
Differential Outcome of a Therapeutic Community Program for Internalizing and Externalizing Personality Disorders: A Change in Cognitive Processes Mediates Symptom Improvement
[Eficacia diferencial para internalizadores y externalizadores de un programa de comunidad terapéutica para trastornos de personalidad]
Juan M. Ramos, Aintzane Sánchez, and Aurora Doll
Hospital Dr. R. Lafora, Unidad de Trastornos de la Personalidad, Madrid, España
https://doi.org/10.5093/clysa2020a3
Received 25 September 2019, Accepted 3 December 2019
Abstract
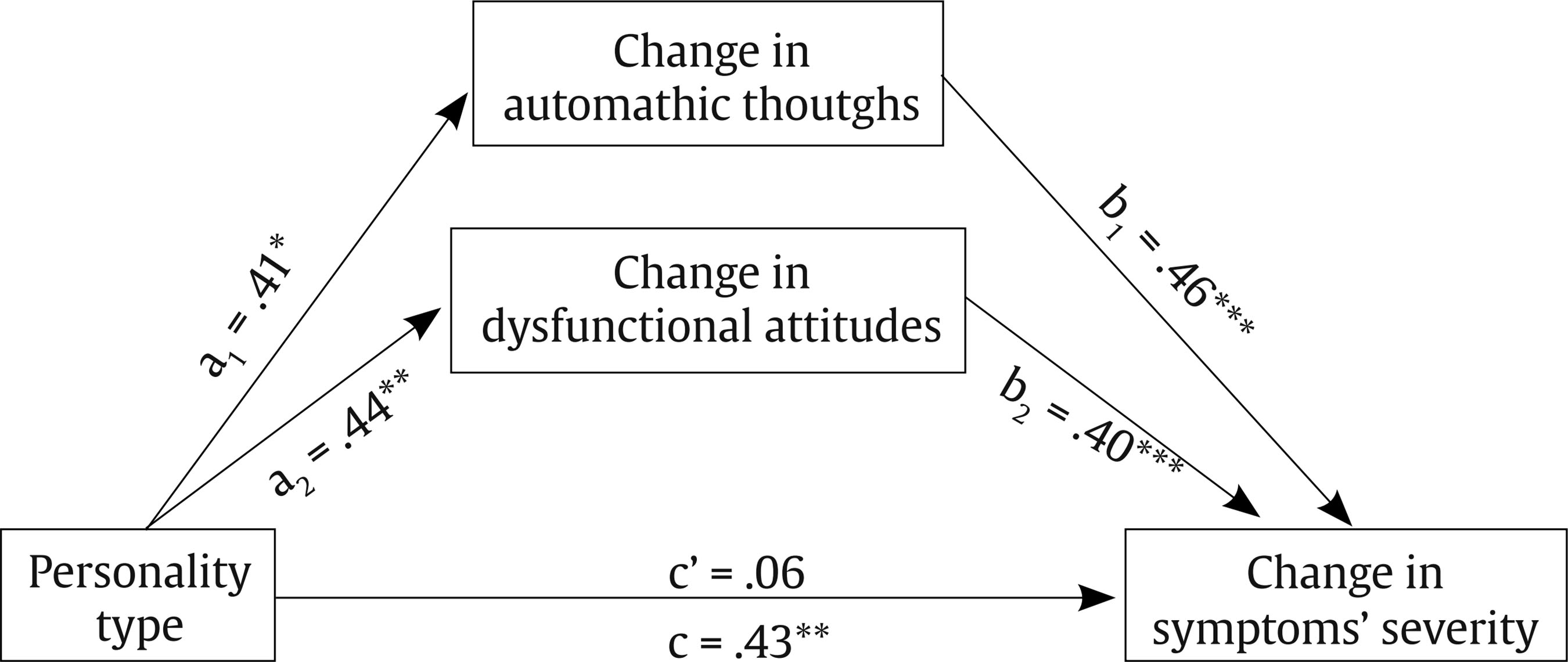
The identification of transdiagnostic mediating processes involved in a therapeutic change and their relationship with personality can contribute to a better adjustment of a therapeutic technique, enhancing its effectiveness. In a sample of 158 adults diagnosed with personality disorder who complete an inpatient therapeutic community program for 6 months, the hypothesis of a differential reduction in symptom intensity according to the externalizer/internalizer typology is tested, and cognitive variables mediating change are explored. A pre-post change (p = .000, ηp2 = .50) is observed, along with a difference between externalizers and internalizers (p = .002, ηp2 = .06), and an interaction effect (p = .037, ηp2 = .03). The effect of personality type on symptom change (β = .43, p = .009) is no longer significant when negative automatic thoughts and dysfunctional attitudes are considered as mediators (β = .06, p = .549). Findings are discussed from the perspective of personality disorder as a vulnerability factor.
Resumen
La identificación de procesos mediadores transdiagnósticos intervinientes en el cambio terapéutico y su relación con la personalidad puede contribuir a un mejor ajuste de la técnica terapéutica, potenciando su eficacia. En una muestra de 158 adultos diagnosticados de trastorno de personalidad inscritos en un programa de comunidad terapéutica hospitalaria durante 6 meses se pone a prueba la hipótesis de una reducción diferencial de laintensidad sintomatológica según la tipología externalizador/internalizador y se exploran las variables cognitivas mediadoras del cambio. Se observa un cambio pre-post (p = .000, ηp2 = .50), la diferencia entre externalizadores e internalizadores (p = .002, ηp2 = .06) y el efecto de interacción (p = .037, ηp2 = .03). El efecto del tipo de personalidad sobre el cambio en los síntomas (β = .43, p = .009) deja de ser significativo cuando se consideran los pensamientos automáticos negativos y las actitudes disfuncionales (β = .06, p = .549) como mediadores. Se discuten los resultados desde la perspectiva del trastorno de personalidad como factor de vulnerabilidad.
