
Health Behaviors and Sleep Quality in Portuguese Adolescents: The Moderating Role of Age and Gender
[Los comportamientos relativos a la salud y la calidad del sueño en los adolescentes portugueses: el efecto moderador de la edad y del sexo]
Silvia Pucci, Ana C. Almeida, and M. Graça Pereira
Universidade do Minho, Campus de Gualtar, Braga, Portugal
https://doi.org/10.5093/clysa2024a9
Received 18 January 2023, Accepted 17 November 2023
Abstract
Background: Adolescence is marked by changes such as sleep and health behaviors. This study analyzed the relationships and differences on excessive daytime sleepiness, anxiety and depression symptoms, sleep habits, family sleep behaviors, sleep quality and health behaviors in adolescents including the moderating effect of adolescents’ age and gender. Method: The sample included 272 adolescents, 58% being female. Results: Girls and older adolescents reported worse sleep quality. Older adolescents reported healthier behaviors. Female gender, having a family member with sleep quality problems, coffee intake, anxiety and depression symptoms, daytime sleepiness, and family sleep behaviors contributed to worse sleep quality. Father’s alcohol consumption, anxiety and depression symptoms and family sleep behaviors contributed to adolescents’ sleep habits. Being a girl and an older adolescent were moderators in the relationship between the presence of excessive daytime sleepiness and worse sleep quality. Conclusions: Findings highlight the importance of health promotion programs regarding sleep quality.
Resumen
Antecedentes: La adolescencia está marcada por los cambios en el sueño y comportamientos referidos a la salud. Este estudio analizó las relaciones y diferencias en la somnolencia diurna excesiva, los síntomas de ansiedad y depresión, los hábitos de sueño, los comportamientos de sueño familiares, la calidad del sueño, los comportamientos de salud en adolescentes, incluido el efecto moderador de la edad y el sexo de los adolescentes. Método: La muestra de este estudio estaba compuesta por 272 adolescentes, siendo el 58% de sexo femenino. Resultados: Las niñas y los adolescentes mayores indicaron una peor calidad del sueño. Los adolescentes mayores manifestaron comportamientos más saludables. Ser de sexo femenino, tener un familiar con problemas de sueño, consumir café, tener síntomas de ansiedad y depresión, así como somnolencia diurna y conductas de sueño familiares se asocian con una peor calidad del sueño. El consumo de alcohol del padre, los síntomas de ansiedad y depresión y las conductas de sueño familiares se asocian con los hábitos de sueño de los adolescentes. Ser niña y adolescente de mayor edad modera la relación entre la presencia de somnolencia diurna excesiva y peor calidad del sueño. Conclusiones: Los resultados resaltan la importancia de los programas de promoción de la salud en relación con la calidad del sueño.
Palabras clave
Adolescente, Comportamientos de referidos a la salud, Ansiedad, Depresión, Calidad del sueño, Somnolencia diurna excessivaKeywords
Adolescent, Health behaviors, Anxiety, Depression, Sleep quality, Excessive daytime sleepinessCite this article as: Pucci, S., Almeida, A. C., & Pereira, M. G. (2024). Health Behaviors and Sleep Quality in Portuguese Adolescents: The Moderating Role of Age and Gender. ClĂnica y Salud, 35(1), 5 - 12. https://doi.org/10.5093/clysa2024a9
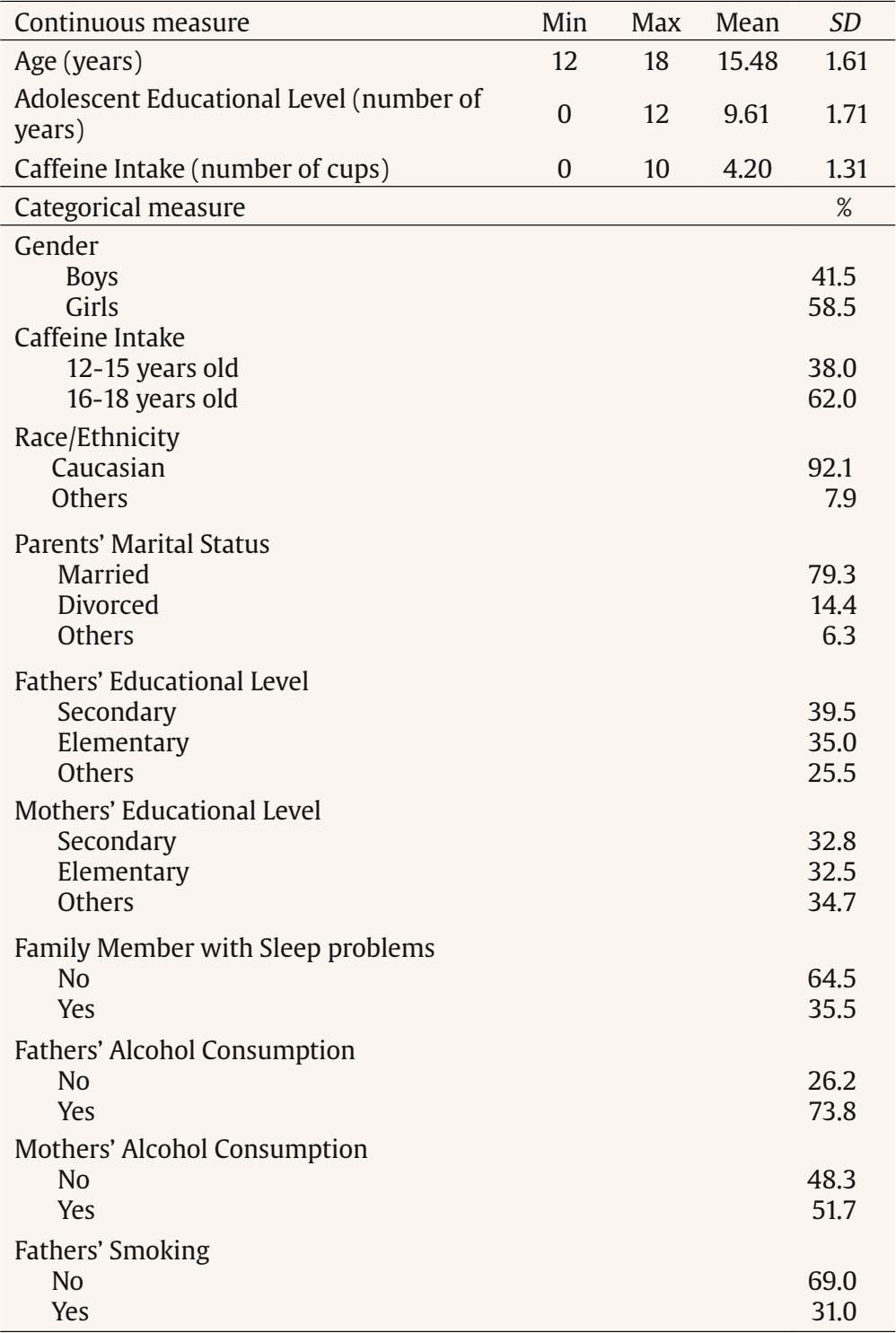
Correspondence: gracep@psi.uminho.pt (M. Graça Pereira).Sleep occurs in a sociocultural context and is influenced by a number of interrelated social and environmental characteristics (Spilsbury et al., 2017). Many variables impact sleep quality in adolescents such as sleep habits, family sleep behaviors, health behaviors, and anxiety and depression symptoms (Crowley et al., 2018). Sleep habits are defined as the behaviors regarding time to go to bed, time to rise, drinking coffee at night, duration of night sleep, and consumption of sleeping pills (Sweileh et al., 2011). Family sleep behaviors include parenting practices and styles regarding sleep (Spilsbury et al., 2017). Routines, enforced rules and parental monitoring of adolescents’ activities, sleep related, are generally associated with greater sleep duration, quality, or both (Spilsbury et al., 2017). Habits at night, such as the use of