Psychological Intervention on Health, Self-Esteem, and Coping in Siblings of Patients with Severe Mental Disorders
[IntervenciĂłn psicolĂłgica en la salud, la autoestima y el afrontamiento de hermanos de pacientes con trastornos mentales graves]
Carolina Reyes-González1, María Nieves Pérez-Marfil1, 2, Gloria M. Roldán3, Isabel C. Salazar1, and 2
1Faculty of Psychology, University of Granada, Spain; 2Mind, Brain and Behaviour Research Centre (CIMCYC), University of Granada, Spain; 3Mental Health Day Hospital, Virgen de las Nieves University Hospital, Granada, Spain
https://doi.org/10.5093/clysa2024a14
Received 7 November 2023, Accepted 16 April 2024
Abstract
Background: This study examined the effectiveness of a psychological intervention on self-esteem, perceived stress, perceived health problems, coping strategies, psychological inflexibility, and caregiving experience in siblings of patients with severe mental disorders (SMD). Method: 42 Siblings of patients with SMD participated. The psychological intervention was based on the third wave of cognitive-behavioural therapy and consisted of 14 group sessions. Pre- and post-treatment assessment were conducted in the intervention group (IG) and compared with the control group (CG). Results: IG significantly increased self-esteem, adaptive coping, and positive caregiving experience and reduced perceived stress, perceived health problems, psychological inflexibility, maladaptive coping, and negative caregiving experience. The effect sizes were moderate to large. No changes were reported for the CG in the post-treatment evaluation. Conclusions: The psychological intervention for siblings was effective in relation to the variables assessed. This is an innovative approach to care within the health system for siblings of people suffering from SMD.
Resumen
Antecedentes: Este estudio evalúa la eficacia de una intervención psicológica sobre la autoestima, el estrés percibido, los problemas de salud percibidos, las estrategias de afrontamiento, la inflexibilidad psicológica y la experiencia en cuidados de hermanos de pacientes con trastornos mentales graves (TMG). Método: Participaron 42 hermanos de pacientes con TMG. La intervención psicológica estaba basada en la terapia cognitivo-conductual de tercera generación y consistió en 14 sesiones de grupo. Se realizó una evaluación antes y después del tratamiento en el grupo de intervención (GI) y se comparó con el grupo control (GC). Resultados: El GI aumentó significativamente en autoestima, afrontamiento adaptativo y experiencias positivas de cuidado y disminuyó en estrés percibido, problemas de salud percibidos, inflexibilidad psicológica, afrontamiento desadaptativo y experiencias negativas de cuidado. Los tamaños del efecto fueron de moderados a grandes. El GC no mostró cambios en el postratamiento. Conclusiones: La intervención psicológica en los hermanos ha sido eficaz y es una propuesta de asistencia innovadora dentro del sistema sanitario en hermanos de personas que padecen TMG.
Palabras clave
IntervenciĂłn psicolĂłgica, Hermanos, Trastorno mental grave, Autoestima, Salud, Afrontamiento, CuidadosKeywords
Psychological intervention, Siblings, Severe mental disorder, Self-esteem, Health, Coping, CaregivingCite this article as: Reyes-González, C., Pérez-Marfil, M. N., Roldán, G. M., & Salazar, I. C. (2024). Psychological Intervention on Health, Self-Esteem, and Coping in Siblings of Patients with Severe Mental Disorders. ClĂnica y Salud, 35(2), 85 - 93. https://doi.org/10.5093/clysa2024a14
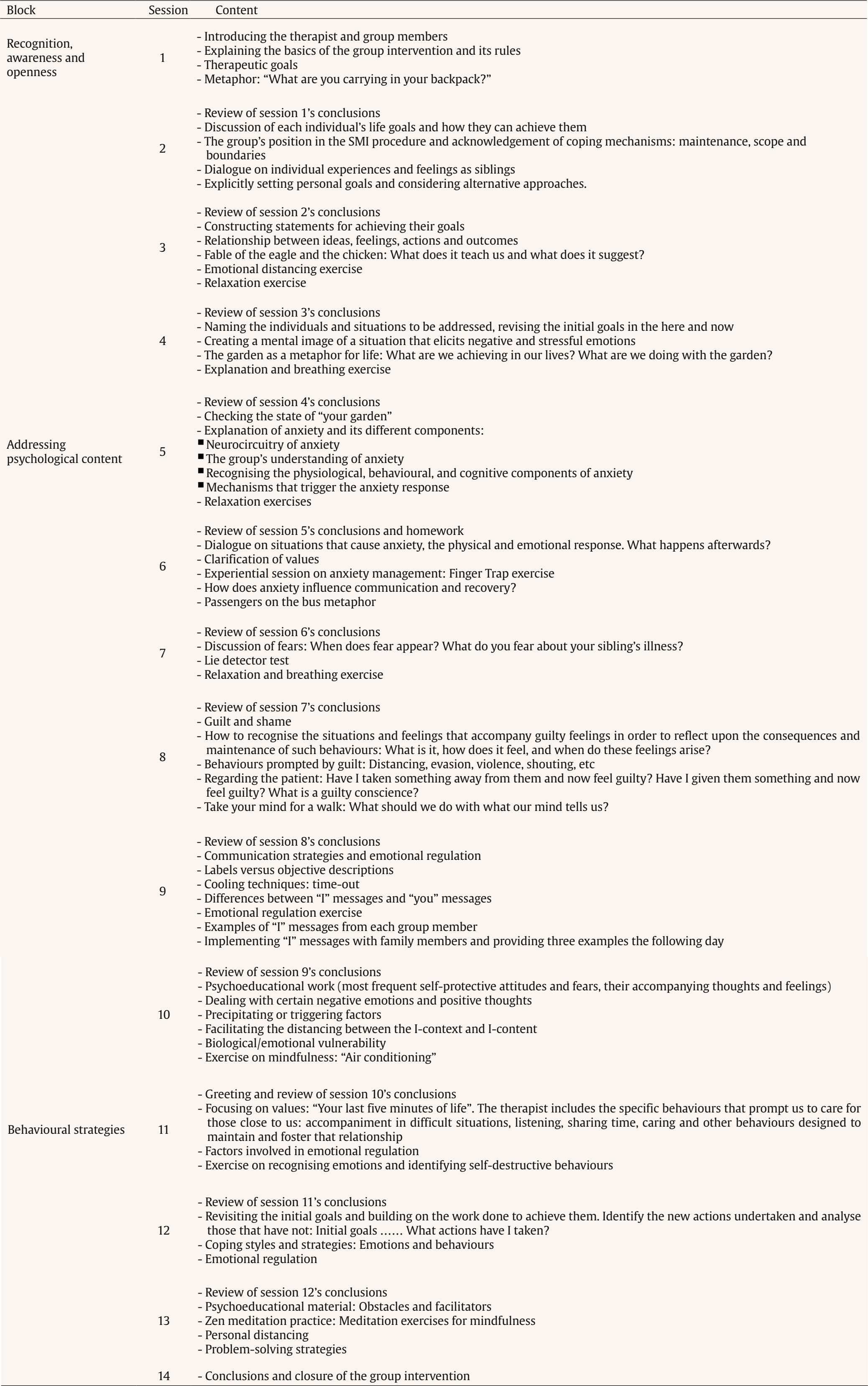
