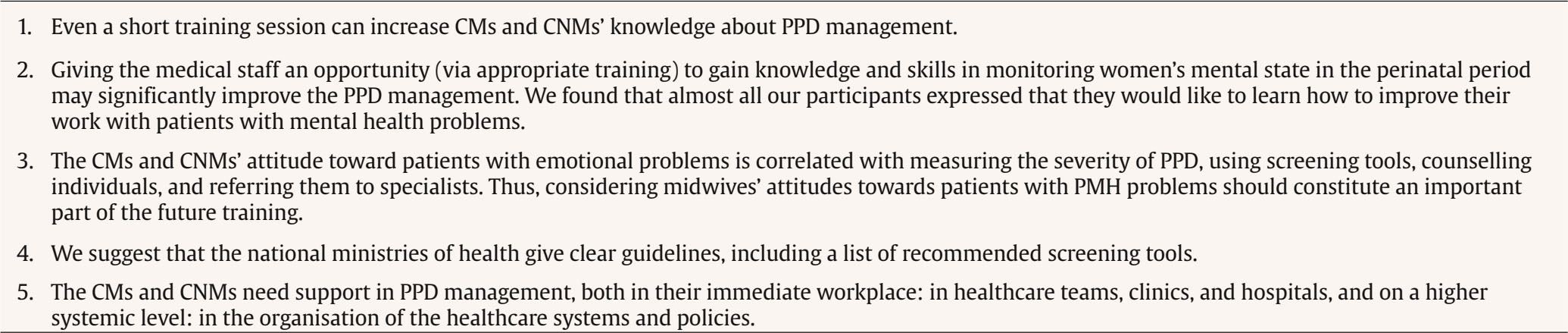
Correspondence: magdalena.chrzan-detkos@ug.edu.pl (M. Chrzan-Detkos).Certified midwives (CMs) and nurse midwives (CNMs) play a vital role in the peripartum primary care system in Poland, and possibly in other countries (as midwives are not part of care systems in all countries), as they have a low-threshold and non-stigmatizing access to their clients (Chrzan-DČ©tkoś & Walczak-Kozlowska, 2020; Bina et al., 2019; Gong et al., 2020; Kurtcu & Golbasi, 2014). They support parents, identify a peripartum distress/peripartum depression (PPD) risk, and make referrals to specialist services. The perinatal women are, in general, satisfied when CMs and CNMs have a more active role in screening for PPD symptoms and risk (Chrzan-DČ©tkoś & Walczak-Kozlowska, 2021). On the other hand, the lack of CMs and CNMs’ sufficient knowledge about perinatal mental health management has been reported in many countries, which have recently implemented an obligatory screening, such as Poland (Chrzan-DČ©tkoś & Walczak-Kozlowska, 2020), Malaysia (Kang et al., 2019), and China (Gong et al., 2020). However, even having an adequate level of knowledge does not affect the practice enough (Arefadib et al., 2021; Kurtcu & Golbasi, 2014), as only 55% of healthcare professionals ever conduct a PPD assessment, even in the countries with a long tradition of screenings (Evans et al., 2015). When it comes to the screening procedures, some countries, for example Spain (Rodriguez et al., 2023), do not require conducting a routine PPD assessment in the perinatal period. Thus, screening depends more on local regulations. Moreover, healthcare systems that implemented an obligatory, routine PPD assessment differ in regulations and guidelines. In the United Kingdom and the Netherlands, CMs and CNMs receive clear guidelines about the screening procedure (Kendrick, & Pilling, 2021; Schiller et al., 2020). In Poland, however, CMs and CNMs are not provided with a list of suggested assessment tools (Regulation of the Ministry of Health on the organisational standard of perinatal care, 2018). Thus, asking a mother how she feels would be considered as following the recommendation, even though a screening based only on a conversation is less effective: when the primary care providers do not know the patients’ Edinburgh Postnatal Depression Scale (EDPS) scores, only around 50% of mothers with a clinically elevated EPDS score are identified (Anding et al., 2015). In other studies, PPD identification rates, without using a screening strategy, were lower than 30% (Coates et al., 2004). CMs’ and CNMs’ knowledge about PPD and screening methods are crucial to identify and refer women for further treatment, as most depressed mothers do not receive care (Cox et al., 2016; Watt et al., 2002). Cox et al. (2016) reported that in a group of women screened for depression at their prenatal visit, only 16% of those identified as possibly depressed later received treatment. Thus, we believe that the knowledge and engagement of CMs and CNMs into PPD management are an important factor in increasing the number of identified and treated women. In Poland, and probably in other Central and Eastern European countries, implementing the EU directive on the recognition of professional qualifications (Directive 2005/36) that introduced a mandatory module of psychology course was an important step in the systemic PPD management training for CMs and CNMs. Also, the perinatal care standard change in 2019 obliged the Midwifery Faculties to implement training about PPD screening procedures. Therefore, we assumed that the age of the CMs and CNMs can be a predictor of their knowledge, with younger CMs and CNMs having more knowledge, due to educational changes. Additionally, some studies highlight the role of CMs’ and CNMs’ attitudes toward mothers experiencing PMH problems. According to Hauck et al.’s (2015) and Jones et al.’s (2011) studies, even though CMs’ attitudes to PMH problems are in general positive, negative stereotypes of mental health problems still exist. The awareness of a potential bias is important to diminish or eliminate its influence on practice and care. Studies focusing on a mother’s perspective show the importance of CMs’ and CNMs’ attitudes: American mothers who sought help reported feelings of humiliation, frustration, and anger, all resulting from their interaction with healthcare professionals (Logsdon et al., 2012). Similarly, Australian mothers perceived their physicians as behaving patronizingly toward them (C. J. Jones et al., 2011). As the referral rates for PMH problems are low, the CMs’ and CNMs’ attitudes toward affected mothers can be an important factor influencing the PPD management outcomes. To be able to look after mothers’ emotional and mental needs, the CMs should be taken care of all well (Reiger & Lain, 2013), especially as the demands imposed on CMs and CNMs are growing: for example, PPD management constitutes additional work, while the resources do not increase. According to Reiger and Lain (2013), CMs and CNMs self-report frequent dilemmas concerning their wish to realise in practice their ideal of themselves as caregivers in what they call often “uncaring” workplaces. Additionally, the continuous staff shortages and witnessing perinatal trauma which leads to PTSD symptoms in 33% of CMs and CNMs (Sheen et al., 2015) may increase burnout. An excessive workload may prevent CMs and CNMs from implementing newly introduced vocational duties, such as PPD screening. An earlier study (Chrzan-DČ©tkoś & Walczak-Kozlowska, 2020) conducted in Poland on a different group of CMs and CNMs in the first six months after the implementation of the new perinatal care standard (Regulation of the Ministry of Health on the organisational standard of perinatal care, 2018), which introduced an obligation for the CMs and CNMs to monitor the maternal PPD risk and symptoms, showed that Polish CMs and CNMs self-assessed knowledge and preparation for