Palabras clave
Trastorno de personalidad, Comunidad terapéutica, Cambio terapéutico, Procesos cognitivos, Análisis de mediaciónKeywords
Personality disorder, Therapeutic community, Therapeutic change, Cognitive processes, Mediation analysisCite this article as: Ramos, J. M., Sánchez, A., & Doll, A. (2020). Differential Outcome of a Therapeutic Community Program for Internalizing and Externalizing Personality Disorders: A Change in Cognitive Processes Mediates Symptom Improvement. ClÃnica y Salud, 31(1), 47 - 53. https://doi.org/10.5093/clysa2020a3
jmramos@cop.es Correspondence: jmramos@cop.es (J. M. Ramos).Specific intervention programs developed to date for personality disorders (PD) show limited results (Cristea et al., 2017; Stoffers et al., 2012). But the search for transdiagnostic processes is spreading knowledge and clinical efficiency (Rodriguez-Seijas, Eaton, & Krueger, 2015). Various transdiagnostic mechanisms of change have been postulated from different theoretical positions in order to explain patients’ improvement: reflexive function or epistemic trust (Fonagy, Luyten, & Allison, 2015), integration of representations of the self and others and affective regulation (Levy et al., 2006), mindfulness, validation and interpersonal effectiveness (Lynch, Chapman, Rosenthal, Kuo, & Linehan, 2006), dysfunctional beliefs (Davidson et al., 2006), early schemes (Kellogg & Young, 2006), social cognition (Jennings, Hulbert, Jackson, & Chanen, 2012), and experiential avoidance (Iverson, Follette, Pistorello, & Fruzzetti, 2012). But “we have very limited knowledge about the moderators and mechanisms of change in psychotherapy” (Bateman, Campbell, Luyten, & Fonagy, 2018, p. 44). Dimaggio and Livesley (2012) suggest an integrated approach that combines empirically supported strategies and techniques. The characteristics shared by effective treatments have been pointed out: a responsible clinician within a multiprofessional team, an expressly accepted therapeutic structure that clarifies roles and procedures, a validation of the patient that integrates acceptance of difficulties and support for the commitment to change, a personal involvement of the patient as an active agent, and a continuous self-critical supervision of therapeutic interaction. Bateman et al. (2018) summarize the crucial aspects of effective therapies for PD in three words: coherence, consistency, and continuity. The therapeutic community methodology offers a particularly powerful intervention framework for the integration of these elements. Its effectiveness is being demonstrated, and therefore its indication has been strengthened in expert guides. Pearce and Pickard (2013) highlighted two specific factors shared by different therapeutic communities that can explain the important therapeutic effect they achieve: promotion of a sense of belonging and empowerment of personal responsibility. Although both factors occur to varying degrees in different approaches and interventions, their emphasis and combination are distinctive in the therapeutic community model, maximizing the chance of change. In a previous paper (Ramos, Sendra, Sánchez, Mena, & Rodríguez, 2017) we examined the efficacy of an intervention based on the therapeutic community model for in-patients with severe personality disorder, observing a significant symptom improvement (Cohen’s d = 1.19) and a moderate decrease of PD severity (d = 0.75) in the group of adherents similar to the results achieved by other specialized programs. Typology features related to change were obtained considering the scales of the MCMI-II, non participants’ individual profile. By taking scales as unit of analysis, interpretation of findings is disfigured: each person is characterized by a particular constellation of features that draws on the score of all scales. One way to overcome this limitation is to identify categories that classify people (not dimensions or traits) in an exhaustive and exclusive way, so that differences in a dependent variable can be attributed to differences in real people, not in dissected traits. In fact, in a recent work (Ramos, Broco, Sánchez, & Doll, 2019), using a methodology of cluster and discriminant analyses, we found a typology of two exclusive groups that classified all the patients in our sample, namely internalizing vs. externalizing. The present study follows the above mentioned studies, with two main goals. Firstly, to test the hypothesis of a differential effectiveness of the intervention program according to the externalizing/internalizing typology. Secondly, to identify some mediating cognitive variables that can explain, in a proximal way, the