Correspondence: isabelsalazar@ugr.es (I. C. Salazar).Mental disorders are at the root of many clinical and behavioural issues. The definition of severe mental disorders (SMD) includes factors of a psychosocial, temporal, and disabling nature, as well as cognitive, affective, and social alterations that have a major impact on the lives of patients and their families (Roldán et al., 2015). These problems affect the everyday lives and well-being of everyone involved (Polo-López et al., 2016). Such disorders include the schizophrenia spectrum and other psychotic, depressive, bipolar, and related disorders, including personality disorders. In Spain, these diagnoses are the fourth most common reason for need of care from relatives and non-professionals (Navarro et al., 2019). SMD do not affect every family member in the same way. Parents and caregivers are the most affected by issues relating to quality of life, coping skills, distress/anxiety, and burnout (Caqueo-Urízar et al., 2012; González-Fraile et al., 2018; Lahera et al., 2020; Polo-López et al., 2016; Roldán et al., 2015). Meanwhile, siblings report feeling mixed emotions, including love, pain, anger, envy, guilt, and shame, stemming from challenges associated with grieving the loss of a “healthy brother or sister”, their fear of also inheriting an SMD (Stålberg et al., 2004), psychological distress (Plessis et al., 2020), stress (Seeman, 2013), the use of coping strategies (Avcıoğlu et al., 2019; Friedrich et al., 2008), subjective burden (Avcıoğlu et al., 2019; Pierazzuoli et al., 2020; Shivers et al., 2023), uncertainty about their future as primary caregivers as their parents age (Smith et al., 2007), and the need for support for their own psychological needs (Amaresha et al., 2014). However, to our knowledge, there are no empirically validated treatment programmes tailored to this cohort and their needs that mitigate the effects of their experience of their sibling’s SMD outside of the healthcare system (Friedrich et al., 2008; Nechmad, 2000). Family intervention programmes in the field of SMD (Lahera et al., 2020; Navarro et al., 2019) have so far yielded significant benefits for both caregivers and patients. These programmes have been shown to improve treatment, care, and recovery (Sampietro et al., 2023), outperforming cases without family interventions (Vallina Fernández & Lemos Giráldez, 2000). However, a review of the participants in these psychological interventions reveals a high level of participation by parents, particularly mothers, who are usually the primary caregivers and typically shoulder the greatest burden. Siblings tend to benefit only from psychoeducation, which is mainly delivered by nursing professionals (Sin et al., 2015). As a result, the lack of interventions targeting siblings of people with SMD within the mental healthcare system (at least in terms of empirical evidence) means that siblings are often the unsung (Friedrich et al., 2008). Third-wave therapies (also known as contextual-behavioural therapies) represent an innovative approach to psychotherapy that goes beyond traditional behavioural and cognitive-behavioural models. These therapies focus on promoting psychological flexibility and values-based living, with an emphasis on the context in which thoughts, feelings, and behaviours are experienced. This study presents an intervention protocol based on third wave of cognitive-behavioural therapy (CBT) and consisting of three interrelated blocks: (1) recognition, awareness, and openness, (2) addressing psychological content, and (3) behavioural strategies. This clinical protocol emphasised issues such as mindfulness, acceptance, emotions, values, goals, cognitive defusion, psychological flexibility and the therapeutic relationship, following Hayes and Hofmann (2017). Study Aim and Hypothesis The aim of the current study was to examine the effectiveness of a group-based psychological intervention using techniques from the third wave of CBT on self-esteem, perceived stress, perceived health problems, coping strategies, psychological