screening was low, as they lacked expected expertise level in basic facts concerning the prevalence, screening, and treatment. In frames of “Next Stop: MUM” PPD intervention program implemented by Ministry of Health, we aimed to evaluate the effectiveness of a dedicated PPD management training in increasing knowledge about PPD management. Moreover, we wanted to investigate CMs’ and CNMs’ self-reported perception of systemic difficulties in the Polish healthcare system, and their self-evaluated competence in PPD management after three years of implementation of the obligatory PPD screening in Poland and their relations with involvement in PPD management. We also aimed to examine the declared general attitude of CMs and CNMs toward working with people experiencing mental difficulties and identify the most problematic areas. Moreover, we wanted to investigate the relationship between participants’ characteristics (age, job tenure, number of working hours per week, perceived educational preparation for PPD management, self-evaluated competence in PPD management, declared general attitude of CMs and CNMs toward working with people experiencing mental difficulties, and CMs’ and CNMs’ self-reported perception of systemic difficulties) and their actual knowledge of PPD management. More specifically, we hypothesized that: H1: CMs’ and CNMs’ knowledge of PPD management will increase after training. H2: CMs’ and CNMs’ younger age is linked to the higher level of knowledge of PPD management and self-perceived educational preparation. H3: Workload prevents CMs and CNMs from addressing women’s problems with depression and/or anxiety. H4: CMs’ and CNMs’ self-reported perceived systemic problems, attitudes toward working with people experiencing mental difficulties, and knowledge of PPD are associated with their involvement in PPD management. Additionally, to examine CMs’ and CNMs’ self-reported preparation and procedures they followed to manage patients with PPD, we asked them to respond to a set of questions. Since the new standard of PPD management has been introduced only recently, we did not formulate any hypotheses. Study Design For our analyses, we used data gathered during the realisation of the “Next Stop: MUM” PPD prevention programme, a part of a project: Development of the concept and substantive assumptions of health policy. According to the Ministry of Health guidelines, the PPD prevention programme had to be established through collaboration with 40 primary care health centres and seven obstetric departments within one macroregion (comprising three voivodeships). All primary healthcare centres and hospitals in this region received invitations to participate in the “Next Stop: MUM” PPD prevention programme. All CMs, CNMs, paediatric nurses, and other medical professionals responsible for the care of mothers and infants employed in these centres who chose to join the programme were required to undergo the training sessions. In our analysis, we only included the responses of CMs and CNMs. CMs and CNMs who participated in this project received six hours of remote training (conducted online due to the Covid-related national restrictions implemented at the time) concerning perinatal mental health. The training started and ended with a knowledge-based test. The small group workshops (instruction methods included a brief theoretical introduction followed by case studies and role-plays) were conducted by a psychologist. The first author developed educational materials for the training, which focused on fundamental PMH issues (PPD, anxiety, posttraumatic stress disorder) and outlining ways in which CMs and CNMs can provide support to mothers and families. Screening methods, chosen in accordance with the NICE guidelines, were also delineated. Furthermore, the specific responsibilities of CMs and CNMs in the project were detailed. These materials, serving as the foundation for the training sessions, were disseminated during the training. Participants A total of 420 people participated in the study. After excluding data provided by non-midwives and non-nurses, the final group consisted of only CMs (n = 306) and CNMs (n = 73), with an average age of 42.93 years (SD = 12.78, range = 22-68). Almost all (99%, n = 376) of the respondents were female, 0.3% male (n = 1), and 0.5% (n = 2) nonbinary. The average number of years worked was 19.02 (SD = 13.10, min. = 4 months, max. = 48 years). The participants worked for an average 42.24 h per week (SD = 10.79, range: 7-90). A majority of respondents, 85% (n = 319), were employed in the public sector, 7% (n = 28) in the private sector, and 8% (n = 32) in both. Most of the participants (73%, n = 278) worked in an urban area with more than 100,000 residents and 27% (n = 101) with fewer than 100,000 residents. Measures Sociodemographic Questionnaire It was developed by the first author, collecting respondents’ demographic data, years of clinical experience, type of practice, working hours per week, and self-reported educational preparation for PPD management. The Test of Antenatal and Postpartum Depression Knowledge (C. J. Jones et al., 2011) It is a single choice test, which measures medical staff’s knowledge of PPD management. The original version consists of 20 items – internal consistency, measured by Cronbach’s alpha = .69. The test was modified by the “Next Stop: MUM” PPD Programme Evaluation Board: the order of questions was changed, and seven questions added (Q12, Q13, Q14, Q16, Q17, Q19, Q20) (Appendix). The internal consistency for 27-item version that we used was Cronbach’s alpha = .67 (calculated on the responses before the training). One point is awarded for each correct answer (range: 0-27). We decided to put in additional questions concerning the EPDS scoring and interpretation to the measure, to better reflect a specific situation in Poland. Since an earlier study (Chrzan-DČ©tkoś & Walczak-Kozlowska, 2020) showed that using the EPDS, recommended by the Polish Ministry of Health