distal effect of personality type on symptom improvement after treatment. Within the framework of PD as a general vulnerability factor (Tyrer, 2007), it is assumed that pathological personality would be related distally to symptomatology through proximal mediating and modulating processes. The identification of processes involved in change and their relationship with personality variables can contribute to the clarification of some of the psychological mechanisms that enhance a treatment’s efficacy and, consequently, it can help to a better adjustment of the therapeutic technique to an individual’s profile (Hayes et al., 2019). Participants The sample is composed of PD diagnosed adults who successively enter a PD Unit to participate voluntarily in a hospital intervention program (N = 310). All subjects meet severe PD criteria. Their age ranges from 18 to 58 years (M = 35.7, SD = 8.6); the majority are women (79.4%), single (66.2%), living with a family member (80%), without home ownership (55.5%). Their employment status is unemployment (61.6%), temporary disability (24.4%) or permanent disability (14%); 38.4% have a certified degree of disability (from 33% to 81%). Only 13.1% have university education. Diagnosed with BPD there were 59.7%, not specified PD (20.6%), and mixed PD (17.1%); 60.6% remain in the program (N = 188); of these, 30 do not satisfactorily complete pre- and post-measurements, so the final sample on which analyses are performed consists of N = 158 participants. Instruments and Procedure After signing a therapeutic contract, participants join the 6-month multi-professional treatment program inspired by the therapeutic community model. All participants give their written consent and receive in the first week (pre measure) and in the last fortnight of hospital admission (post measure) a battery of self-reporting instruments from which data are obtained for this research, which complies with the ethical and legal guidelines of the institution where it is conducted. The instruments selected for this research were the following ones. Millon Clinical Multiaxial Inventory_II (MCMI-II; Millon, 1999). It is a measure of personality and clinical syndromes. It consists of 175 items with dichotomous response (true/false) and provides a profile of 10 basic personality scales plus 3 severe pathological personality scales, as well as other clinical syndrome scales. Internal consistency is satisfactory (KR coefficients between .81 and .95); in our sample, the Cronbach’s alpha was .84. We define the personality disorder severity (PDS) variable as the summation of the scores on those 13 scales that exceed the base rate of 75. Symptom Checklist-90-Revised (SCL90-R; Derogatis, 2002). It evaluates a wide range of psychopathological characteristics (somatization, anxiety, depression, obsession-compulsion, interpersonal sensitivity, hostility, paranoid ideation, psychoticism). Participants evaluate how upset they were in the last few weeks for each of 90 symptoms on a Likert scale (0 to 4). It has 10 scales and three global indices. Its reliability is acceptable, with high internal consistency coefficients (α > .81) and test-retest values higher than .78. For this study, only the Global Severity Index (GSI) was used, which is a generalized and indiscriminate measure of the intensity of symptom distress. In our sample, Cronbach’s alpha was .97. General Self-Efficacy Scale (GSE; Schwarzer & Jerusalem, 1995; Spanish version by Schwarzer & Baessler, 1996). It evaluates a general sense of personal agency with 10 sentences rated from 1 to 4. Its reliability is acceptable, and internal consistency coefficients range from .79 to .93. In our sample, α = .88. Rosenberg Self-Esteem Scale (RSS; Rosenberg, 1989; Spanish version by Martín-Albo, Núñez, Navarro, & Grijalvo, 2007). It evaluates the sense of own worth with 10 sentences rated from 1 to 5. It shows adequate levels of reliability and validity (Martín-Albo et al., 2007). In our sample, α = .76. Social Skills Scale (EHS; Gismero, 2000). It evaluates perceived assertiveness and social skills through 33 sentences rated from 1 to 4 and structured in 6 scales. We use the overall score in this research. It has a Cronbach’s alpha reliability of .88. In our sample, α = .90. Dysfunctional Attitude Scales (DAS; Weissman y Beck, 1978; D. Burns version adapted to Spanish by Bas y Andrés, 1994). It evaluates cognitive schemes. It consists of 35 sentences with which an individual shows his/her degree of agreement between -2 (strongly agree) and +2 (strongly disagree), grouped into 7 scales whose scores range from -10 to +10 (a negative score is an indicator