inflexibility, and caregiving experience in siblings of patients with SMD. The main hypothesis of the study is that siblings in the intervention group (IG) will improve their self-esteem, coping strategies, and caregiving experiences, while reducing perceived stress, perceived health problems, and psychological inflexibility. In addition, the control group (CG, no intervention) will have no significant changes in these psychological variables. Participants The initial sample size of 47 siblings was determined using G-Power v. 3.1.9.2 software. This calculation was based on a significance level of 5%, a power of 80%, and a mean effect size of 0.39, based on the effect size of a previous group psychological intervention with families (Roldán et al., 2015). The pre-intervention assessment included a total of 50 siblings. The two groups (IG and CG) were formed after asking participants if they were willing to take part in the study. The siblings were informed about what their participation would entail, and the two groups were formed, each consisting of 25 siblings of patients with SMD at the University Hospital (HU) of Granada (Spain). Over the course of the study, three siblings from the IG declined to participate and did not attend the group on their scheduled days, and five siblings from the CG were excluded because they did not attend the post-intervention assessment. At the end of the process a total of 42 siblings had taken part in the study. Table 1 Socio-demographic and Background Information for the Intervention and Control Groups  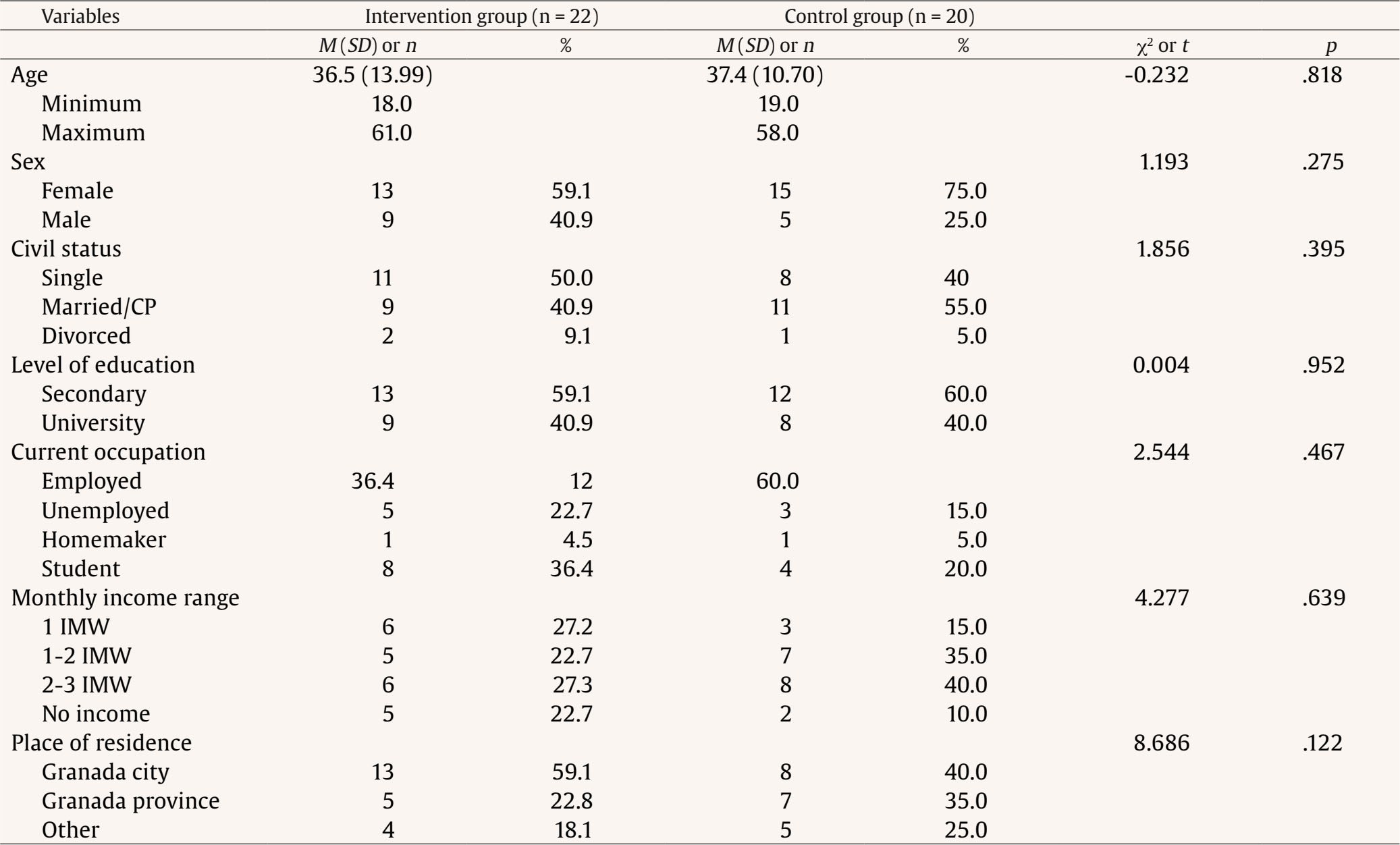 Note. CP = civil partnership; IMW = interprofessional minimum wage. To be included, participants had to meet the following criteria: being a sibling of a person diagnosed with an SMD, being at least 16 years old, providing signed informed consent, either personally or from a legal guardian, living with or caring for the patient in a relationship considered close by both parties, agreeing to participate in the study and being available to do so, and not having received direct mental health support and/or been involved in any psychological/psychiatric intervention related to the patient with an SMD. Exclusion criteria were as follows: inability to commit to the study, diagnosis of neurological disorder or history of cerebral damage, substance abuse or dependence, intellectual disability, or SMD. Table 1 shows the socio-demographic and background information for the two groups. There were no statistically significant differences between the groups for any of these variables. Measures and Variables Ad-hoc Semi-structured Interview This interview was used to collect data on the following variables: age, sex, relationship status, level of education, current occupation, monthly income range, place of residence, people in their care, therapeutic support, and length of time since the patient’s disorder was diagnosed. Rosenberg Self-Esteem Scale (RSES; Rosenberg, 1973; Spanish version by Vázquez et al., 2004) This is a 10-item self-report instrument used to assess self-esteem. It consists of four response options ranging from strongly disagree (1) to strongly agree (4). It assigns both direct (1, 2, 4, 6, and 7) and inverse (3, 5, 8, 9, and 10) scores. Scores below 25 are considered low self-esteem, scores between 26 and 29 are considered moderate self-esteem, and scores between 30 and 40 are considered normal self-esteem. Internal consistency, measured by Cronbach’s alpha, was reported to be .87 in the study by Vázquez et al. (2004) and .86 in our study. Coping Strategies Inventory (CSI; Tobin et al., 1989; Spanish version by Cano et al., 2007) This is a 40-item self-report instrument that assesses coping strategies in four categories: adaptive problem-focused (problem solving and cognitive restructuring), adaptive