as a screening method, was a challenge for CMs, a proper interpretation and communication of the result to the mother was a crucial part of the programme. Moreover, three years after the implementation of the new standard, we wanted to investigate CMs’ and CNMs’ potential difficulties and the knowledge in this area. The REASON Scale (C. J. Jones et al., 2012) It is a 17-item measure, which assesses midwives’ attitudes towards care for women with depression and anxiety. The responses are given on a seven-point Likert scale (from 1 – I strongly disagree – to 7 – I strongly agree). This measure comprises four factors (we cite sample items in brackets): 1) systemic problems (e.g., “I am too pressed for time to routinely assess women’s emotional health”, “Where I work the organisation of maternity services hinders midwives ability to get to know women well enough to give adequate emotional care”) (range = 5-35 points) – a higher score means reporting perceiving more systemic problems that hinder emotional care; 2) working with women experiencing emotional health problems (e.g., “I feel I cannot make a difference to women with emotional problem”) (range = 6-42 points) – a higher score means declaring a more negative attitude towards working with women experiencing emotional health problems; 3) using treatment techniques (e.g., “I feel competent in the use of counselling techniques”) (range = 4-28 points) – a higher score means a greater self-evaluated competence in the use of treatment techniques (e.g., counselling and relaxation); 4) referral (e.g., “I feel competent in knowing which women need to be referred to another health professional”) (range = 2-14 points) – a higher score means a greater self-assessed competence and a more positive attitude towards the referral of women with depression and anxiety to other health professionals. A Cronbach’s alpha of the original REASON total scale was .60, and for the “systemic problems”, “working with women experiencing emotional health problems”, “using treatment techniques”, and “referral” subscales were .85, .61, .79, and .36, respectively (C. J. Jones et al., 2012). In our sample, Cronbach’s alphas were .60, .77, .52, .66, and .39, respectively. While it is typically preferred for the internal consistency of a scale, as measured by Cronbach’s alpha, to be at least .70 or higher, a minimum of .60 is acceptable for new or modified scales (M. A. Jones et al., 1999). Therefore, we did not modify the original scale, as we found comparable consistency indices in our sample. Perception of own CMs’ and CNMs’ role and competence in PPD management was measured with first author-designed 22 statements, – e.g., “It is my responsibility to refer mothers with depression for further treatment”. The participants responded on a five-point Likert scale (from 1, I strongly disagree, to 5, I strongly agree) and rated the frequency of screening during their work using the scale from 1, never, to 5, every day (sample questions: “How often do you assess the severity of depressive symptoms in mothers?”, “How often do you use screening tools to measure the severity of postpartum depression symptoms?”). Since all these statements do not measure a single phenomenon, the response to each question was analysed separately, and no total score was calculated. Procedure All participants completed a sociodemographic questionnaire, the REASON scale, and rated their perceived knowledge and screening skills before the training. Moreover, they filled in the Test of Antenatal and Postpartum Depression Knowledge before and after the training. As 40 (11%) participants did not complete the knowledge-based test after the training, statistical analyses concerning the comparisons of the respondents’ knowledge about PPD management before and after the training include only the results of 339 respondents – this specifically refers to the data included in Table 1 and Table 2. The remaining data analyses use the responses of all participants. The CMs and CNMs who completed and who did not complete the knowledge test did not differ in age, average number of work experience in years, hours of work per week, work in the public vs. private sector, and prior educational preparation for PPD management. There were slight differences in the work place: more participants who dropped out worked in an urban area with fewer than 100,000 residents and fewer who worked in an urban area with more than 100,000 residents, as compared with the respondents who did not, 40% vs. 25%, and 60% vs. 75%, respectively, χ2(1) = 4.01, p = .043. CMs and CNMs who failed to complete the knowledge test after the training (M = 14.90, SD = 3.87) had a lower score on the knowledge test before the training as compared with the respondents who completed the test again, M = 16.10, SD = 3.63, t(377) = 1.97, p = .049, d = 0.33. Participants gave written informed consent before the testing. Statistical Analyses We used SPSS version 27.0 for statistical analyses. Since our sample sizes were large, we used parametric tests following the central limit theorem (King et al., 2018). We used Cronbach’s alpha to calculate internal consistency. We used descriptive statistics to examine respondents’ level of knowledge about PPD management and their attitudes towards care for women with depression and anxiety; t-test and McNemar test for dependent samples were computed to compare the level of knowledge before and after the training. To determine the difficulty of the items and the test as a whole and to examine CMs’ and CNMs’ perceived educational preparation and commitment to perform professional activities related to PPD management, we carried out frequency analyses. To examine links between CMs’ and CNMs’ characteristics (age, job tenure, the number of working hours per week, and perceived educational preparation) and their knowledge of PPD we calculated partial correlation analyses. To examine relationships between CMs’ and CNMs’ knowledge about PPD, their attitudes