of vulnerability). The original version has adequate internal consistency (α = .89 to .92) and test-retest reliability (.84). For this research we use the inverted global score: the higher the score, the greater the attitudinal dysfunctionality (range between -70 and +70). In our sample, α = .93. Table 1 Mean Difference before and after Intervention (Student-t for repeated measures), with 95% Confidence Interval (CI) and Effect Size (Hedges’ g)  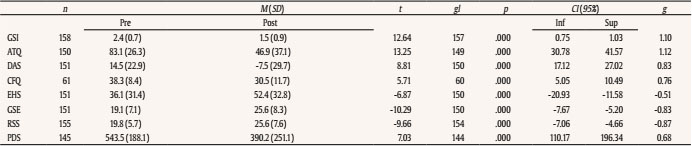 Note. ATQ = automatic thoughts; CFQ = Cognitive Fusion Questionnaire; DAS = Dysfunctional Attitudes Scales; GSE= General Self-Efficacy Scale; EHS = Social Skills Scale; GSI = Global Severity Index of the Symptom Checklist-90-Revised; PDS = Personality Disorder Severity; RSS = Rosenberg Self-esteem Scale. Cognitive Fusion Questionnaire (CFQ; Gillanders et al., 2014; Spanish version by Romero-Moreno, Márquez-González, Losada, Gillanders, & Fernández-Fernández, 2014). It evaluates the degree of identification with the literal content of thoughts. It consists of 7 sentences rated from 1 (never) to 7 (always). Higher scores reflect higher cognitive fusion. It has adequate reliability (α = .87 to .93), temporary stability, and convergent, divergent and discriminant validity, as well as sensitivity to change after treatment. In our sample, α = .89. Automatic Thoughts Questionnaire (ATQ; Hollon y Kendall, 1980; Spanish version by Cano-García & Rodríguez-Franco, 2002). It evaluates the frequency of undeliberated negative thoughts that emerge in the mind. It consists of a list of 30 items scored from 1 (never) to 5 (always), indicating higher frequency of negative thoughts at higher scores (between 30 and 150). The original internal consistency is .96. In our sample, α = .96. The design of the study is quasi-experimental and longitudinal: before and after treatment (independent variable) subjects took the General Severity Index (GSI from the SCL90-R), as dependent variable, to test differences in symptom severity between two groups of participants (PT, personality type): internalizers vs. externalizers. As mentioned earlier, this categorization was a result of applying cluster and discriminant analyses to the data obtained from the 13 personality scales of the MCMI-II (see Ramos et al., 2019 for details). Then, some cognitive processes were evaluated as putative mediating variables between personality type (PT, independent variable) and change in symptom severity (C-GSI, dependent variable) by means of mediation analyses. Data Analysis Differences between the group of adherents and non-adherents to the program were analyzed by means of χ2 and Student’s t-tests. Through a general linear model of repeated measures (GLM) we tested the first hypothesis that the type of personality (PT, internalizers vs. externalizers, between-subject factor) makes a difference in symptom severity (GSI of SCL90-R, dependent variable) before and after treatment (intra-subject factor). To test the second hypothesis of identifying some mediating cognitive variables that explain the distal effect of personality type on symptom change, we define change in each variable (CV) as the difference between pre- and post-measures in each instrument (CV = Vpre – Vpost); then, zero-order and partial correlations are obtained, taking change in symptom severity (C-GSI) as the control variable. Differences between internalizers and externalizers in average scores of each change variable – change in self-efficacy (C-GSE), self-esteem (C-RSS), perceived social skills (C-EHS), automatic thoughts (C-ATQ), dysfunctional attitudes (C-DAS), and cognitive fusion (C-CFQ) – are checked (Student’s t). Through a stepwise regression analysis, the variables whose change best explain the variance of change in symptom severity (C-GSI, criterion) were selected. Finally, a mediation model is proved with the PROCESS program (Hayes, 2018), taking type of personality (PT) as independent variable, change in cognitive processes (CV) as mediating variables, and change in severity of symptoms (C-GSI) as dependent variable. The direct effect of personality on symptom severity is compared with the indirect effect through the mediating variables. Confidence interval (95%) of the differences is calculated using the bootstrap technique, with 5,000 iterations; Finally, the indirect effect measured with the Sobel test was different from zero. We used qgraph package for R for graphical representation of the correlation network and SPSS Statistics v.22 program for analyses. Out of all the participants in the initial sample, 60.6% remained in the program (N = 188). There were no gender