technology (e.g., TV, video game, text messages) and consumption of caffeine showed that adolescents may present an increased arousal during the night, excessive daytime sleepiness, with a reduced level of functional status, and alertness (Calamaro et al., 2009). Excessive daytime sleepiness can be interpreted as a decreased state of alertness or as considerably higher sleepiness. Excessive daytime sleepiness increases with biological, psychological, and social factors affecting negatively the quantity and quality of sleep (Owens et al., 2020; Thorarinsdottir et al., 2019). Adolescents with adequate sleep reported more health behaviors, such as a healthy lifestyle (e.g., exercising, having a good meal with vegetables and fruits) (Chen et al., 2006). In turn, adolescents with poor sleep quality, such as sleep restrictions and sleep loss, report more health risk behaviors such as smoking, and consumption of alcohol and drugs (Eaton et al., 2012). Sleep problems in adolescence have also been studied in connection with family sleep behavior. Family characteristics, such as family environment, emotional climate, and rules, may impact adolescents’ sleep quality (Whalen et al., 2017). Furthermore, just as family sleep behavior may impact adolescents’ sleep quality, family health behaviors may also impact adolescents’ health behaviors (Whalen et al., 2017). Sleep habits may show a significant impact on sleep quality in adolescents, besides the sleep disturbance, with consequences such as excessive daytime sleepiness and anxiety and depression symptoms (depression and anxiety) (Lapidaire et al., 2019). The literature has shown a relationship between sleepiness, depression, and anxiety with sleepiness being related to higher levels of depressive and anxiety symptoms, and the latter contributed to excessive sleepiness (Roberts & Duong, 2013). Literature shows that the prevalence of poor sleep quality in European adolescents is high, with almost 60% of adolescents showing sleep problems (Thorsén et al., 2020), which may contribute to depressive symptoms, less motivation to daily function, negatively influencing their mental health (Wang et al., 2021), learning capacity (Bugueño et al., 2017), being associated with addictive behaviors, such as nicotine dependence, internet addiction, and substance abuse (Rosi et al., 2020). The decline in adolescents sleep quality was exacerbated by the COVID-19 pandemic (Wang et al., 2021), with adolescents sleeping patterns changing such as fewer hours of sleep and difficulty in falling asleep, which may interfere negatively not only with their cognitive skills, but also with their mood and well-being (Buonsenso & Rose, 2021). A literature review on gender differences regarding sleep suggested different mechanisms of sleep modulation according to gender (Mong & Cusmano, 2016). Studies found that girls report worse sleep quality than boys (Tang et al., 2017). However, there are still obscure processes concerning the understanding of the variables that involve sleep process in women, and especially in adolescents. Blake et al. (2018) in a randomized control trial about the relationship between cognitive-behavioral sleep interventions and adolescents sleep quality found that adolescents’ gender was not a significant moderator in this relationship, although female adolescents reported poor sleep quality and more internalizing symptoms (high anxiety and depressive symptoms) than male. Also, in Lewien et al’s (2021) study regarding the relationship between sleep habits and sleep-related difficulties found that either adolescents’ gender or age was a significant moderator in this relationship. However, Jahrami et al. (2019), in their literature review regarding excessive daytime sleepiness and sleep quality in students, found that age and gender were not moderators, perhaps because the relationship between gender and sleep problems may reflect cultural influences. The literature presents, therefore, mixed results regarding the moderating effect of age and gender regarding sleep quality. In stressful situations, like sleep disturbance caused by the presence of daily sleepiness, coping strategies depend on the individual’s cognitive and emotional appraisal to manage their internal and external demands according to his or her resources (Maes et al., 