towards PPD management, and professional activities, we calculated correlation analyses. The CMs and CNMs’ Knowledge of PPD Management To test the first hypothesis, we conducted a t-test for dependent samples and a frequency analysis. A t-test for dependent samples revealed a significant increase in CMs’ and CNMs’ knowledge of PPD (as measured with the Test of Antenatal and Postpartum Depression Knowledge), by three points on average, after taking part in the training (Table 1). The largest increase in score for an individual participant was 18, while a decrease - six points. The effect size for the change in knowledge was very strong. Table 1 The Participants Knowledge of PPD before and after Training  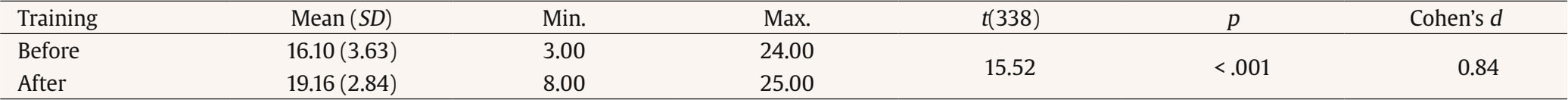 Note. n = 339 due to participant attrition. We defined as difficult these items of the Test of Antenatal and Postpartum Depression Knowledge (Table 2), which fewer than 75% of the respondents responded correctly to, following C. J. Jones et al. (2011). Both before and after the training, the most challenging ones (range of percent correct = 10-74; all changes in proportions were investigated with McNemar test) concerned the percentage of women suffering from prenatal depression who attempt suicide (I23), risk factors for prenatal depression (I24), interpreting the EPDS score (I12), the usual onset of postpartum depression (I7), the common treatment for depression (I25), the EPDS as an assessment tool (I11), the prevalence of antenatal depression (I2), the most frequent reason why mothers experiencing antenatal depression do not receive adequate help (I22), the prevalence of postpartum depression (I8), the consequences of perinatal mental disorders (I19), and the prevalence of “baby blues” (I4). The proportion of correct responses for all these items increased significantly after the training, except for items 22 and 25 (no change) and item 24 (a decrease in knowledge). Before the training, the most challenging items (range of percent correct: 38-74) concerned the EPDS scoring (I13), the relationship between perinatal psychiatric disorders and foetal development (I20), a recommended treatment for moderate to severe depression (I10), antidepressant medications and breastfeeding (I15), the consequences of antenatal depression (I21), the EPDS scoring (I14). After the training, the percentage of correct answers to these items increased to above 75%; each of these changes was significant. For 1 item, concerning the main symptom of antenatal depression (I26), only the score after the training fell below 75% correct; this change was significant. For items that more than 75% of the participants responded correctly to both before and after the training, a significant increase in knowledge was still found for the morbidity of depression and anxiety (I1), “baby blues” management (I5), symptoms and characteristics of PPD (I6 and I18), and mental health (I17). No change was observed for the items that asked about the persistence of antenatal depression (I3), the treatment for mild postpartum depression (I9), mood after delivery (I16), and the symptoms of PPD (I27). Generally, out of 27 items, an increase in the proportion of correct answers before and after the training was found for 19, no change for 6, and a decrease for 2. The average item difficulty was above .50 both before and after the training. Table 2 Item Difficulty in the Test of Antenatal and Postpartum Depression Knowledge Pre- and Posttest (N = 339)  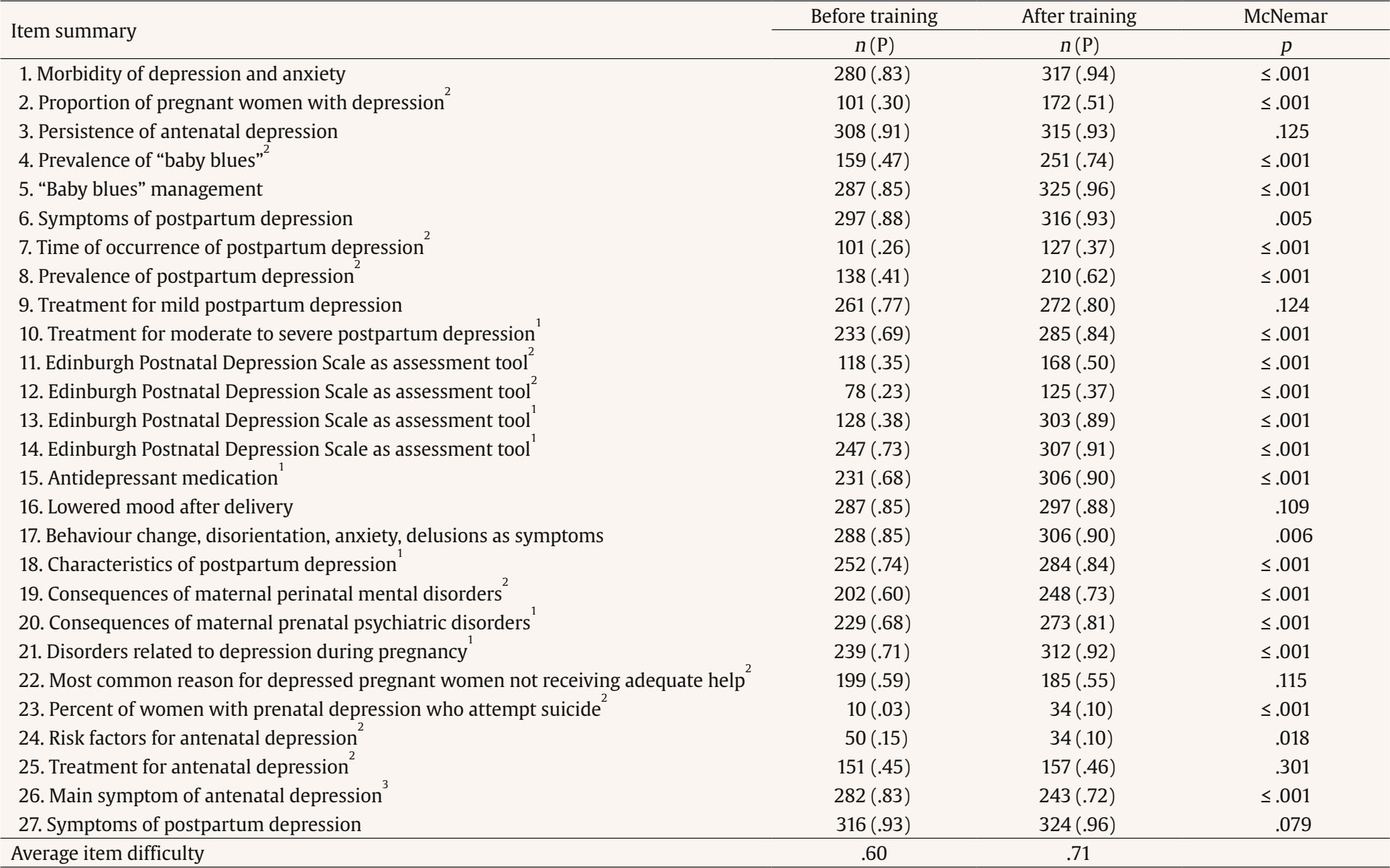 Note. n = number of correct answers; P = the number of correct answers divided by the number of both correct and incorrect answers; 1 p < .75 before training; 2 p < .75 both before and after training; 3 p < .75 after training; additional questions: Q12, Q13, Q14, Q16, Q17, Q19, Q20. A partial correlation analysis was conducted to test hypothesis 2 and investigate the relationship between CMs’ and CNMs’ individual characteristics, such as job tenure, working hours per week, perceived educational preparation for PPD management, and their knowledge about PPD management before training, whilst controlling for age. Our findings suggested that age exerted a substantial influence in controlling for the relationship between perceived educational preparation and knowledge, highlighting the importance of considering age as a factor in understanding this association. However, perceived educational preparation for PPD management also played a role. The results revealed a weak, positive partial correlation between CMs’ and CNMs’ perceived educational preparation and their knowledge about PPD while controlling for age (Table 3), which was statistically significant (indicating that the respondents who declared being more educated for PPD management did score more points in the PPD management knowledge test). The results revealed no statistically significant correlation between job tenure and the knowledge of CMs’ and CNMs about PPD while controlling for age. Moreover, there was no statistically significant correlation between working hours per week and the CMs and CNMs’ knowledge about PPD whilst controlling for age. Table 3 Partial Correlations, Controlling for Age, between Variables: Knowledge before Training, Job Tenure, Working Hours per Week and Perceived Educational Preparation for Peripartum Depression Management  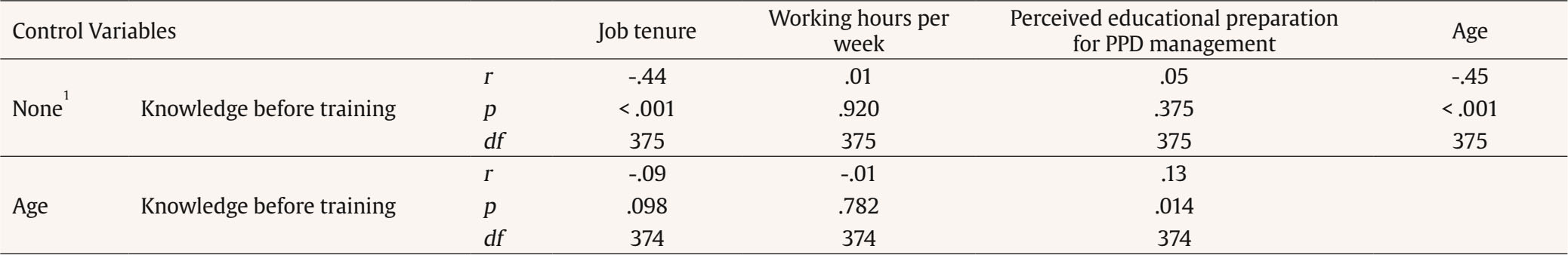 Note. 1 Cells contain zero-order (Pearson) correlations; N = 379; PPD = peripartum depression. Age correlated with the CMs and CNMs’ perceived educational preparation (r = .16, n = 379, p < .002, zero-order (Pearson) correlations). Attitudes of the CMs and CNMs toward their Role in the PPD Management To test the hypothesis 3, we assessed the attitudes of CMs and CNMs toward their role in the PPD management (measured with the REASON scale) using descriptive statistics. A significant percentage of CMs and CNMs (57%, n = 216) reported that their workload prevented them from addressing women’s problems