emotion-focused (social support and emotional expression), maladaptive problem-focused (problem avoidance and wishful thinking), and maladaptive emotion-focused (social isolation and self-criticism). High scores indicate greater use of the strategies. Internal consistency, measured by Cronbach’s alpha, ranges from .63 to .86 (Cano et al., 2007), with a coefficient of .78 observed in our study. General Health Questionnaire (GHQ-28; Goldberg & Hillier, 1979; Spanish version by Lobo et al., 1986) This is a 28-item questionnaire that assesses an individual’s general perception of health and provides an initial screening for psychopathology using four subscales: Somatic symptoms, Anxiety, Social dysfunction, and Depression. Cronbach’s alpha for the overall score is reported as .97 (Godoy-Izquierdo et al., 2017). In our study, it was .93 for the overall score, .85 for Somatic symptoms, .67 for Anxiety, .83 for Social dysfunction, and .89 for Depression. Perceived Stress Scale (PSS; Cohen et al., 1983; Spanish version by Remor, 2006) This is a 14-item self-report instrument that assesses perceived stress levels over the last month. Scores of 0-14 indicate that the individual is rarely or never stressed, 15-23 sometimes stressed, 24-42 often stressed, and 43-56 constantly stressed. Cronbach’s alpha is .82 (Remor, 2006) and .87 in this study. Experience of Caregiving Inventory (ECI; Szmukler et al., 1996; Spanish version by Crespo-Maraver et al., 2019) This is a 66-item self-report instrument that measures caregivers’ assessment of both positive and negative aspects of the caregiving experience. Positive aspects include positive personal outcomes and good aspects of the relationship with the patient. Negative aspects include difficult behaviours, negative symptoms, stigma, problems with (social and healthcare) services, effects on the family, need for backup, dependency, and loss. High scores on the positive and negative subscales reflect a positive or negative appraisal of caregiving, respectively. Cronbach’s alpha ranges from .72 to .88 in the study by Crespo-Maraver et al. (2019). In our study, Cronbach’s alpha for the overall score was .92. Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011; Spanish version by Ruiz et al., 2013) This questionnaire measures psychological inflexibility and consists of seven items on a Likert-type scale. To interpret the results, the scores obtained for each item are added together. Higher scores indicate a higher level of psychological inflexibility. Participants without clinical problems had a mean score ranging from 18 to 23 points. Participants with clinical problems averaged over 29 points. Cronbach’s alpha as reported by Ruiz et al. (2013) is .88, and here it is .87. Procedure This quasi-experimental study, featuring a pre-post design with experimental and control groups, was approved by the UH Ethics Committee (code 1894-N-19), the management of the Mental Health Service, and the supervisors of the respective mental health units where it was carried out. It was conducted in accordance with the ethical principles of the Declaration of Helsinki and the Council of Europe Convention on Human Rights. All participants read and signed an informed consent form. The research objectives were explained to the staff of each mental health unit who helped to identify patients with siblings. Patients were asked for permission to contact their siblings, and siblings who agreed to take part invited to attend an initial assessment. Those who met the inclusion criteria were asked if they were willing to participate in the study. In this way, the initial group of 50 siblings was formed. Once their willingness to participate and be part of the therapeutic group was confirmed, the IG was established. The siblings who did not receive the intervention