1996). Thus, this study took into consideration Maes et al.’s (1996) model, that was derived from the cognitive-appraisal model and analysis of the coping process with a chronic disease. This model considers that disease and treatment characteristics, disease-related events, and demographic characteristics are related to the appraisal of demands and goals and to emotional and cognitive responses. All these factors directly or indirectly influence coping behaviors, that may be moderated by external and internal resources. All these factors contribute to the psychological, social, and physical dimensions of quality of life through coping (Maes et al., 1996). Thus, in this study excessive daytime sleepiness was considered a symptom of sleep disturbance with impact on adolescents’ physical and emotional health. Sociodemographic characteristics included either adolescent’s characteristics (age, gender, consumption of psychoactive substances: coffee, caffeine beverages, and energetic sodas) and parent’s characteristics (presence of sleep problems and consumption of psychoactive substance with nicotine and alcohol). Anxiety and depression symptoms were considered the emotional and cognitive response of sleep disturbance and a moderator between excessive daytime sleepiness and sleep quality (psychological consequence) and between excessive daytime sleepiness and health behaviors as proposed by Peeters et al. (2008) in a study with children. Sleep habits were considered an internal resource and coping strategies were assessed through family sleep behaviors. Based on the lack of studies addressing adolescents’ sleep behaviors, the present study was focused on: (1) adolescents’ age and gender differences regarding anxiety and depression symptoms, excessive daytime sleepiness, family sleep behaviors, health behaviors, and sleep quality, (2) the contributions of adolescents and families’ socio-demographic characteristics regarding sleep quality and adolescents’ health behaviors, and (3) the moderator role of adolescents’ age and gender in the relationship between excessive daytime sleepiness and sleep quality. We hypothesized that: H1) there will be differences according to gender and age, with girls reporting worse anxiety and depression symptoms, more excessive daytime sleepiness, worse family sleep behaviors, worse sleep habits and worse sleep quality, and older adolescents reporting worse anxiety and depression symptoms, more excessive daytime sleepiness, worse family sleep behaviors, worse sleep habits, and worse sleep quality; H2) being female, an older adolescent reporting more anxiety and depression symptoms, poor sleep habits, the presence of excessive daytime sleepiness and poor family sleep behaviors will contribute to less health behaviors and poor sleep quality; and H3) gender and age will moderate the relationship between the presence of excessive daytime sleepiness and worse quality of sleep. Knowing the variables that are associated with health behaviors and sleep quality in adolescents will help to tailor interventions to improve sleep quality and promote healthy behaviors in adolescents, taking into consideration gender and age. Participants Two hundred and seventy-two school-going adolescents aged between 12 and 18 years old with a mean age of 15 years old (M = 15.48, SD = 1.61) participated in the study. Most participants were girls (58%), Caucasian (90%), and consumed 1-2 cups of coffee/day (29%). Most adolescents had parents consuming alcohol (73% fathers and 51% mothers) and tobacco (30% fathers and 15% mothers). Family members with sleep problems were reported by 35% of the sample. Measures Sociodemographic Questionnaire This questionnaire was developed to access characteristics of adolescents regarding age, gender, and educational level, parents use of alcohol and tobacco, adolescents’ consumption of caffeine products (more than 1/2 cups per day), and adolescents’ knowledge about drugs. Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989) This instrument assesses sleep quality in the previous month and includes 19 items (e.g., “Wake up in the middle of the night or early morning”). The PSQI has seven components that evaluate daytime dysfunction, sleep medication, sleep disturbances, sleep efficiency, sleep duration, sleep latency, and sleep quality. Scores range between 0 and 21 points and higher scores indicate worse sleep quality. Cronbach’s alpha for the total scale was .83 in the original version, and .60 in the present study. Since this instrument assessed different facets of adolescents’ sleep quality (e.g. daytime dysfunction, sleep medication, sleep latency, and sleep efficiency), Cronbach alpha may be modest (Taber, 2018). However, due to the clinical importance of this instrument and the fact that .60 is considered acceptable under certain circumstances (e.g., validating a new scale) (Taber, 2018), the authors decided to include the scale in the hypothesis testing. Sleep Habits Questionnaire (SHQ; Billings & Berg-Cross, 2010a) This 12-item questionnaire assesses the impact of behaviors that may influence sleep, in adolescents in a Likert type scale from 0 to 7 regarding the frequency of week days the behavior happens and how long the behavior takes place ( ≤ 15 min.; 1 hour; 1 ½ hour; ≥ 2 hours (e.g. “How many times a week do you play video-games after bedtime?” and “How long did you spend on that activity?”). The questionnaire includes information about weekend and weekday variations in sleep duration and scheduling, as well as questions about the perceived need for sleep and desired wake times. The sum of the responses indicates the sleep competing activity score. Scores range from 0 to 84 with higher scores indicate greater interference with sleep. Cronbach’s alpha was .65 in the original version and .70 in the present study. Modified Excessive Sleepiness Scale (MESSA; Billings & Berg-Cross, 2010b) The instrument is a modified version of the ESS (Epworth Sleepiness Scale) assessing the propensity of adolescents to fall asleep in different situations and is composed of 13 items (e.g., “For each situation, decide whether or not you would have: watched TV”). The scores range between 0 and 39 and a higher score indicates the presence of excessive daytime sleepiness. The author does not report the value of the Cronbach’s alpha. In this study, the Cronbach’s alpha for the total scale was .78. Hospital Anxiety and Depression Scales (HADS; Zigmond, & Snaith, 1983) The instrument assesses depression and anxiety symptoms (e.g., “I still enjoy the things I used to enjoy”). The instrument includes 14 items organized into two subscales (7 items for each subscale) and a global score assessed in a 4- point Likert type scale (0 to 3). The cutoff score for clinical depression and anxiety is 8 for both scales. The score in both subscales ranges between 0 and 21 and between 0 and 42, in the global scale. A high score indicates more symptomology. Cronbach’s alpha for the total scale was .80, in the original version and .76 in the present study. Health Behavior Questionnaire (HBQ; Pereira, & Pedras, 2009) The 24-item instrument assesses health behaviors in 4-point Likert type scale from never (0) to everyday (4) (e.g., How often do you do the following behaviors: exercising, having a good meal with vegetables and fruits, doing a general checkup once a year). A higher score indicates the use of more healthy behaviors. Cronbach’s alpha was .82, in the original version, and .70 in the present study. Howard Family Sleep Questionnaire (HFSQ; Billings et al., 2010) This scale assesses the impact of family dynamics on sleep behavior and includes 52 items that assess physical and cultural aspects of the family environment that influence sleep (e.g., “We respect each other’s needs for quiet once one of us goes to bed”). The scores range between 24 and 120 and a higher score indicates poor sleep behaviors. In the original version, Cronbach’s alpha for the total scale was .81, and in this study was .70. Procedure Adolescents’ participation was voluntary and anonymous. After the approval of the Portuguese General Education Committee, the study was also approved by the directive board of each school. Data collection took place in two public high schools in the Northern region of Portugal. Previously, parents signed an informed consent regarding the students’ participation. Participants answered the instruments in the presence of one of the researchers during one of their classes, after teacher’s approval. Data Analysis In order to analyze the differences in sleep quality, excessive daytime sleepiness, family sleep behaviors, anxiety and depression