with depression and/or anxiety. Half of the respondents (51%, n = 194) declared that the organisation of primary care health services hindered midwives’ ability to get to know women well enough to provide them with adequate emotional care (51%, n = 194). A significant percentage of CMs and CNMs reported feeling incompetent in counselling patients with anxiety (50%, n = 190). More than half of the participants reported experiencing too strong pressure for routine emotional health assessment (63%, n = 240), especially as, according to them, the questions about emotional health were treated by their patients as intrusive (57%, n = 215). Moreover, a significant percentage of CMs and CNMs declared that organisational culture prioritised focusing only on problems communicated by a woman rather than on exploring underlying issues (64%, n = 244). More than half of the respondents reported feeling competent to recognise a need for referral to another health professional (60%, n = 229), but uncomfortable when questioning women about emotional disorders (56%, n = 213). Two-thirds of CMs and CNMs declared that they accepted their primary role in the treatment of women with anxiety disorders (67%, n = 252), but a vast majority (93%, n = 351) reported that they believed that patients with anxiety disorders should be referred to a counsellor, psychiatrist, or psychologist. Moreover, the average rating score for the perception of systemic problems that “hindered” emotional care was 17.70 points (out of 35 possible; SD = 6.28, range = 5-35), and for respondents’ perceived competence in using treatment techniques it was 12.78 points (out of 28 possible; SD = 4.31, range = 4-25). The declared attitudes toward working with women experiencing emotional difficulties were rated at an average level, almost exactly in the middle between a positive and a negative attitude, of 22 points (out of 42 possible; SD = 6.19, range = 6-41), and self-evaluated competence towards the referral of women with depression and anxiety to other health professionals was 9.84 points on average (out of 14 possible; SD = 2.41, range = 2-14), indicating an above average self-evaluated competence. Table 4 Correlations Between the Subscales of the REASON Scale and the Frequency of Involvement of Certified Midwives and Nurse Midwives in Peripartum Depression Management  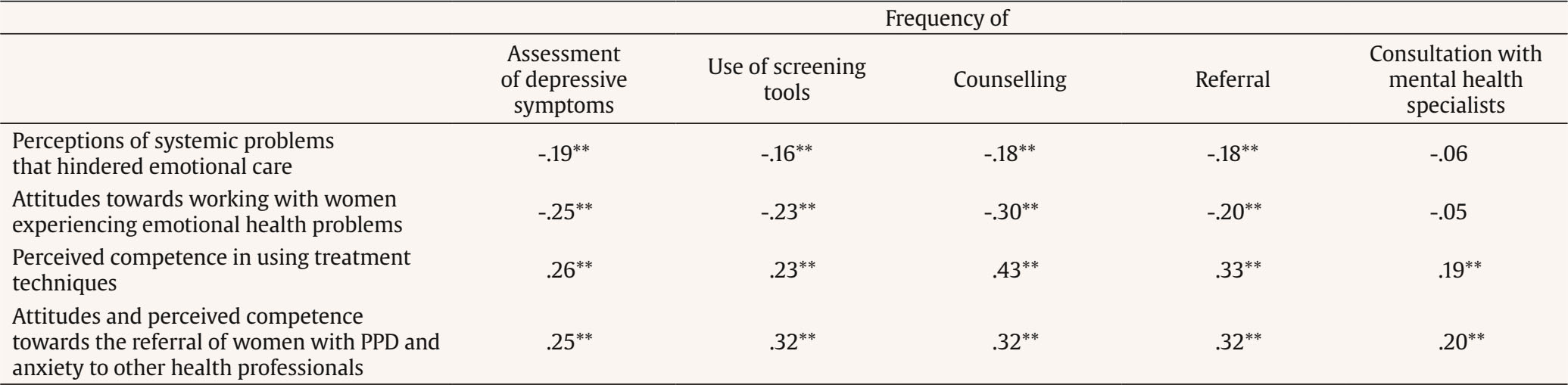 Note. N = 379; PPD = peripartum depression; Pearson product-moment correlations. ** p ≤ .01. Table 5 Correlations between the Midwives and Nurses’ Knowledge about the Peripartum Depression before the Training and the Frequency of their Involvement in its Management and between the Subscales of the REASON Scale  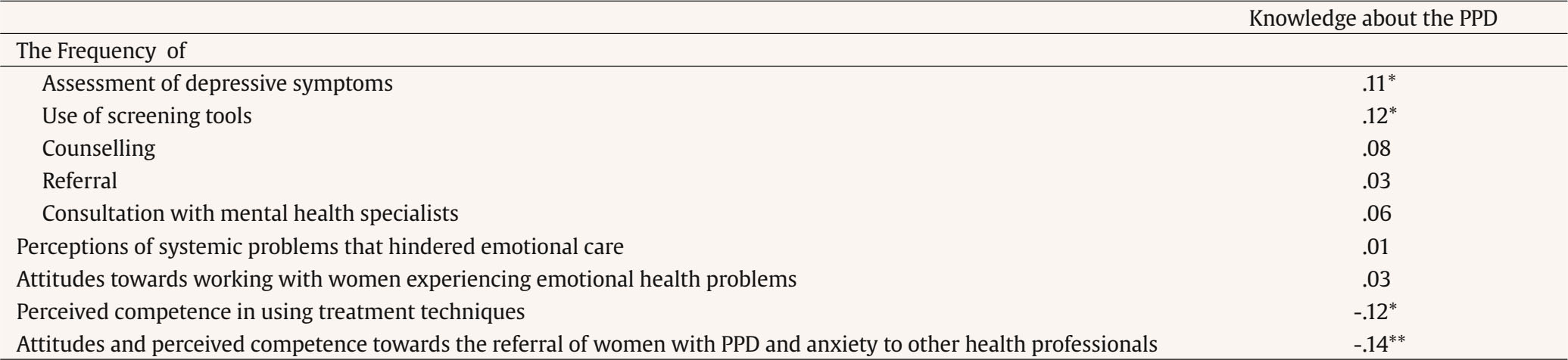 Note. N = 379; PPD = peripartum depression; Pearson product-moment correlations. * p ≤ .05, ** p ≤ .01. The CMs and CNMs’ Self-reported Perceived Systemic Problems, Attitudes toward Working with People Experiencing Mental Difficulties, the Knowledge of PPD and Their Involvement in PPD Management A correlation analysis, which we conducted to test hypothesis 4 (Table 4) showed that CMs’ and CNMs’ self-reported observation of a greater number of systemic problems hindering their ability to provide emotional care to patients was associated with the less frequent assessment of the severity of depressive symptoms, using screening tools in their work, counselling their patients, and referring them to mental health specialists (weak correlations). Similarly, the respondents’ declared more negative attitudes toward working with women experiencing emotional difficulties were associated with the less frequent assessment of the severity of depressive symptoms, using screening tools in their work, counselling their patients, and referring them to mental health specialists (weak correlations). Moreover, CMs’ and CNMs’ self-reported more positive self-assessment of their competence in using therapeutic techniques and referring patients to specialists was associated (weak and moderate correlations, respectively) with more frequent assessment of the severity of depressive symptoms, using screening tools in their work, counselling their patients, and referring them to mental health specialists. Also, in line with hypothesis 4, respondents’ higher knowledge about PDD was associated with the more frequent assessment of the severity of depression and using screening tools (weak correlations, Table 5) and more positive attitudes and higher perceived competence towards referral of women with depression and anxiety to other health professionals (weak correlations, Table 5). However, the higher knowledge was associated with their lower self-evaluated competence in using treatment techniques. CMs’ and CNMs’ Self-reported Preparation and Procedures they Followed to Manage Patients with PPD – a Description Additionally, we compared the actual questionnaire (the Test of Antenatal and Postpartum Depression Knowledge and the REASON scale) results with the self-declarations of CMs and CNMs when they were asked about it directly and we asked them to respond to a set of questions. Since the new standard of PPD management has been introduced only recently, we did not formulate any hypotheses. On this basis we calculated CMs’ and CNMs’ self-reported preparation and reported procedures to manage patients with PPD. The results are presented below. We found that only a small percentage of CMs and CNMs (17%, n = 66) declared before training that they believed to be educated for PPD management, as measured with the “set of statements”. A significant proportion of the respondents (83%, n = 313) had no prior educational preparation for PPD management. Moreover, all respondents rated their preparation, on average, as equal to 4.23 points (SD = 0.98, range = 1-7), suggesting an average level. A significant percentage of participants (69%, n = 263) reported that they were required to recognize depression in mothers. A similar proportion (67%, n = 255) declared