differences in adherence (χ2 = 1.43, p = .231), nor typology differences (χ2 = 0.01, p = .909): both externalizers and internalizers have a similar rate of adherence (.60 and .61, respectively). However, there are differences by age: those who leave are 2.5 years younger on average (t = -2.65, p = .008, 95% CI [-4.4, -0.6]). There are also differences in 3 personality scales of the MCMI-II: patients with premature discharge score higher on the antisocial scale (t = 2.39, p = .017, difference = 5.6, error = 2.34, 95% CI [0.99, 10.21]) and passive-aggressive scale (t = 2.70, p = .007, difference = 6.1, error = 2.25, 95% CI [1.64, 10.51]), and score lower on the obsessive-compulsive scale (t = -2.69, p = .007, difference = -7.5, error = 2.8, 95% CI [-13.03, -2.03]). Figure 1 Differences between Internalizers and Externalizers in the Personality Scales of the MCMI-II. To facilitate comparison, direct scores have been transformed into z-scores (M = 0, SD = 1) and have been ordered according to the magnitude of their differences.  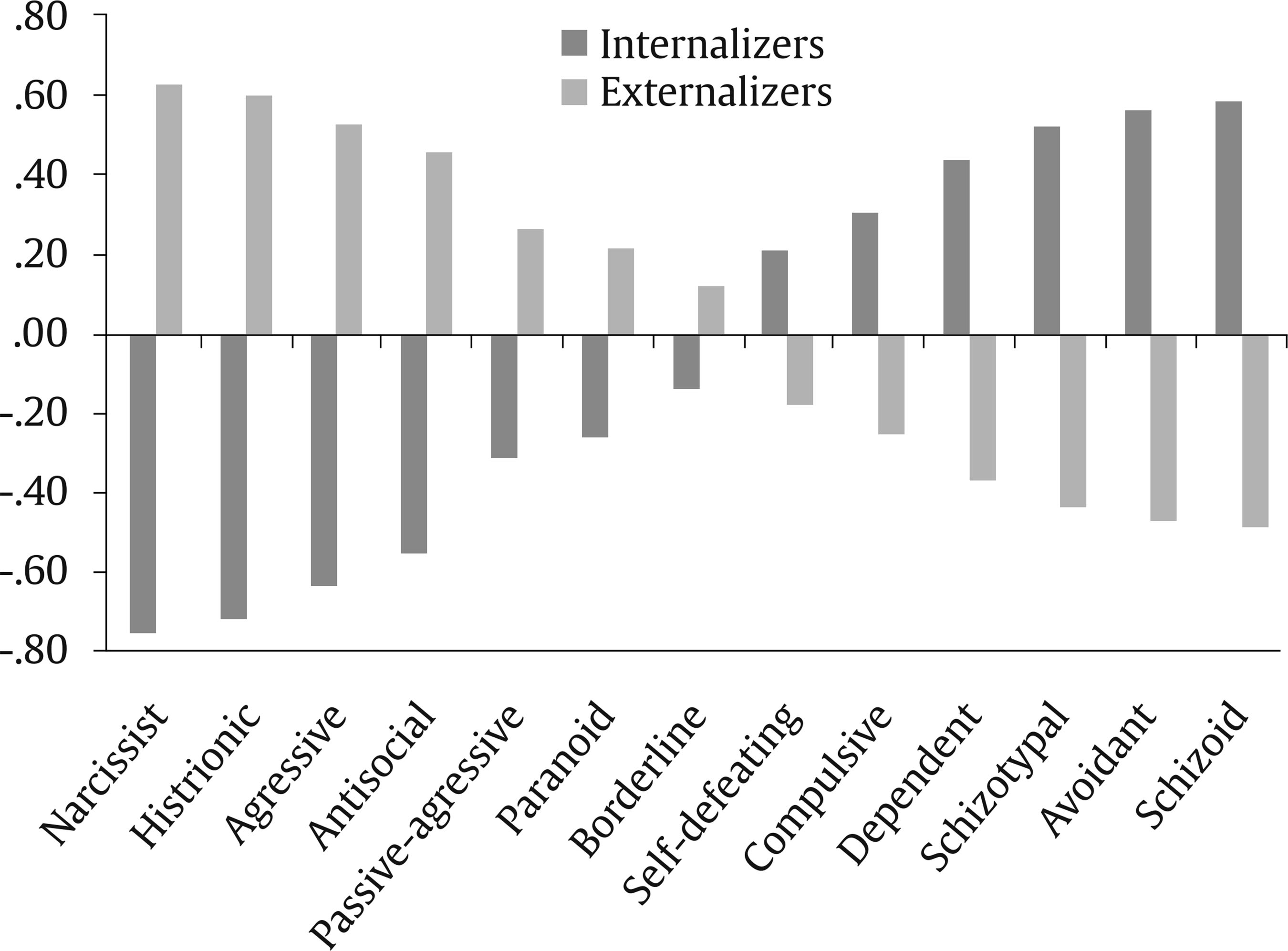 The difference between pre- and post-measures is significant in all variables, with effect sizes between moderate and large (Table 1). Table 2 Repeated Measures General Lineal Model. Intra-subjects Factor: Time (pre, post). Between-subjects Factor: Personality Type (INT, EXT). Dependent Variable: Symptom Severity (GSI del SCL90-R)  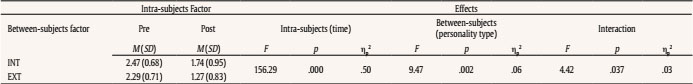 Note. GSI = Global Severity Index of the Symptom Checklist 90 Revised; INT = internalizers; EXT = externalizers. Externalizers (54.5%) differ from internalizers (45.5%) in all personality scales (p < .05). Figure 1 shows differences between both profiles; direct scores have been transformed into z-scores (M = 0, SD = 1) to facilitate comparison. The differential change observed between the beginning and the end of the program in the symptom severity variable (C-GSI) according to the type of personality is shown in Table 2 and Figure 2. Significance is observed in the intra-subject effect (difference between pre- and post-severity measure) (p = .000, ηp2 = .50), in the between-subject effect (difference between externalizers and internalizers) (p = .002, ηp2 = .06) and in the interaction effect between both (p = .037, ηp2 = .03). Externalizers obtain a greater reduction in symptom severity than internalizers (C-GSI: MINT = .73, SDINT = .92, MEXT = 1.03, SDEXT = .84, difference= -.30, t(156) = -2.10, p = .037, IC 95% [-0.57, -0.02]). Figure 2 Mean Scores in Severity of Symptoms (GSI del SCL90-R) before and after Intervention, according to Personality Type (INT = internalizers, EXT = externalizers).  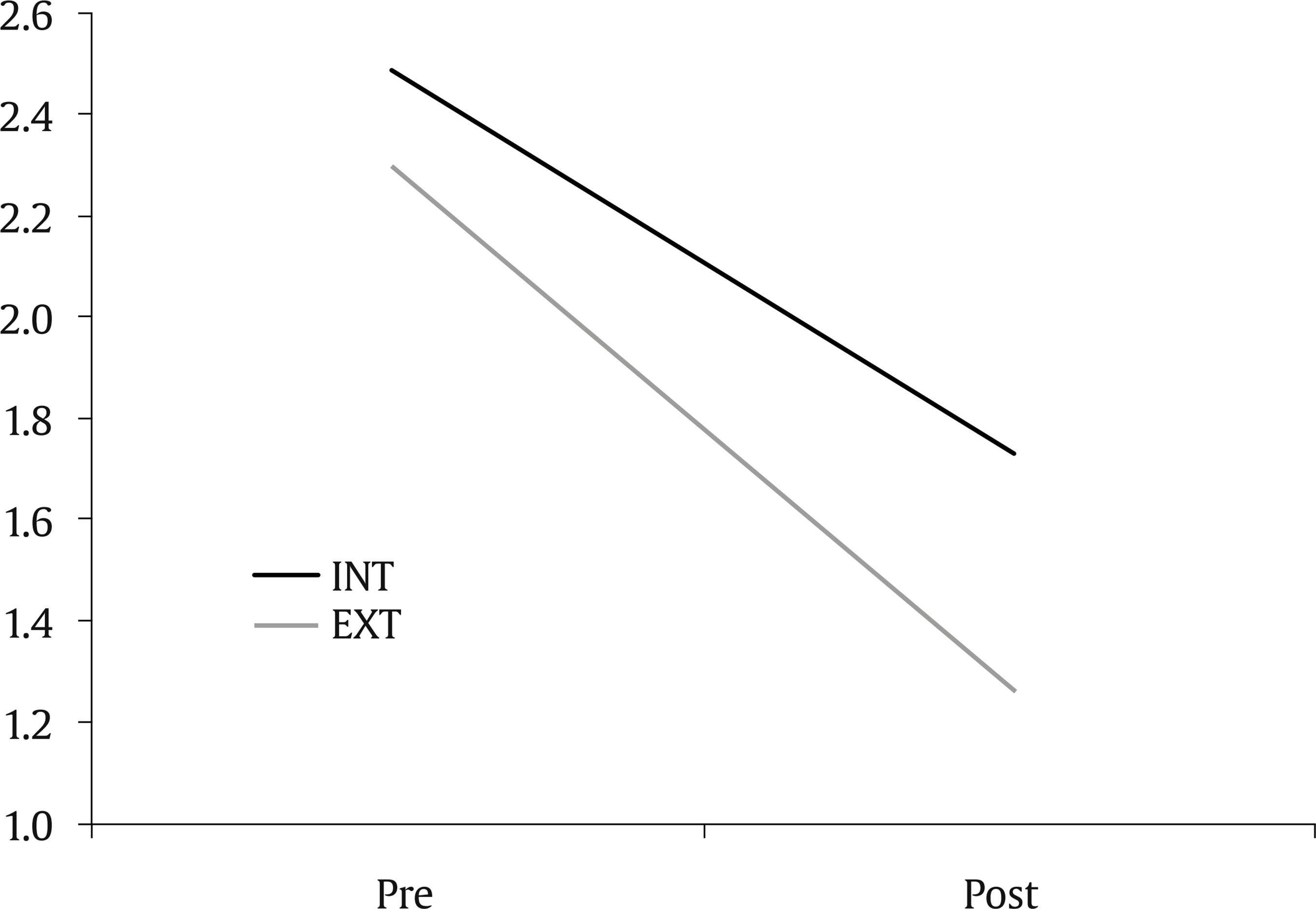 All the variables selected as potential intermediate processes exhibit a change between the pre- and post-measures with a significance of p = .000. Table 3 shows the magnitude of the change in each of them according to the type of personality: externalizers get a lower score in cognitive fusion (C-CFQ) up to 7 points in more extent than internalizers (between 12.2 and 1.9 points of difference with a 95% level of confidence), but there were no significant differences between both types in the rest of the variables. Table 3 Mean Differences (Student-t) between Internalizers (INT) and Externalizers (EXT) in the Variables of Change (pre-post)  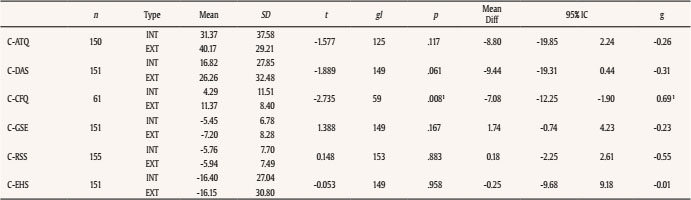 Note. 1Statististically significant. CATQ = change (pre-post) in Automatic Thoughts Questionnaire; CCFQ = change in Cognitive Fusion Questionnaire; CDAS = change in Dysfunctional Attitudes Scales; CGSE = change in General Self-Efficacy Scale; CEHS = change in Social Skills Scale; CRSS = change in Rosenberg Self-esteem Scale. The six pre-post change variables show high correlations with each other (Pearson’s r ranges from .37 to .74 in absolute scores, p < .01), which significantly diminish by controlling the effect of their association with the change in symptom severity (C-GSI) (Table 4, Figure 3). Figure 3 Partial Correlations (Pearson’s r) among the Variables of pre-post Change  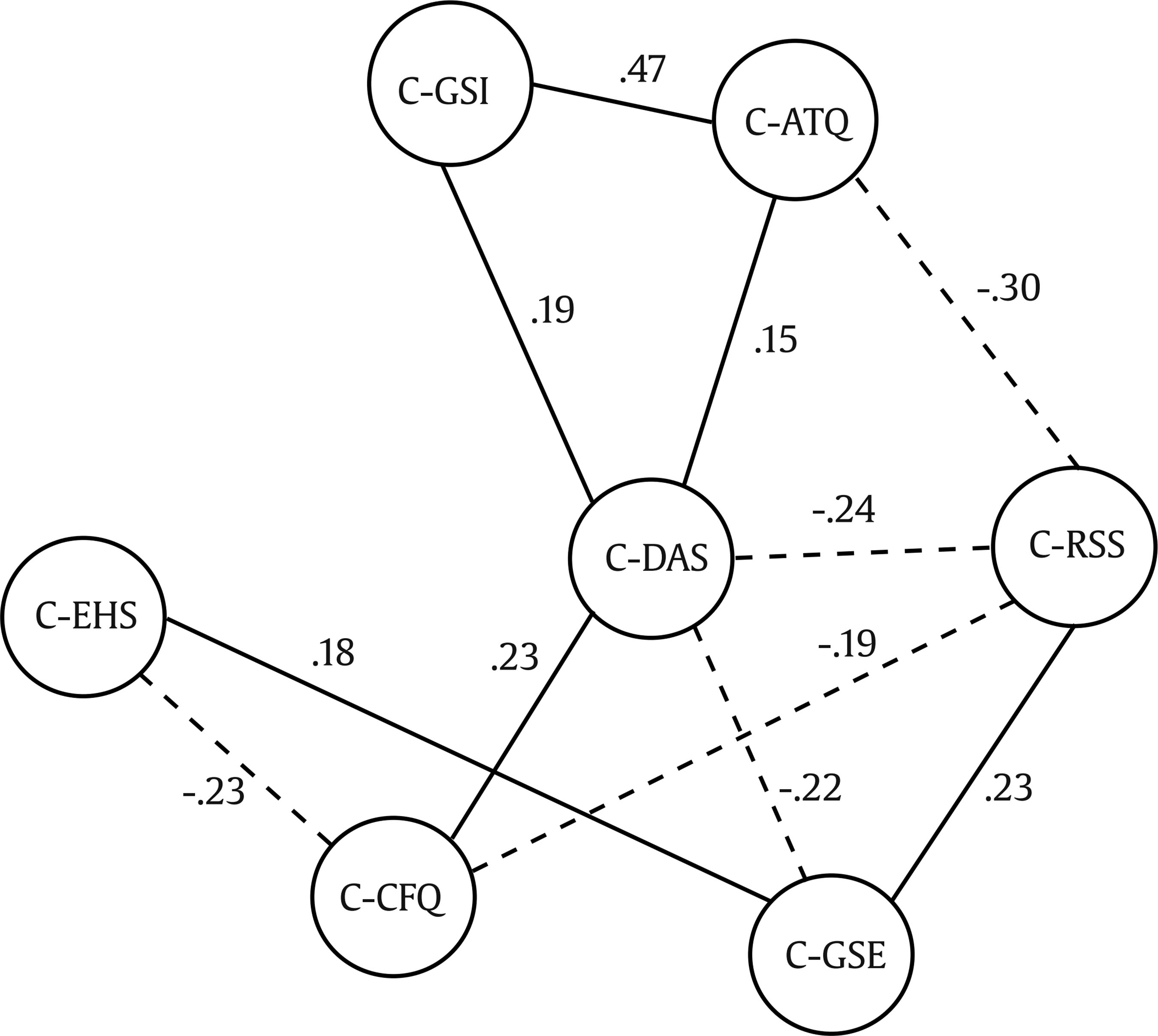 Note. C-ATQ = change (pre-post) in Automatic Thoughts Questionnaire; C-CFQ = change in Cognitive Fusion Questionnaire; C-DAS = change in Dysfunctional Attitudes Scales; C-GSE = change in General Self-Efficacy Scale; C-EHS = change in Social Skills Scale; C-GSI = change in Global Severity Index of the Symptom Checklist-90-Revised; C-RSS = change in Rosenberg Self-esteem Scale. Table 4 Pearson’s r Zero-order Correlations (right superior angle) and Partial Correlations (left inferior angle) with C-GSI as Control Variable  