were assigned to the CG. All participants were assessed in two one-hour sessions. The IG was divided into three groups, with the first and third groups consisting of eight siblings and the second group of six siblings. At the end of the intervention, both IG and CG groups were assessed using the same self-report instruments. Table 2 Between-group Differences in Perceived Health, Perceived Stress, Self-esteem, and Psychological Inflexibility  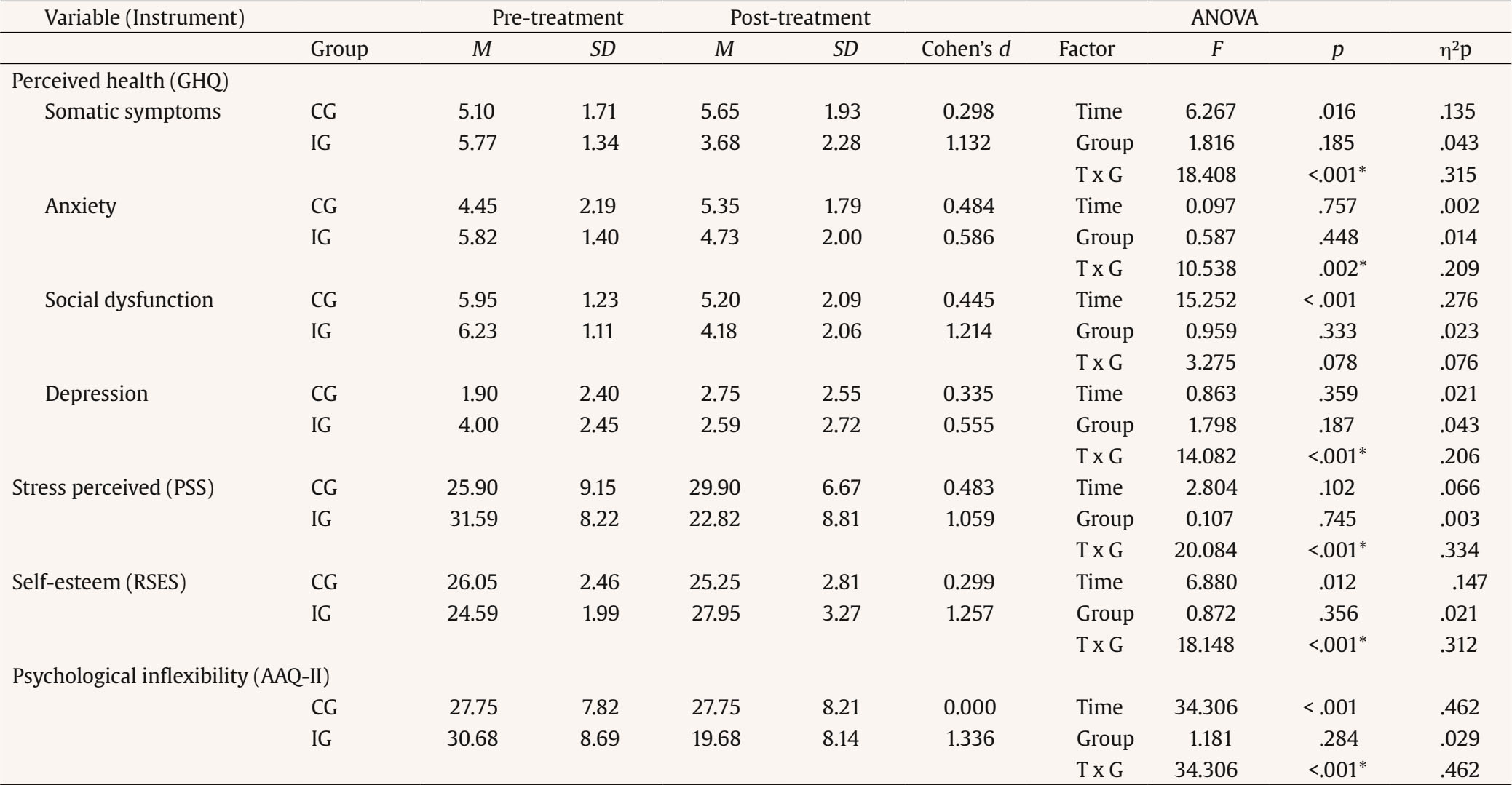 Notes. CG = control group; IG = intervention group; T x G = (interaction) time x group; GHQ = General Health Questionnaire; PSS = Perceived Stress Scale; RSES = Rosenberg Self-Esteem Scale; AAQ-II = Acceptance and Action Questionnaire-II. * p < .05. Table 3 Between-group Differences in Caregiving Experience and Coping Strategies  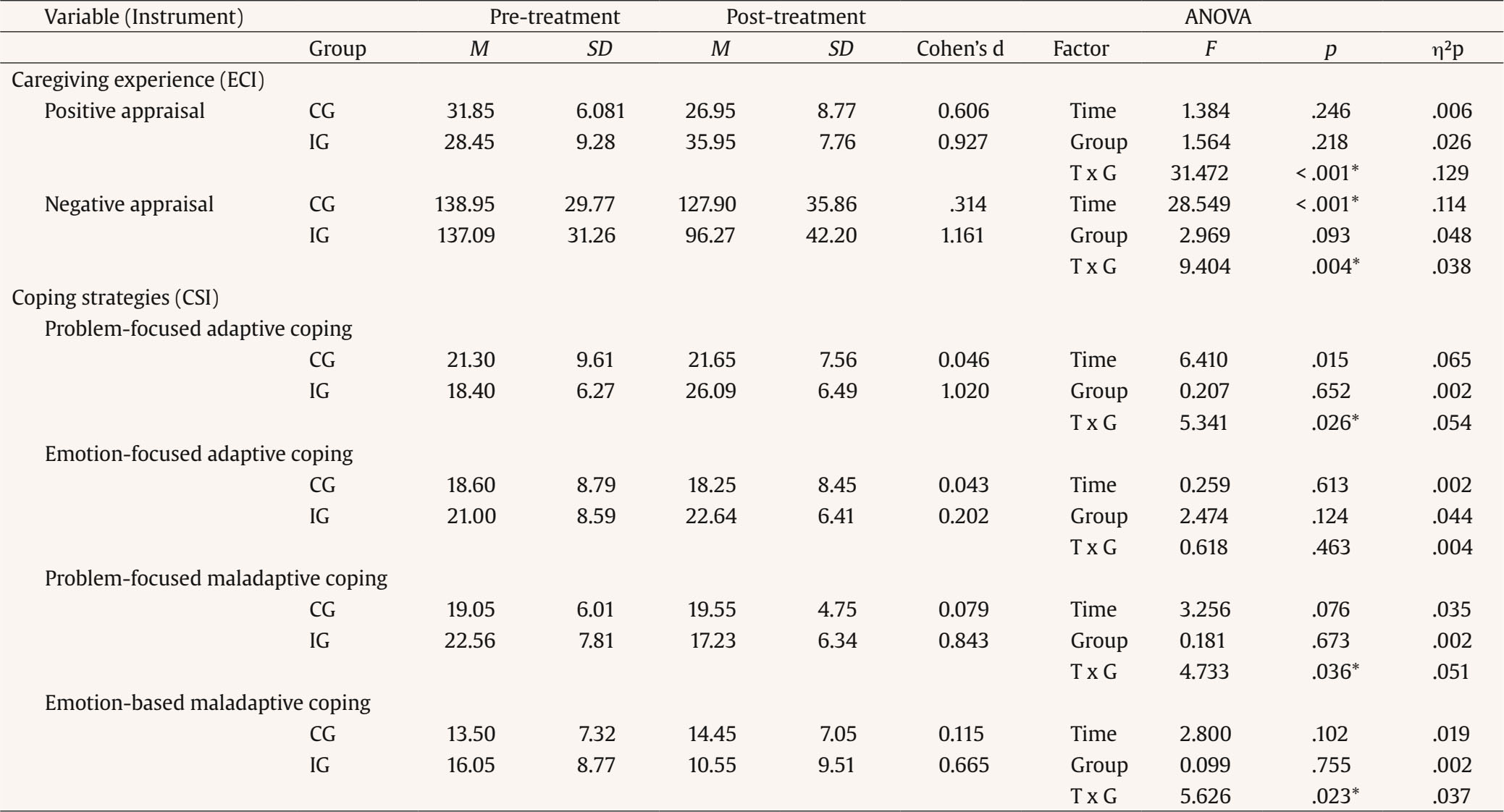 Notes. CG = control group; IG = intervention group; T x G = (interaction) time x group; ECI = Caregiver Inventory; CSI = Coping Strategies Inventory. * p < .05. The psychological intervention was based on the third wave of cognitive-behavioural therapy and consisted of 14 group sessions divided into three blocks: 1) recognition, awareness and openness (sessions 1 to 4), 2) addressing psychological content (sessions 5 to 9), and 3) behavioural strategies (sessions 10 to 14) (see Appendix). Each session lasted two hours and took place once a week in the hospital attended by the patients with SMD. An experienced clinical psychologist and a co-therapist delivered the intervention. Data Analysis Data were analysed using JASP v.0.16.3 software (JASP Team, 2022). Descriptive analyses (means, standard deviations, and frequencies) were performed on the socio-demographic and clinical variables. Between-group differences were analysed using the Student’s-t test for independent samples and the chi-squared test (χ²). Repeated measures linear models (Wilks’ λ) were used to assess the impact of the programme. In all cases, the assumption of homogeneity of variance was assessed using Levene’s test. Effect size was calculated using Cohen’s d and partial eta squared (η²p). Impact was also determined using the intervention as the independent variable, while the scores recorded in the various pre-post self-report instruments used in each group served as the dependent variables. The significance threshold was set at p < .05. Tables 2 and 3 show the means, standard deviations and effect sizes (η²p and Cohen’s d), as well as the between-group differences, assessment time and Time x Group (T x G) interactions of the various psychological variables assessed. Perceived Health Problems The GHQ-28 revealed significant differences in the T x G interaction for Somatic symptoms (F = 18.408, p ≤ .001, η²p =.315), Anxiety (F = 10.538, p = .002, η²p = .209), and Depression (F = 14.082, p ≤ .001, η²p = .206). In the second assessment, the scores were lower in the IG and higher in the CG. Cohen’s d indicated that the intervention had a large effect on the IG in terms of Social dysfunction (d = 1.214) and Somatic symptoms (d = 1.132), and a moderate effect in terms of Anxiety (d = 0.586) and Depression (d = 0.555). There were also significant differences in Somatic symptoms (F = 6.267, p = .016, η²p = .135) and Social dysfunction (F = 15.252, p ≤ .001, η²p = .276) for the time factor, indicating changes at the time of the second assessment (Table 2). Perceived Stress The PSS showed significant differences in the T x G interaction (F = 20.084, p ≤ .001, η²p = .334). Following the intervention, perceived stress increased in the CG and decreased in the IG. Cohen’s d indicates that the intervention had a large effect on the IG (d = 1.059) (Table 2). Self-esteem The RSES revealed significant differences in the T x G interaction (F = 18.148, p ≤.001, η²p = .312). The