that depression identification was their responsibility. We found that a majority of CMs and CNMs declared that treating women with depression was not their responsibility (76%, n = 286), but referral for further treatment was (70%, n = 265). Two-thirds (66%, n = 249) of the respondents reported that they were not able to recognise PPD and did not know the diagnostic criteria (70%, n = 265). The CMs and CNMs who took part in our study declared that they rarely or never measured the severity of depressive symptoms (79%, n = 299), used screening tools (81%, n = 308), referred their patients for further treatment (92%, n = 348), provided advice on PPD (82%, n = 312), and consulted a mental health specialist about a patient with depression (82%, n = 312). A minority of our respondents (32%, n = 121) reported feeling comfortable when discussing depression with the patient or her family, while a substantial majority declared that they had never attended training on the assessment (71%, n = 268) or the treatment of PPD (74%, n = 281). Only a small percentage of our participants (11%, n = 44) reported satisfaction with the availability of mental health professionals. Most participants (82%, n = 316) declared their willingness to screen for PPD in their work and almost all (95%, n = 360) to learn how to improve their management of patients with mental health problems. Our study aimed to assess the effectiveness of a PPD management training workshop, defined as an increase of CMs’ and CNMs’ knowledge about PPD management in a primary care setting. The trainings sessions were conducted two and three years after the implementation of the new standard of perinatal care, including PPD management, in Poland (Regulation of the Ministry of Health on the organisational standard of perinatal care, 2018), which introduced an obligation for CMs and CNMs to assess PPD symptoms and risk. Our results showed that 83% of participants had no prior educational preparation for PPD management, as declared in a sociodemographic questionnaire. Our first hypothesis was confirmed. The training proved successful, and we found a very strong effect size for the increase in knowledge. Generally, out of 27 items an increase in the proportion of correct answers before and after the training was found for 19, no change for 6, and a decrease for 2. Like C. J. Jones et al.’s (2011) findings, our study indicated that CMs and CNMs lacked adequate knowledge of how to use the EPDS. Our participants had difficulties with identifying effective therapeutic methods for PPD, which is in line with reports that midwives are unsure of how to manage women with PPD (Coates & Foureur, 2019; Eden, 1989; C. J. Jones et al., 2011) and are not eager to suggest appropriate treatment strategies (Eden, 1989; C. J. Jones et al., 2011). We believe that, even though CMs and CMNs do not and should not provide treatment outside their area of expertise, it still may be helpful for them to know the basic information about methods, e.g., to better advise the mothers. Our second hypothesis, concerning CMs and CNMs age as a factor linked with the level of knowledge of PPD management and perceived educational preparation, was also confirmed. We found that a self-evaluated better educational preparation for PPD management was related to a deeper knowledge of PPD management only when we controlled for age. This was because, although younger age was associated with actually knowing more about PPD management, the older age was linked with perceiving oneself as more educated. Thus, our findings highlighted the importance of considering age as a factor in understanding the association between perceived educational preparation, job tenure, and knowledge. The average age of our participants was over 40 years, while the average age of CMs and CNMs in Poland is 53, and it is projected to increase in the coming years (Main Council of Nurses and Midwives [NIPiP, 2022]). Special attention should be paid to provide training for older CMs and CNMs, as they graduated from programmes that did not include PMH management (the information about PPD management in midwifery and nursing courses has been obligatory in midwifery education only in recent years). Our third hypothesis focused on the self-reported workload of the CMs and CNMs as a factor preventing the effective management of PPD patients, according to respondents’ own assessment, and was also confirmed. C. J. Jones et al.’s (2012) study showed that midwives acknowledged the importance of perinatal mental health care, but their perceived lack of competence compromised their willingness to offer assistance and provide emotional care. In contrast to our results, more than half of the midwives did not perceive systemic problems such as workload, organisational priorities, and time as factors hindering their care for women with emotional distress (C. J. Jones et al., 2012). Our respondents had a higher average of working hours per week than required by the Act on Health Facilities of 1991 (42 hours and 15 minutes per week vs. 38 hours and 55 minutes per week), which can lead to work overload. Additionally, the emotional work of midwives is often unseen and unsupported, and that can be an additional cause of work overload (Rayment, 2015). According to Sheen et al.’s (2015) study, empathy, a valued characteristic for CMs, is associated with more severe posttraumatic stress responses in CMs when exposed to traumatic events. Data concerning CMs’ and CNMs’ general health are also alarming and supporting the hypothesis of the pressure and work overload: in the moment of death, CMs’ and CNMs’ average age is only 62.3 years. These figures are significantly lower than the general population figures: average age of death for women in Poland is 81.8 years (NIPiP, 2022). Introducing systemic support for CMs and CNMs could be an important factor for effective PPD management. As our fourth hypothesis stated, CMs’ and CNMs’ self-reported more negative attitudes toward