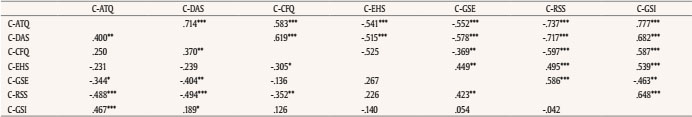 Note. C-ATQ = change (pre-post) in Automatic Thoughts Questionnaire; C-CFQ = change in Cognitive Fusion Questionnaire; C-DAS = change in Dysfunctional Attitudes Scales; C-GSE = change in General Self-Efficacy Scale; C-EHS = change in Social Skills Scale; C-GSI = change in Global Severity Index of the Symptom Checklist-90-Revised; C-RSS = change in Rosenberg Self-esteem Scale *p < .05,**p < .01, ***p < .000. With the stepwise regression analysis, we intend to choose the least redundant predictive model presented by the associations of these six variables on the change in symptom severity (C-GSI). The model does not meet all the assumptions well (Durbin-Watson = 1.73, tolerance = .49, VIF = 2.04, standardized residuals: M = -0.16, SD = 1.12), so the results must be interpreted with caution. Two variables (C-ATQ and C-DAS) can explain more than half of the variance of C-GSI (F(2, 49)= 42.96, p = .000, R2 = .63) and are therefore proposed as mediators of the effect exerted by personality type (independent variable) on severity of symptoms. Mediation analysis (see Figure 4) is presented in Table 5: the distal variable (X) is personality type, mediating variables (M1 y M2) are change in automatic thoughts (C-ATQ) and change in dysfunctional attitudes (C-DAS), the criterion variable (Y) is change in symptom severity (C-GSI). To control the effects of the magnitude of pre variables, these are incorporated into the analysis as covariates (n = 145). Table 5 Mediation Analysis: Direct and Indirect Effects of Personality Type (PT) on Change in Symptom Severity (C-GSI). Mediator Variables: C-ATQ y C-DAS. Covariate variables GSIpre, ATQpre, and DASpre (N = 145)  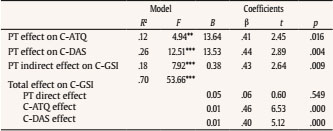 Note. C-ATQ = change (pre-post) in Automatic Thoughts Questionnaire; C-DAS = change in Dysfunctional Attitudes Scales; C-GSI = change in Global Severity Index of the Symptom Checklist-90-Revised; PT = Personality type (internalizers vs. externalizers). **p < .005, ***p < .000. The conditions of the mediation model are met, and it is observed that the effect of personality type on symptom change (β = .43, p = .009) ceases to be significant when the two mediating variables are included (β = .06; p = .549). The Sobel test proves that the indirect effect is different from zero: z1 = 2.29, p = .022; z2 = 2.53, p = .011. Using the bootstraping technique with 5,000 iterations, an indirect effect of .38 is obtained (95% CI [.09, .57]), the direct effect being .05 (95% CI [-.12, .23]), not significant for including zero in the interval. Data of the present paper replicate, in a remarkably larger sample, findings of a previous study (Ramos et al., 2017) that supported the significant reduction of symptoms in people with a diagnosis of severe PD who receive an specialized multi-professional intervention articulated from the therapeutic community model for 6 months. Adherence to the program appears related to a lower intensity of antisocial and passive-aggressive traits and a greater intensity of obsessive-compulsive traits. Sexual differences have been irrelevant in this respect, but those who drop out are two and a half years younger. The group of adherents has significantly reduced their disturbance or symptomatic distress to subclinical mean levels. Both the rate of adherence to the program and the results obtained (with effect sizes between moderate and large) are similar to those reported by other studies with PD, which confirms the widespread conviction that different therapies produce equivalent results and accentuates the need to investigate change processes. Although incidental, the sample could be considered representative of the severe segment of people with a diagnosis of PD, both in the sense of socio-family and work dysfunctionality, morbidity and clinical comorbidity, and use of resources, as in the resistance to change; in fact, they have been referred from a specialized outpatient level (mental health centers) to a superspecialized hospitalization level (hospital therapeutic community), as no progress had been achieved at the previous level. Among severe PD, overlapping of dysfunctional traits and co-diagnosis of types is usual, which generates between-categories permeability and intra-category heterogeneity. Therefore, studies that incorporate typical patients rather than typical diagnoses are needed (for example, “treatment resistant patients”). If traditional diagnostic categories have significant validity problems, and treatment programs have a nonspecific efficacy, the need to re-categorize people and identify individual processes of change is understood. We