symptoms, health behaviors, and sleep habits according to gender and age, hpsthps-tests were conducted. The variable age was categorized: 12-14 and 15-18 years old. To analyze the variables that contributed to health behaviors and sleep quality, hierarchical regressions were performed (enter method). In both regressions, socio-demographic variables (gender, fathers and mothers’ alcohol consumption, fathers’ and mothers’ smoking, family members with sleep problems, coffee intake, caffeinated sodas, energy drinks intake) were included in block 1, and in block 2 psychological variables (anxiety and depression symptoms, excessive daytime sleepiness, sleep quality and family sleep behaviors) were added. Multicollinearity was assessed (VIF < 1) (Daoud, 2017). To apply the moderated moderation model of adolescents’ gender and age in the relationship between excessive daytime sleepiness and sleep quality, the Macro Process for SPSS was used. The model was significant if both the two-interaction and the three-way interaction were significant (p < .05) and if the 95% bias corrected confidence intervals (95% CI), determined through the bootstrapped technique, did not include zero. For a more precise probe of the three-way interaction between excessive daytime sleepiness and adolescent’s gender and age, the Johnson-Neyman technique was employed to identify the significant regions of the moderated moderation (Hayes, 2013). The sample included 272 adolescents. Of the total sample, 60% were girls, Caucasian (92%), with parents being married (79%), reporting no sleep problem (65%). Fathers (74%) and mothers (52%) were alcohol consumers. The average caffeine intake (measured in number of cups) by adolescents was 4.20 (SD = 1.31) and 62% of adolescents between 16 and 18 years old consumed caffeine compared to younger adolescents (12-15 years old). Differences in Health Behavior, Anxiety and Depression Symptoms, Excessive Daytime Sleepiness, Sleep Quality, Family Sleep Behaviors, and Sleep Habits According to Gender and Age The results revealed significant differences between boys and girls on sleep quality. Female adolescents showed poorer sleep quality. No other differences were found in the remaining variables. Older adolescents (15-18 years old) showed healthier behaviors and worst sleep quality when compared to younger adolescents (12-14 years old). Younger adolescents reported poor sleep habits (Table 1). Contributors to Health Behaviors According to the final model, having a father that drinks alcohol, anxiety and depression symptoms as well as family sleep behavior contributed to poor health behaviors in adolescents. The regression model explained 11% of the variance (Table 2). Table 2 Differences on Psychological Variables according to Adolescents’ Gender and Age  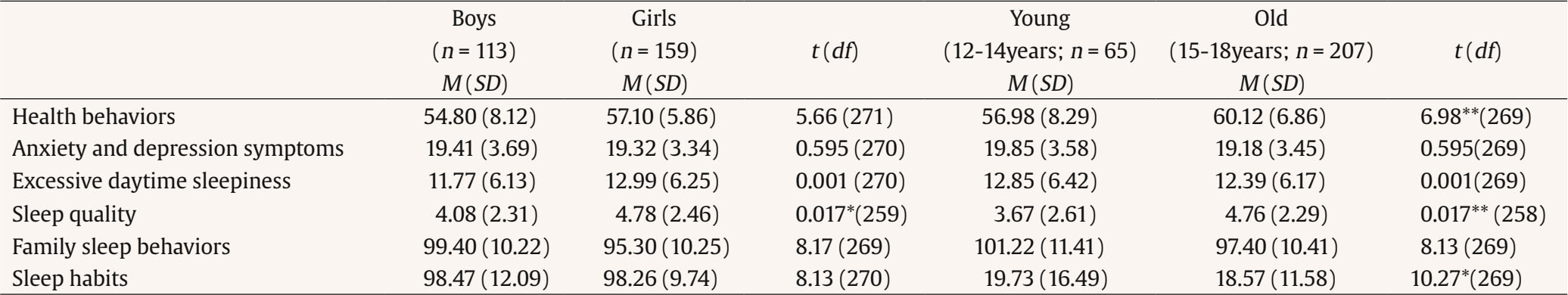 *p < .05, **p < .01, ***p < .001. Contributors to Sleep Quality The results of the final model showed that gender (female), having someone in the family with sleep problems and drinking 1-2 cups of coffee per day, more anxiety and depression symptoms, poor family sleep behaviors and the presence of excessive daytime sleepiness were contributors to poor sleep quality. The regression model explained 21% of the variance (Table 2). Adolescents’ Gender and Age as Moderators in the Relationship between Excessive Daytime Sleepiness and Sleep Quality The moderating effect of adolescents’ gender in the relationship between excessive daytime sleepiness and sleep quality was significantly moderated by adolescents’ age. The overall moderated moderation model explained 14.3% of the variance, F(7, 263) = 6.284, p < .001. All two-way interactions, i.e., Excessive Daytime Sleepiness x Gender (β = -1.068, SE = .403, p = .009), Excessive Daytime Sleepiness x Age (β = -.060, SE = .020, p = .004) and Gender x Age (β = -1.056, SE = .371, p = .005) were negatively significant. The three-way interaction Excessive Daytime Sleepiness x Gender x Age was positively significant (β = .072, SE = .026, p = .006). Therefore, being a girl and an older adolescent moderated the relationship between the presence of excessive daytime sleepiness and worse sleep quality. The Johnson-Neyman technique showed that the moderated moderation was significant when Ď´XM→Y = 16.254 or greater, with 28.78% of the adolescents’ age values producing a moderated moderation (Table 3 and Figure 1). Table 3 Predictors of Health Behaviors and Sleep Quality (Final Model)  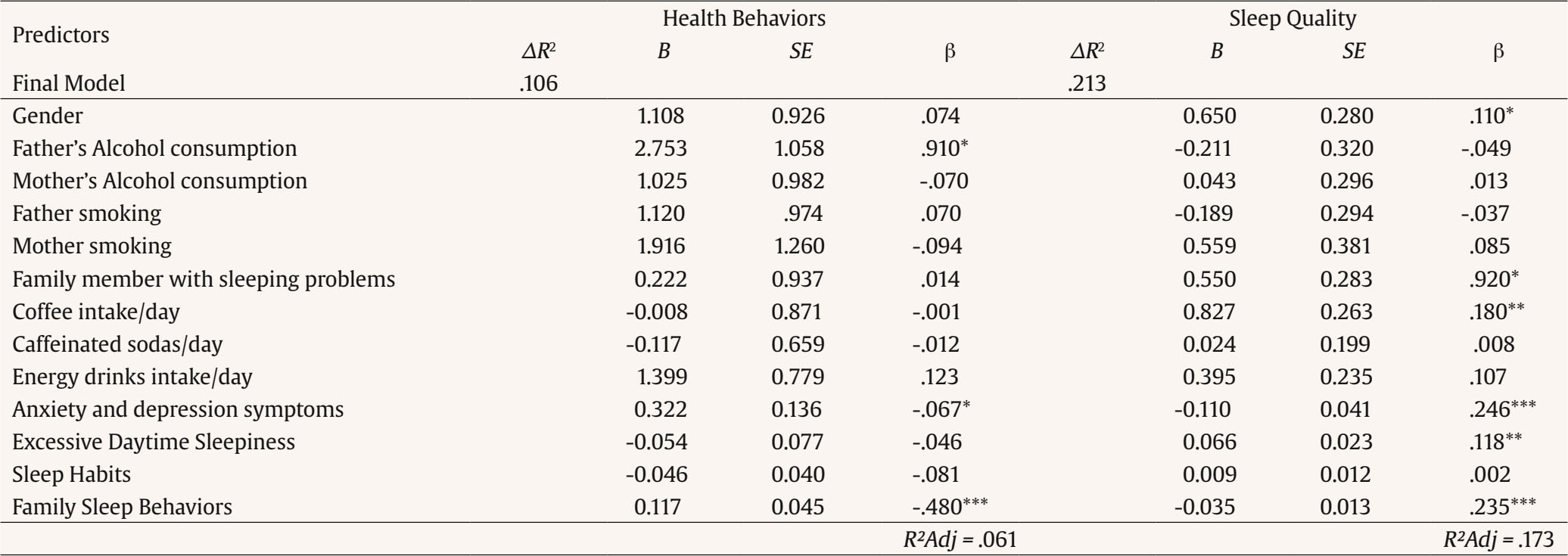 *p < .05, **p < .01, ***p < .001. Figure 1 The Moderated Moderation Effect of Adolescents’ Gender and Age in the Relationship between Excessive Daytime Sleepiness and Sleep Quality.  