second evaluation showed an increase in self-esteem in the IG and a decrease in the CG. Cohen’s d indicates that the intervention had a significant effect on the IG (d = 1.257). There were also differences in the time factor (F = 6.880, p = .012, η²p = .147), reflecting changes between the first and second assessments (Table 2). Psychological Inflexibility The AAQ-II showed significant differences in the T x G interaction (F = 34.306, p ≤ .001, η²p = .462). The IG exhibited a reduction in psychological inflexibility, whereas CG levels were unchanged in the second evaluation. Cohen’s d indicates that the intervention had a large effect on the IG (d = 1.336). There were also differences in the time factor (F = 34.306, p = ≤ .001, η²p = .462), reflecting changes between the first and second assessments (Table 2). Caregiving Experience The ECI recorded statistically significant differences in the T x G interaction in “positive appraisal” (F = 31.472, p = ≤.001, η²p = .129) and “negative appraisal” (F = 9.404, p = .004, η²p = .038) of the caregiving experience. There was an increase in “positive appraisal” and a decrease in “negative appraisal” for the IG, while the opposite was true in the CG. Cohen’s d indicates a major impact in the IG for both “positive appraisal” (d = 0.927) and “negative appraisal” (d = 1.161) of caregiving as a result of the intervention. There were also significant differences in the time factor for “negative appraisal” (F = 28.549, p = ≤ .001, η²p = .114) of the caregiving experience, indicating changes in this variable at the second assessment (Table 3). Coping Strategies The CSI showed significant differences in the T x G interaction for “problem-focused adaptive coping” (F = 5.341, p = .026, η²p = .054), “problem-focused maladaptive coping” (F = 4.733, p = .036, η²p = .051) and “emotion-based maladaptive coping” (F = 5.626, p = .023, η²p = .037). The intervention increased “problem-focused adaptive coping” and decreased “problem-focused maladaptive coping” and “emotion-based maladaptive coping” in the IG, whereas there were no changes in any of these variables in the CG at the second assessment. Cohen’s d indicates a large effect in the IG for “problem-focused adaptive coping” (d = 1.020) and “problem-focused maladaptive coping” (d = 0.843), and a moderate effect for “emotion-focused maladaptive coping” (d = 0.665). The intervention also led to significant differences in the time factor for problem-focused adaptive coping (F = 6.410, p = .015, η²p = .065) (Table 3). The aim of this study was to examine the effectiveness of a group-based psychological intervention utilizing techniques from the third wave of cognitive behaviour therapy on the self-esteem, perceived stress, perceived health problems, coping strategies, psychological inflexibility, and caregiving experience in siblings of patients with SMD. The findings suggest that the programme led to increases in self-esteem, the use of problem-focused adaptive coping strategies and positive perceptions of health problems. There were also decreases in perceived stress, the use of problem- and emotion-focused maladaptive coping strategies, negative appraisals of the caregiving experience, and psychological inflexibility. By contrast, psychological difficulties (e.g., psychological inflexibility) persisted and even deteriorated in those who did not participate in the programme (CG). We can therefore conclude that the data support the main hypothesis of the study. One of the more significant changes concerns “psychological inflexibility”. These changes reflect the programme’s content and exercises, which are designed to help participants better understand their own psychological processes and learn new ways of dealing with distress and psychological challenges. The programme teaches participants to