psychometrically (through cluster analysis) found a personality typology potentially useful in this regard, since it can totally and exclusively discriminate participants according to their scores on the 13 personality traits of the MCMI-II: internalizers vs. externalizers. Their respective typological and clinical differences have been described elsewhere (Ramos et al., 2019); here we sought to verify (1) if there was a differential response to the intervention and (2) if any cognitive process could mediate or modulate that response. There were no differences between internalizers and externalizers in the rate of adherence to the program. As the latter had a higher score on antisocial and passive-aggressive scales and the former on obsessive-compulsive scales, a higher percentage of dropouts was expected in externalizers. These features that would make them more vulnerable to non-adherence, though, must have been compensated by other factors that were not explored. Neither age nor sex differentiate them. The main finding was that externalizers obtain a better final result: they managed to reduce the intensity of the symptomatic malaise more than internalizers (with a moderate effect size), even controlling initial intensity differences. This achievement is more accelerated, as can be seen in Figure 2 (pre-post lines of change are not parallel) and also in the significance of the interaction effect between time and personality type (with a low effect size). The mediating process that explains most of the variance of symptomatic severity change has turned out to be the reduction of the intensity of negative thoughts, followed by the change in dysfunctional attitudes. In neither of the two achievements typological differences appeared: both externalizers and internalizers benefited in both processes in a similar way; only in cognitive fusion change externalizers showed superiority. Change in automatic thoughts was the best predictor of symptomatology improvement. It not only precedes proximally depressive symptomatology, mediates between depression and suicidal behavior, and is related to a wide range of symptoms, but their modification seems key to the relief of symptomatology and suffering. The high association found between the change in both variables (C-ATQ and C-GSI) suggests a synergy or cascade effect (Selby, Anestis, & Joiner, 2008). On the other hand, change in dysfunctional attitudes occupies a central place in the network of associations (partial correlations) of the set of variables, as can be seen in Figure 3. Improvement in attitudes seems to be a strategic factor, since its effect is associated with greater intensity to a greater number of processes. The finding that externalizers manage to lower the level of cognitive fusion more than internalizers and that the starting level was not different at the beginning of the intervention would suggest that their advantage over internalizers in post-intervention benefit could rest on this process. But it is also possible that the best prognosis of externalizers that adhere to the treatment is due rather to a disadvantage of internalizers: their characteristic hyper-controlling and self-attentional tendency would make them more impervious to the modification of automatic negative thoughts; this factor is what, in the end, was shown to contribute better and more directly to symptom change. In the endeavor of theoretical rethinking and practical designing of new therapy models, the relationship between these overlapping constructs cannot be ignored. In their model of emotional cascades, Selby et al. (2008) suggested that cognitive rumination processes connect emotional deregulation with behavioral deregulation. And it has been argued that the BPD is an emerging self-powered circuit of emotional deregulation and disruptive behaviors that try to curb the emotional intensity produced by recurring negative thoughts (Selby & Joiner, 2009). Because of the similarity of the intensity of automatic negative thoughts (ATQ) with the rumination processes, it seems fruitful to examine our results in light of the model. The fact that the borderline scale of MCMI-II was the least discriminatory between externalizers and internalizers (Figure 1, z scores) and that the average base rate is higher than 94 in both groups is consistent with the proposal by Selby and Joiner (2009) and allows expanding their model to all severe PD. The BPD category would be irrelevant as it lacks discriminatory power. It could refer to the common dimensional factor that every PD shares (Sharp et al., 2015). The fact that BPD covariates with neuroticism (Kendler, Myers, & Reichborn-Kjennerud, 