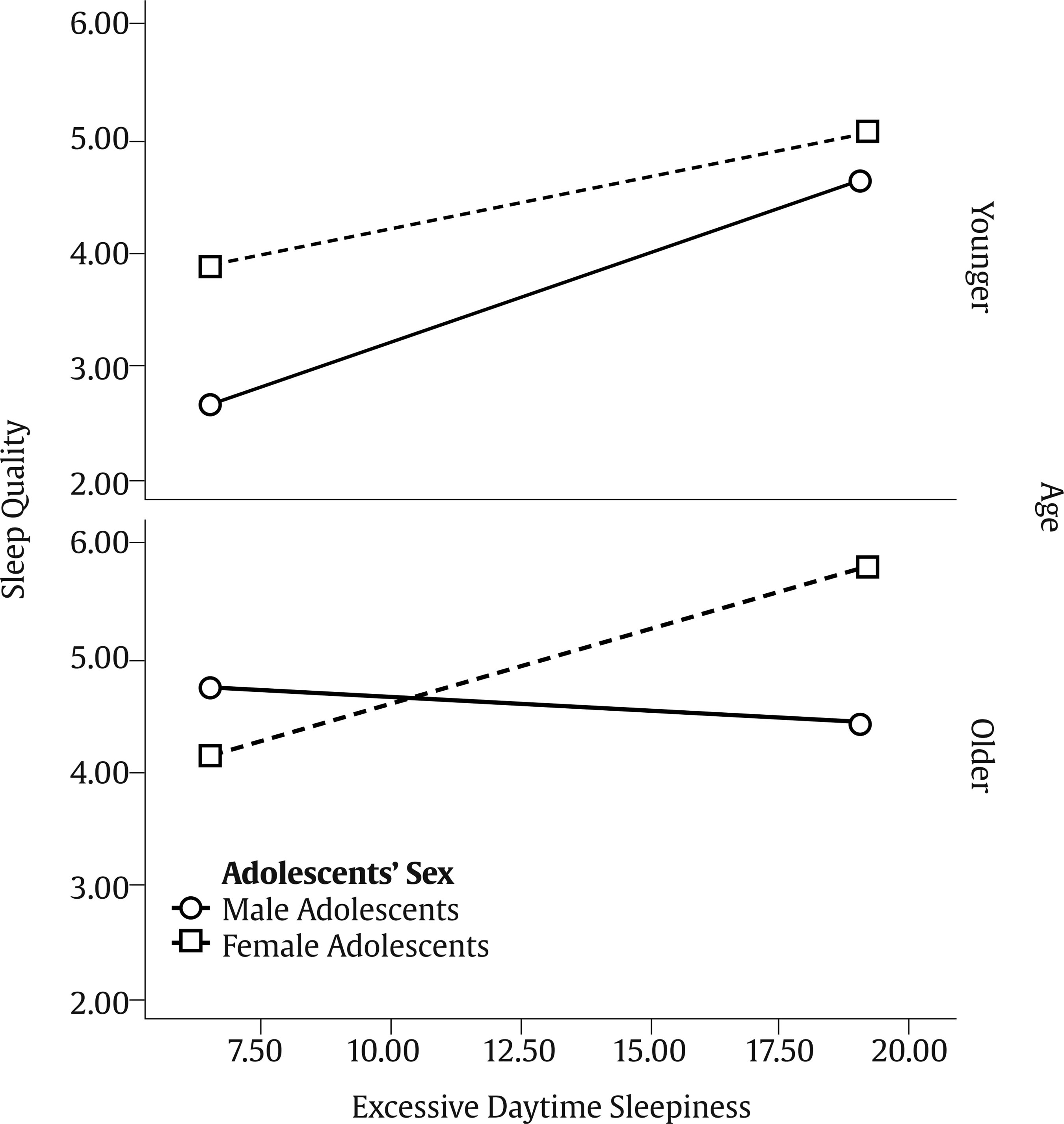 According to the results, girls showed worse sleep quality, which partially confirmed H1. An epidemiological study with adolescents found that girls showed major risks for insomnia compared to boys (Tang et al., 2017). Another study with 131 young boys and girls found that most of the girls had poor sleep (de Zambotti et al., 2018). The differences found in sleep problems between genders may be explained by the increased number of girls in pubertal status in most studies, i.e., the results are influenced by participants’ age (de Zambotti et al., 2018). Younger adolescents (12-14 years old) reported poorer family sleeping habits than older ones (15-18 years old). In fact, the family environment is an important factor to be considered concerning sleep in adolescents (Gunn et al., 2019). Family disorganization can be a source of poor sleep practice in young adolescents (for example, using computer at night in bed to relax) and may inhibit good practices of sleep hygiene (Gunn et al., 2019). Older adolescents showed healthier behaviors, but worse sleep quality when compared to younger adolescents. In fact, younger adolescents show a higher chance of being high-risk internet users than older adolescents and this behavior is associated with other unhealthy behaviors, such as the use of psychoactive substances (alcohol, tobacco) and inadequate diet (Lemola et al., 2015). Older adolescents also went to bed later and, consequently, they got less sleep than younger adolescents (Gradisar et al., 2011). The results of the present study also showed that gender, family sleep problems, drinking coffee, anxiety and depression symptoms, family sleep behaviors and excessive daytime sleepiness contributed to sleep quality. Being a girl, having someone in the family with sleep problems, drinking 1-2 cups of coffee per day, reporting more anxiety and depression symptoms and poor family sleep behaviors, as well as the presence of excessive daytime sleepiness contributed to poor sleep quality, confirming H2. The literature found similar results about gender-related differences regarding sleep, indicating a major susceptibility of girls that showed more profound effects of insufficient sleep (variable that impacts sleep quality) than boys (Tang et al., 2017). Moreover, adolescents’ habits, e.g., coffee intake, was found to contribute to sleep quality. Caffeine is characterized as a stimulant psychoactive substance that may impact sleep quality (Calamaro et al., 2009). Previous research regarding adolescents showed that caffeine intake and use of electronic equipment before bedtime changed the overall functionality of the adolescent, which in turn caused excessive daytime sleepiness (Lemola et al., 2015). Also, Hoelfelmann et al. (2015) in their study about the association between unhealthy behaviors and sleep quality in adolescents found that the use of computer/video games during more than 4 hours per day, an excessive consumption of alcoholic beverages, and eating salty or sweet snacks more than 5 days per week were related to negative sleep quality. Instead, physical activity was found to be a protective factor against sleep difficulties, been consistently associated with better sleep quality (Foti et al, 2011). In the present study, excessive daytime sleepiness contributed to sleep quality. In fact, other study concluded that different variables (e.g., insomnia symptoms, perceived sleep insufficiency, and apnea) were associated with excessive daytime sleepiness among adolescents (Calamaro et al., 2009). Furthermore, having a family member with sleep problems also contributed to sleep quality. Parents’ influence may explain behavior alterations and sleep problems (Gunn et al., 2019). In the present study, family sleep behavior contributed to adolescents’ sleep quality. Family environment is an important factor related to sleep in adolescents, but there are few studies that analyze the relationship between family functioning and adolescent sleep (Khor et al., 2021; Machado et al., 2020). One of these few studies found that family stress works as a predictor of sleep disturbances (Bernert et al., 2007). Adolescents’ sleep may be affected by family functioning, but more research regarding this topic is needed (Machado et al., 2020). In turn, poor sleep hygiene practices were associated with adolescents’ poor sleep (Crowley et al., 2018). Behavioral treatments that include adolescents and parents’ sleep practices seem to improve family sleep as a whole and should, therefore, be a major concern for health professionals (Machado et al., 2020). Furthermore, depression and anxiety were two other contributors towards sleep quality. Da and Kutlu (2017) studied the relationship between sleep quality and depressive symptoms and found that moderate to severe depressive symptoms, tobacco use, and having a family member with sleep problems were related to poor sleep quality in adolescents. Table 4 Regression Analysis of Moderated Moderation for Quality of Sleep and Conditional Effects of Excessive Daytime Sleepiness at Values of Adolescents’ Gender and Age (moderators)  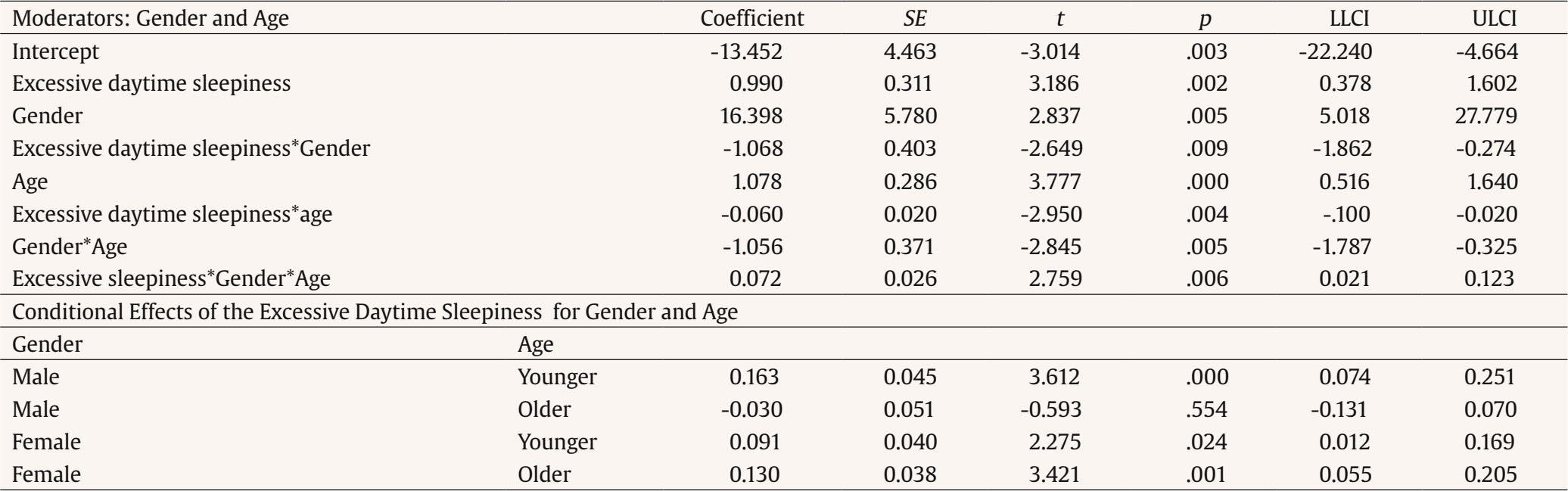 Father’s alcohol consumption was a contributor of health behaviors in adolescents. The impact of parents’ consumption on adolescents’ health has been found in the literature (Kansagra, 2020). In a study that examined the relationship between parents’ consumption of alcohol and adolescents’ health behaviors, parental alcoholism predicted changes in health behaviors in adolescents, i.e., young adolescents whose parents drank alcohol reported more alcohol abuse and developed alcohol dependence (Raitasalo et al., 2019). Also, unhealthy behaviors in adolescence may have a negative impact on adolescents’ comorbidities (anxiety and depression symptoms). The present study found that adolescent anxiety and depression symptoms contributed to health behaviors. A longitudinal study, that analyzed depressive symptoms and health risk behaviors in approximately 4,400 adolescents, concluded that adolescents with higher levels of depressive symptoms reported a major use of psychoactive substances (Hooshmand et al., 2012). Family sleep behaviors contributed to health behaviors in adolescents. This is an interesting result, since family habits may be manageable to change and, therefore, contribute to promote healthy sleep habits in adolescents. A study with pre-adolescents (10-11 years) found that family characteristics such as family meals and being less time alone were predictors of positive changes in lifestyle-related health behaviors (Gunn et al., 2019). Since the model only explained 10% of the variance, there are several factors that account for health behaviors in adolescents. Being a girl and an older adolescent moderated the relationship between the presence of excessive daytime sleepiness and poor sleep quality, which confirmed the last hypothesis of this study. Literature revealed an important gap in the knowledge of the influence of adolescents’ gender and age on sleep outcomes, such as daytime sleepiness and sleep quality (Blake et al., 2018; Lewien et al., 2021). However, Maes et al.’s (1996) Stress-Coping Model recognizes that sociodemographic characteristics, as adolescents’ gender and age, and disease characteristics (excessive daytime sleepiness) may influence sleep quality (psychological consequence) as our model of moderated moderation found. Also, in Jahrami et al.’s (2019) study, age and gender were not significant moderators both on sleep quality and excessive daytime sleepiness and the authors, hypothesized that the developmental variation between male and female young adults could explain the absence of the effect of gender and age on the relationship between daytime sleepiness and sleep quality. Some studies did not find any difference in adolescents’ gender and age in the relationship between sleep quality and internalizing symptoms, as anxiety and depression (Rubens et al., 2017). However, being a male and a young adolescent influenced the relationship between poor sleep quality and impulsivity behaviors (Rubens et al, 2017), emphasizing the need to explore the developmental mechanisms that may influence poor sleep quality and adolescents’ behaviors beyond heath behaviors. Implications for Practice According to the results, it is important that health professionals screen anxiety and depression symptoms as well as sleep habits in routine consultations to prevent adolescents’ sleep problems. Results also showed the importance to organize intervention programs according to adolescents’ gender and age, since female adolescents and older adolescents seem to present more sleep difficulties and have different needs that should be addressed. Also, the assessment of adolescent and family’s health behaviors that interfere with sleep should also be targeted. Families and teachers should be trained to early recognize important changes in the adolescents’ behaviors such as excessive daytime sleepiness that may compromise the adolescent performance in school and refer the adolescent and the family to a multidisciplinary healthcare team. Schools also have an important role in promoting adolescents’ mental and physical health, contributing to adolescents’ lifestyle and, as a result, should be part of the solution and contribute to a decrease of the current epidemiology of sleep problems, in this population. Limitations The main limitations of this study were the use of self-report measures and the cross-sectional design that does not allow causal relationships between the variables under study. Furthermore, the data were collected in two public high schools in the northern region of Portugal, so further studies should use a bigger sample from different public and private schools and different regions of the country. Future research should employ a longitudinal design to find which variables, in early adolescence, predict health behaviors and sleep quality over time, as the adolescent grows older into early adulthood. Also, future longitudinal studies should assess if parents’ sleep problems mediate the relationship between adolescents’ sleep problems and sleep quality since sleep behavior seems to be part of the family dynamics. As such, the parent-adolescent dyad should be assessed on sleep quality over time to determine how much they both influence each other. Conclusion The current study emphasized the importance of anxiety and depression symptoms, excessive daytime sleepiness, family sleep behavior, and sleep quality in adolescents. Girls and older adolescents reported poorer sleep quality. Anxiety and depression symptoms were also an important factor regarding adolescents’ health, contributing to sleep quality and health behaviors. This study found that family sleep behaviors contributed to adolescents’ health behaviors and sleep quality, emphasizing the importance of the family and the need to integrate the latter in intervention programs. According to results, health promotion interventions for adolescents should also be developed for each specific age group considering the adolescent maturation phase. Conflict of Interest The authors of this article declare no conflict of interest. Authors’ Contribution Silvia Pucci was involved in literature review, data collection and data analysis, Ana C. Almeida was involved in data analysis, and data interpretation, and M. Graça Pereira developed the study design and was involved in data analysis, data curation, data interpretation, and critical revision of the paper. All authors were involved in writing the draft of the manuscript. Cite this article as: Pucci, S., Almeida, A. C., & Pereira, M. G. (2024). Health behaviors and sleep quality in Portuguese adolescents: The moderating role of age and gender. Clínica y Salud, 35(1), 5-12. https://doi.org/10.5093/clysa2024a9 Funding: The present research was supported by Erasmus Mundus 15. Ref: 2099-1670/001-001-ECW to the first author. This study was conducted at the Psychology Research Centre (PSI/01662), School of Psychology, University of Minho, supported by the Foundation for Science and Technology (FCT) through the Portuguese State Budget (Ref. UIDB/ PSI/01662/2020). References |
Cite this article as: Pucci, S., Almeida, A. C., & Pereira, M. G. (2024). Health Behaviors and Sleep Quality in Portuguese Adolescents: The Moderating Role of Age and Gender. ClĂnica y Salud, 35(1), 5 - 12. https://doi.org/10.5093/clysa2024a9
Correspondence: gracep@psi.uminho.pt (M. Graça Pereira).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