adopt a dispassionate perspective when observing experiences (e.g., having a sibling with an SMD), focus on the present, accept negative emotions, distance themselves from thoughts that exacerbate distress, and behave in accordance with their personal values. Interventions of this kind have yielded positive outcomes in families of people with SMD (e.g., Roldán et al., 2015) and in patients with some form of mental disorder (e.g., Salazar et al., 2022). The “self-esteem” variable also experienced a significant increase following the intervention. This is another notable finding, as self-esteem tends to be affected in family members of people with an SMD (Navarro et al., 2019), highlighting the importance of reinforcing it through psychiatric rehabilitation programmes. Although the intervention programme did not specifically target self-esteem, the change in the way individuals judged themselves (and their self-worth) could be attributed to acceptance, the development of a value system and support for actions guided by such values. These findings cannot be compared with other studies of siblings of people with an SMD, as no such studies exist. However, other research on group-based third-wave of CBT has documented its benefits for the self-esteem of people with other psychological problems (e.g., Salazar et al., 2022). Participants in the study also reported improvements in terms of “perceived health”. There were significant reductions in somatic symptoms, anxiety, and depression. These types of health problems and vulnerability to them have been reported in siblings of people with SMD (Friedrich et al., 2008). Given the prevalence of depressive and anxiety disorders in Spain and worldwide, tackling these issues should be a priority in mental health care. It is important to reiterate that there are no previous studies of interventions involving a sample such as ours. However, studies have been conducted with parents/caregivers of people with SMD whose symptoms of anxiety and depression have been alleviated by psychological interventions like this one (Navarro et al., 2019; Roldán et al., 2015). The effectiveness of the psychological intervention programme is demonstrated by the changes observed in participants’ “perceived stress” levels. The results show that siblings can learn to cope with stress, especially in complex situations such as those brought on by SMD. It is widely recognised that stress is the product of a person’s interaction with their environment. In this context, the programme is designed to build individuals’ capacity to better understand how psychological responses are triggered and then learn to control them. It is evident that interventions are needed to help siblings of people with SMD to manage and reduce stress (Friedrich et al., 2008; Nechmad, 2000; Roldán et al., 2015), and we now have a tool that fulfils this requirement. Regarding “coping strategies”, the changes observed after treatment indicate an improvement in the use of adaptive coping strategies, especially those focused directly on the problem, alongside a significant reduction in the use of maladaptive strategies. The intervention programme directly promotes adaptive coping by incorporating some of the techniques that help with emotional regulation (e.g., mindfulness, breathing, and defusing dysfunctional thoughts). It also assists in overcoming problems and challenging situations. Previous research has highlighted the importance of problem-focused coping for people’s well-being (Avcıoğlu et al., 2019) and the role of emotion-focused coping in caregiving (Avcıoğlu et al. 2019; Friedrich et al., 2008). One last positive finding relates to the change in siblings’ appraisals of their “caregiving experience” with patients with an SMD. The results suggest that their involvement in the programme