2011) points in the same direction. The relevance of this paper in the current conceptual debate and in the search for processes that improve therapeutic practice must be framed within the framework of its limitations. Only one symptom change index was used (the GSI of the SCL90-R). Such reductionism imposes caution not to evaluate an entire intervention program with this simple parameter; but the evaluation of the program was not an objective of this work. Besides, data coming from self-report lose objectivity, but instead allows access to the communicated subjectivity that is a key aspect in an individual’s personal identity. The number of comparisons among variables varied because of lost values, and no method to correct them was applied; it is relevant to be particularly aware of the fact that we got data from only n = 61 participants in the C-CFQ variable. Also the addition of a representative sample of the mild or moderate segment of PD would allow for a wider generalizability of results. Successive follow-ups would reinforce the conclusions, since the challenge of treatment is to maintain the change, not to obtain mere ephemeral changes. Current clinical research is thus leading to “rethink” the diagnosis of BPD. The form (pathoplasty) described in classical psychopathological syndromes can emerge from diachronic and dynamic processes that are reinforced and made more dominant and probable throughout the life cycle. If there is a network of situational and personal processes (which is shaping personality) that is generating personal vulnerability or resilience in an individual (diathesis), its identification, understanding and modification would save personal and socio-family consequences of an already emerged (and consolidated) disorder. This idea of PD as a diathesis (Tyrer, 2007), on the other hand, relieves the stigmatizing weight of a diagnosis of PD. Moreover, the finding of processes such as automatic negative thoughts, whose activation (facilitated by personality and stimulated by precise circumstances) triggers symptom escalation, allows a better focus on the therapeutic intervention targets. Instead of treating a disorder that a person suffers (medical model), it is possible to intervene in the network of processes that come into play inside and outside a person: certain environmental circumstances, particular social interactions, specific individual processes. Bateman et al. (2018) believe that it would be wrong to conceive of BPD as a disorder: it would be rather a vulnerability indicator whose core would be constituted by a relative lack of tolerance to adversity, and assume that what makes therapies effective is precisely their ability to reduce this vulnerability. BPD can be understood as an entrenched form of adaptation to the social context, rather than as a deficit. For these authors, epistemic distrust interferes with the communicative exchange that protects against emotional dysregulation, impulsivity, and social dysfunctionality of people with severe mental health problems. Any intervention that facilitates trust inside and outside formal spaces of therapy will be, from this point of view, an effective intervention. The emphasis on promoting a sense of belonging and the empowerment of personal responsibility (sense of agency) is distinctive of therapeutic communities (Pearce & Pickard, 2013). The community experience, in its double aspect of being-with and being-for (affection and direction, get along and get ahead), can reconstitute trust, facilitate openness and flexibility, modify attitudes, promote self-worth and meaning; then, the emergence of positive thoughts would, with a cascading effect, make a person commit to health behaviors, feel better, and become more resilient with adversities that come with being alive. Conflict of Interest The authors of this author declare no conflict of interest. Cite this article as: Ramos, J. M., Sánchez, A., & Doll, A. (2020). Differential outcome of a therapeutic community program for internalizing and externalizing personality disorders:A change in cognitive processes mediates symptoms improvement. Clínica y Salud, 31(1), 47-53. https://doi.org/10.5093/clysa2020a3 References |
Cite this article as: Ramos, J. M., Sánchez, A., & Doll, A. (2020). Differential Outcome of a Therapeutic Community Program for Internalizing and Externalizing Personality Disorders: A Change in Cognitive Processes Mediates Symptom Improvement. ClÃnica y Salud, 31(1), 47 - 53. https://doi.org/10.5093/clysa2020a3
jmramos@cop.es Correspondence: jmramos@cop.es (J. M. Ramos).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