working with women experiencing emotional difficulties were associated with a less frequent assessment of the severity of depressive symptoms, using screening tools in their work, counselling their patients, and referring them to mental health specialists. Additionally, importantly for clinical practice, self-reported knowledge about the techniques used to manage PMH issues, a more positive self-assessment of the respondents’ competence in using therapeutic techniques and referring patients to specialists correlated positively with active PPD management. These results are in line with Bina et al.’s (2019) study findings and Fekadu et al.’s (2022) systematic review and meta-analysis: improving PPD identification needs to be combined with improving capacity to provide care. As the fourth hypothesis also stated, CMs’ and CNMs’ self-reported observation of a greater number of systemic problems was associated with the less frequent assessment of the severity of depressive symptoms, using screening tools in their work, counselling their patients, and referring them to mental health specialists. Also, according to other studies (e.g., Tai-Seale et al. 2007), systemic problems such as time constraints and conflicting demands in the ‘real-world’ primary care settings are a major challenge for an effective depression treatment (in the general population, not only in mothers with PPD). In general, more than 50% of potential cases of depression remain unidentified even in high income countries, which shows the universality of depression management problems in primary health care and an urgent need to improve this proportions (Mitchell et al., 2009). Our results demonstrated that higher knowledge about PPD was associated with more frequent depression assessment and using screening tools, which is in line with Bina et al. (2019). The greater knowledge about the PTSD helps CMs and CNMs understand their vocational duties concerning PMH. Of course, while caring for mothers, CMs and CNMs should focus on screening and referral, and not on treatment, as this is not a part of their duties. There are some studies, however, showing that interventions conducted by CMs, such as a listening visit, are effective in PPD management. At this moment, though, such options do not exist in the Polish health care system. We assume that this result demonstrated a more responsible attitude, showing that a deeper knowledge includes a clearer understanding of one’s role in PMH management. This can also help with work overload. This study’s participants felt competent in knowing which women needed to be referred to another health professional and 92% recognized when mothers should be referred to a counsellor, psychiatrist, or psychologist, what confirms their recognition of their duties. These findings are contradictory to Bina et al.’s (2019) results, which demonstrated that the better midwives and nurses self-evaluated their knowledge, the better they also perceived their competence in using treatment techniques. These discrepancies can be explained by the fact that the measurement of knowledge in our study was an objective single choice response test, and in Bina et al.’s (2019) it was a subjective self-assessment. Additionally, we investigated CMs’ and CNMs’ responses to statements concerning PPD management in their practice. Before taking part in our training, more than half of the participants (66%) declared that they were not able to recognize PPD symptoms and 70% did not know the diagnostic criteria. Most respondents (79%) reported that they rarely or never assessed the severity of maternal depression symptoms and 81% did not use screening tools, despite 82% expressing their willingness to screen for PPD in their work. Similarly, C. J. Jones et al.’s (2011) study revealed that Australian midwives were willing to play a more active role. Unfortunately, they often faced a lack of adequate educational preparation and systemic constraints. Most of the CMs and CNMs in our study self-reported that they recognized their role in screening and identifying symptoms of depression. However, although 67% of the respondents declared that they considered depression identification a part of their workplace responsibilities, 69% indicated that it was required of them, and 70% claimed that they believed that referring women to specialists for further treatment was their duty, most of them self-reported that they rarely or never assess the severity of depressive symptoms (79%). They did not either use screening tools (81%), and actually made referrals (92%), which is key for the success of PPD management. Similarly, most midwives and nurses who participated in Bina et al.’s (2019) study evaluated their knowledge regarding PPD as average, but perceived carrying out the screening as important and as part of their responsibilities. Our findings are contradictory to reports that a sense of responsibility for PPD identification promotes commitment to PPD management (Kang et al., 2019; Leiferman et al., 2008). A significant proportion (76%) of our participants did not consider treating women with depression as their responsibility, 82% rarely or never gave advice on PPD and consulted a mental health specialist about a patient with depression (in fact, only 11% of the respondents reported satisfaction with the availability of mental health professionals), and only 32% felt comfortable discussing depression either with a mother or her family. In practice, PMH care provided by CMs and CNMs is hindered rather by a perceived lack of competency and knowledge, systemic problems, and work overload than a lack of interest. Most of our participants declared that they regarded PMH management as their duty. CMs’ and CNMs’ competency in the assessment and care of women with PPD should be enhanced through continuing professional education. One training, although proved effective, is not enough to ensure the implementation of good practices. Limitations There was significant attrition – almost 11% of CMs and CNMs failed to complete the knowledge test after the training. These participants did not differ from their colleagues who completed the test twice in terms of sociodemographic characteristics (except for small differences in place of residence) and being educated for PPD management. They, however, scored lower in the knowledge test. Thus, we have no data on how successful training would be for CMs and CNMs who exhibited the lowest knowledge of PPD. Our participant sample was also biased in the respect that they participated in a governmental programme which provided them with free of charge training. The majority of CMs and CNMs in Poland are not offered such trainings. Although CMs’ and CNMs’ perceptions of attitudes and systemic problems had been assessed before the training, they were not the main focus of training, what limits the possibility to draw definite conclusions about the overall impact of the training programme and the importance of self-perceived attitudes and competencies after training. CMs’ and CNMs’ self-perceived attitudes, competence, confidence, or comfort levels in addressing mental health might have changed. Their attitudes toward routinely assessing women’s emotional health or counselling patients with PPD and anxiety could have evolved, potentially aligning more closely with the best practices promoted by the training. In future studies, we would like to assess self-perceived attitudes and competence both before and after training, to give us a full insight in the potential change in this aspect. Probably, a single training session would not be enough to change CMs’ and CNMs’ attitudes. Likely, regular supervisions would be needed. However, during the training we noticed that CMs and CNMs talked about their attitudes, what highlights the importance of this issue for them. Additionally, in our study we used self-report measures. Thus, a lack of congruency between statements and actual behaviour may limit the generalisability of conclusions. Moreover, although reliability coefficients of measures are acceptable, they are quite low. The measures (the Test of Antenatal and Postpartum Depression Knowledge and the REASON scale) we used have not been validated in Poland. Moreover, the internal consistency of the REASON Scale was low, so the results need to be treated tentatively. Possibly, a follow-up work using factor analysis could be conducted to modify the scales for Polish conditions; however, reliability coefficients that we calculated using our data is comparable to those of the original tools. Additionally, due to the covid-19 pandemic, training sessions were offered only remotely and results could have been different in face-to-face conditions. Although some researchers do not find any differences between online and in-person education, data concerning midwifery education are unambiguous. Milne et al.’s (2014) study showed a higher participation in face-to-face midwifery education activities as compared with online video conferencing. Geraghty et al. (2019) explored students’ experiences in completing online theory courses and found a preference for face-to-face learning, due to the opportunities for asking questions, raising issues, and seeking confirmation of thoughts. Also, non-midwifery students rated online courses more negatively than in-person ones. Probably, individual preferences or an adaptation to online learning could influence individual achievements and could have also influenced our results – for example, Price Banks and Vergez’s (2022) study found a weak but positive relationship between student achievement and the perception of learning modality. Lastly, most of our statistical analyses are correlational, so we cannot infer a causal relationship between reported systemic issues and CMs’ and CNMs’ knowledge. Conclusions Our study confirmed that CMs’ and CMNs’ knowledge about PPD management increased after the conducted training and it was associated with PPD management. Emotional work of midwives is often unseen and unvalued, and in our study the system, which obliged CMs and CNMs to expand the emotional care they had already provided and monitor the risk and symptoms of PPD, failed to support them in this new vocational task. Even short training sessions for CMs and CNMs can facilitate the delivery of evidence-based care and enhance maternal mental health outcomes (Arefadib et al., 2021; Legere et al., 2017). Our recommendations are presented in Table 6. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgement We would like to thank all participants of the “Next Stop: MUM” perinatal mental health trainings for their involvement in the project. Cite this article as: Chrzan-Dętkoś, M., Murawska, N., & Łockiewicz, M. (2024). Certified midwives and nurse-midwifes’ knowledge and attitudes about peripartum depression management – the effectiveness of a peripartum depression management training. Clínica y Salud, 35(2), 63-75. https://doi.org/10.5093/clysa2024a12 Funding: This study is a part of a program: “The Next Stop: Mum”, which was implemented on the basis of the contract with the Ministry of Health for co-financing project No. POWR.05.01.00-00-0023/18 under the Operational Program Knowledge Education Develop-ment 2014-2020, co-financed from the European Social Fund. However, sponsor did not have any involvement in the study design, collection, analysis and interpretation of data, writing of the report nor the decision to submit the article for publication. References Appendix
|
Cite this article as: Chrzan-Dętkoś, M., Murawska, N., & Łockiewicz, M. (2024). Certified Midwives and Nurse-Midwifes’ Knowledge and Attitudes about Peripartum Depression Management – The Effectiveness of a Peripartum Depression Management Training. ClĂnica y Salud, 35(2), 63 - 75. https://doi.org/10.5093/clysa2024a12
Correspondence: magdalena.chrzan-detkos@ug.edu.pl (M. Chrzan-Detkos).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 CrossRef
CrossRef JATS
JATS