led to an increase in positive experience and a decrease in negative experience. A particular highlight of the programme is its emphasis on exercises and the use of metaphors to help participants express their emotions, reflect on how to behave in a way that is consistent with their values and fully enjoy the here-and-now without judgement. The success of this approach is clearly reflected in the improvement in the psychological flexibility of the participants. In our opinion, this helps them to be less intolerant of the situations they face due to the severity of the disorder and thus improves their appraisal of the experience. This study has yielded several positive outcomes and has pioneered research into how siblings of people with SMD can benefit from psychological interventions specifically tailored to their needs (e.g., self-esteem, perceived health, and perceived stress) and to issues that indirectly affect the patient. These include changes in their caregiving experience, as well as coping and problem-solving strategies. To date, most interventions involving relatives of patients with SMD have targeted parents (Amaresha et al., 2014). Although the disorder affects the whole household, siblings have been largely overlooked by healthcare services. Therefore, bearing in mind the empirical evidence on the impact of parental interventions on the recovery/rehabilitation of patients with an SMD (González-Fraile et al., 2018; Navarro et al., 2019; Roldán et al., 2015), we contend that the treatment programme examined here will benefit not only the siblings, but also the patients themselves. This may provide families with strategies for mental health prevention, detection, and support. There are some limitations to this study. One such limitation is the way in which the intervention and control groups were set up. Although all siblings agreed to take part in the study, not all could be included in the IG due to time constraints or scheduling problems. These participants were assigned to the CG, potentially introducing bias into the research findings. Another limitation was the lack of any kind of follow-up to determine whether the benefits of the programme were sustained in the medium and long term. Finally, we believe that there is a need to enrol more participants in the intervention programme to achieve greater generalisability. In conclusion, the group-based psychological intervention using third-wave of CBT in siblings of patients with SMD was found to be effective. This is evidenced by improvements in adaptive coping, self-esteem, and positive caregiving experience and reductions in maladaptive coping, perceived health problems, stress, and psychological inflexibility. This optimises the time and care that professionals can devote to healthcare service users. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgements We extend our thanks to the siblings who participated in this research, to the patients with an SMD who attended the Mental Health Units and granted their consent, and to the healthcare professionals who provided us with the necessary help to make the study possible. Cite this article as: Reyes-González, C., Pérez-Marfil, M. N., Roldán, G. M., & Salazar, I. C. (2024). Psychological intervention on health, self-esteem, and coping in siblings of patients with severe mental disorders. Clínica y Salud, 35(2), 85-93. https://doi.org/10.5093/clysa2024a14 References |
Cite this article as: Reyes-González, C., Pérez-Marfil, M. N., Roldán, G. M., & Salazar, I. C. (2024). Psychological Intervention on Health, Self-Esteem, and Coping in Siblings of Patients with Severe Mental Disorders. ClĂnica y Salud, 35(2), 85 - 93. https://doi.org/10.5093/clysa2024a14
Correspondence: isabelsalazar@ugr.es (I. C. Salazar).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS