Associations of knowledge about AlzheimerŌĆÖs disease, dysfunctional cognition, and coping with caregiverŌĆÖs blood pressure
[El conocimiento sobre la enfermedad de Alzheimer, la cognici├│n disfuncional y el afrontamiento en la tensi├│n arterial del cuidador]
Carlos Vara-García1, Rosa Romero-Moreno1, María Márquez-González2, Samara Barrera-Caballero1, María del Sequeros Pedroso-Chaparro1, and Andrés Losada-Baltar1
1Universidad Rey Juan Carlos, Alcorc├│n, Madrid, Spain; 2Universidad Aut├│noma de Madrid, Spain
https://doi.org/10.5093/clysa2020a33
Received 1 April 2020, Accepted 26 November 2020
Abstract
Dysfunctional ways of thinking and coping with caregiving have been associated with worse caregivers’ cardiovascular health. The objective of this study is to analyze the associations between caregivers’ knowledge about Alzheimer’s disease, dysfunctional thoughts, experiential avoidance, and blood pressure. Participants were 123 family caregivers of a relative with dementia. Path analysis was used to analyze the association between the assessed variables. The obtained model shows that there is a significant and negative relationship between caregivers’ knowledge about Alzheimer’s disease and systolic blood pressure, potentially mediated by caregivers’ dysfunctional thoughts and experiential avoidance. The findings of this study provide support to the idea that a lack of knowledge about Alzheimer’s disease may contribute to maladaptive ways of thinking about caregiving, increasing caregivers’ cardiovascular risk.
Resumen
El pensamiento disfuncional acerca del cuidado o el inadecuado afrontamiento del mismo han sido asociados con una peor salud física de los cuidadores. El objetivo de este estudio es analizar las asociaciones entre el conocimiento de los cuidadores sobre la enfermedad de Alzheimer, los pensamientos disfuncionales, la evitación experiencial y la presión arterial. Los participantes de este estudio fueron 123 cuidadores de un familiar con demencia. Un modelo de senderos fue empleado para analizar la relación entre las variables. El modelo obtenido muestra que existe un relación negativa y significativa entre el conocimiento de los cuidadores acerca de la enfermedad d Alzheimer y la presión arterial sistólica, potencialmente medida por los pensamientos disfuncionales y la evitación experiencial de los cuidadores. Los resultados de este estudio apoyan la idea de que una falta de conocimiento acerca de la enfermedad de Alzheimer puede contribuir a cogniciones desadaptativas acerca del cuidado, incrementando el riesgo cardiovascular de los cuidadores.
Palabras clave
Conocimiento acerca de la enfermedad de Alzheimer, Presi├│n arterial, Cuidado, Pensamientos disfuncionales, Evitaci├│n experiencialKeywords
AlzhiemerŌĆÖs disease knowledge, Blood pressure, Caregiving, Dysfunctional thoughts, Experiential avoidanceCite this article as: Vara-García, C., Romero-Moreno, R., Márquez-González, M., Barrera-Caballero, S., Pedroso-Chaparro, M. D. S., and Losada-Baltar, A. (2021). Associations of knowledge about AlzheimerŌĆÖs disease, dysfunctional cognition, and coping with caregiverŌĆÖs blood pressure. Cl├Łnica y Salud, 32(2), 79 - 87. https://doi.org/10.5093/clysa2020a33
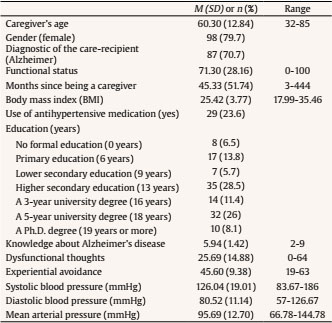
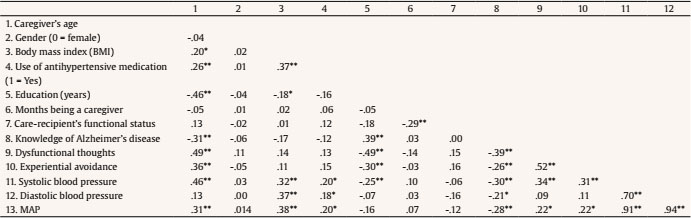
carlos.vara@urjc.es Correspondence: carlos.vara@urjc.es (C. Vara Garc├Ła).Caring for a relative with Alzheimer’s disease or related disorders has been considered to be a prototypical example of chronic stressful situations (Vitaliano et al., 2004). The main models of the caregiving stress process assume that “the onset and progression of dementia are stressful for both the patient and the caregiver” (Schulz & Sherwood, 2008, p. 2). In this sense, caregivers’ health consequences are considered to be relevant for care recipients’ health outcomes, as caregiver distress is associated with institutionalization, elder abuse of dementia care recipients, and worsening behavioral and psychological symptoms of dementia (Stall et al., 2019). In addition, caregivers’ mental health predicts mortality of patients with neurodegenerative diseases (Lwi et al., 2017). The caring situation has also been found to be associated with negative consequences for caregivers’ physical and mental health, including increased risk of developing a cardiovascular disease (Mausbach et al., 2007; Roepke et al., 2011; Vitaliano et al., 2003; von Känel et al., 2008). In spite of the existence of multiple risk factors (poor health habits, genetic predisposal, etc.), blood pressure (BP) has been described as one of the most common risk factors for developing cardiovascular disease (i.e., stable and unstable angina, myocardial infarction, unheralded coronary death, and subarachnoid hemorrhage; Rapsomaniki et al., 2014). However, not all measures of BP seem to react equally to alterations in emotions. In non-caregiver populations it has been suggested that while sadness equally influences systolic and diastolic BP, changes in fear, action, and joy are more related with changes in systolic BP and modifications in anger have been associated with changes in diastolic BP (Sinha et al., 1992). Regarding caregiving research, differential effects have been found for both systolic and diastolic BP (e.g., Vitaliano et al., 1993) and on some occasions even just for one of them (Kim et al., 2007, Vara-García et al., 2019). For this reason, it is a recommendable practice to assess both measures of BP when analyzing the effects of caregiving or related variables. Dementia family caregivers have been found to develop hypertension significantly earlier than non-caregivers (Shaw et al., 1999) and current and long-term caregiving has been associated with hypertension risk (Capistrant et al., 2012). The number of studies analyzing caregiving factors that may contribute to increases in caregivers’ cardiovascular health is sparse. Vitaliano et al. (2002) highlighted the importance of including caregivers’ resources, vulnerability factors and health habits that may influence their health. Among the few existing studies analyzing associations between caregiving resources or psychological factors and their cardiovascular health (von Känel & Albus, 2018), caregivers’ perceived self-efficacy (Harmell et al., 2011; Mausbach et al., 2011) and leisure activities (Chattillion et al., 2013; Chatillion et al., 2012; Mausbach et al., 2012; Moore et al., 2013) have been found to be negatively related to caregivers’ cardiovascular risk. In the caregiving context, dysfunctional thoughts have been seen to be a key variable to understanding the caregiving stress process. Dysfunctional thoughts or attitudes were defined by Beck and colleagues (Beck et al., 1979) and have been traditionally considered as “rigid and inappropriate contingencies of a person to guide and assess one’s behavior” (Kuiper et al., 1989, p. 229). In addition, regarding dementia caregivers, the construct of dysfunctional thoughts about caregiving has been defined as rigid thoughts related to some caregiver statements such as “Having to do everything for the person they are looking after, and preferably, doing it alone” or “Not feeling bad about caring and, if that happens, not showing their feelings publicly” (Losada, Montorio, Knight, et al., 2006). This kind of thoughts has been found to be related with negative outcomes of caregivers’ mental health, such as depression (McNaughton et al., 1995; Stebbins & Pakenham, 2001) or burden (Vázquez-Sánchez et al., 2012). In order to explain how cognitive factors may contribute to caregiver health, Losada, Montorio, Knight, et al. (2006) adapted the cognitive-behavioral model for the explanation of caregivers’ mental health problems. This model highlights the fundamental role that caregivers’ ways of thinking play in the explanation of the health consequences associated with the caregiving process (Cohen et al., 2015). However, to our knowledge, the usefulness of this model for the explanation of caregivers’ physical (e.g., cardiovascular) health has not been tested. In other populations (i.e., undergraduate students and middle-aged adults), dysfunctional thoughts have been linked to worse physical health, specifically with increased systolic and diastolic blood pressure (Ottaviani et al., 2016). In addition, cognitive-behavioral interventions, which have as a main clinical target the decrease and modification of dysfunctional thoughts, have shown promising results in reducing cardiovascular risk markers in people suffering depression or other conditions (Lopresti, 2017). Dysfunctional thoughts have been described in caregivers as cognitive barriers that could make it difficult for them (the caregivers) to take appropriate care of their own mental and physical health (Losada, Montorio, Knight et al., 2006) through different paths. One such path is that dysfunctional thoughts could prevent caregivers from expressing emotional distress associated with caregiving, as some may think that they should not complain or express any negative feeling related to caregiving as it would be perceived as some “sort of betrayal to their family” (Losada, Montorio, Knight et al., 2006, p. 120). Regarding this path, another variable that has been found to be associated with negative caregiver outcomes is experiential avoidance of caregiving. This variable has been described as the fear and evasion of specific negative emotions or thoughts about the care recipient and reluctance to accept or reflect upon one’s own emotions about caregiving (e.g., “I have never felt bad in relation to caring for my relative”), resulting in a maladaptive long-term coping style and negative physical and mental health outcomes (Losada et al., 2014). A related construct, “avoidant coping”, has been considered one kind of emotion-focused strategy (Lazarus & Folkman, 1984) and also associated with physical and mental health in stress processes. It has been suggested that these coping strategies are used “to preserve hope and optimism, to deny both the fact and its implication, not having to accept the worst…” (Lazarus & Folkman, 1984, p. 174), which may lead to an erroneous interpretation of reality. Specifically, avoidant coping refers to an emotion-focused coping style that has the goal of distracting the person, mitigating the impact of stressors on their emotions (Lazarus & Folkman, 1984). Along with other emotion-focused coping strategies, this coping strategy has been thought to be more commonly applied when the situation is perceived as unmodifiable and has to be accepted as it is (Folkman & Lazarus, 1980; Lazarus & Folkman, 1984), and it has often been studied in the caregiving stress process (Gilhooly et al., 2016). Regarding the effects of this coping strategy on physical health, Kohlmann et al. (1996) found that the increases in systolic BP when facing a stressful situation were higher for those participants scoring higher in avoidant coping. Different forms of avoidance coping strategies (such us denial, mental and behavioral disengagement) can be considered forms of experiential avoidance (Hildebrandt & Hayes, 2012). Moreover, it has been highlighted that experiential avoidance (as a chronic thought-suppression strategy) plays a role in cardiovascular risk (Ingjaldsson et al., 2003). Although avoidant coping strategies or experiential avoidance can be useful in the short term, often providing an opportunity for emotions to calm down, they are ineffective in the longer term (Carver, 2011), with negative effects on caregivers’ depression (Kim et al., 2007; Mausbach et al., 2006; Spira,et al., 2007), anxiety (Cooper et al., 2007), and blood pressure (Kim et al., 2007). The cognitive-behavioral model adapted to caregiving (Losada, Montorio, Knight et al., 2006) also suggests that caregivers’ ways of thinking may be affected by some contextual variables and culturally related variables. Specifically, Losada, Montoro, Izal, et al. (2006) suggested that dysfunctional thoughts “are not independent of culture” (p. 914), and cultural beliefs have also been shown to be associated with health outcomes in dementia caregivers (Dilworth-Anderson et al., 2004; Knight et al., 2002). These variables could include the level of formal education and knowledge about Alzheimer’s disease. Although this last variable has scarcely been studied in relation to caregiver health, greater knowledge has been related to some demographic characteristics of caregivers such as, for example, being a child caregiver (rather than a spouse; Werner, 2001) and having received more years of formal education (Carpenter et al., 2011; Werner, 2001). Also, greater knowledge about Alzheimer’s disease has been found to be associated with adaptive coping strategies, such as a higher sense of competence and confidence (i.e., “I feel that in all, I am a very good caregiver”), reduced expectations regarding their care-recipients (i.e., “I try to accept my relative as he/she is, not as I wish he/she could be”), more frequent use of positive comparisons (i.e., “I’m looking for things that I have always liked or admired in my relative”), and lower levels of depression in the caregiver population (Graham et al., 1997), a variable which, as mentioned above, has been associated with dysfunctional thoughts (Graham et al., 1997; Losada, Montorio, Knight et al., 2006; Losada et al., 2010) and experiential avoidance (Márquez-González et al., 2018) or avoidant coping (Kim et al., 2007; Mausbach et al., 2006; Spira et al., 2007) in this population. Similarly, higher dysfunctional thoughts about caregiving (e.g., “No matter how badly a caregiver feels, he/she should not vent with others because it would be disrespectful to the person being cared for”) have been found to be associated with high experiential avoidance in family dementia caregivers (Losada et al., 2014). However, as far as we are aware, the role of caregiver knowledge about Alzheimer’s in the caregiving stress process (specifically, its relationship with dysfunctional thought and experiential avoidance) remains understudied, nor has its association with cardiovascular risk been researched. We believe the findings reported above provide support for the healthy pathway that was described by Losada, Montorio, Knight et al. (2006), since it suggests that having knowledge about the illness contributes to a rational approach to the caregiving situation by activating thoughts such as “caregiving is very complex and demanding, so I need help from others”. Conversely, a lack of knowledge about the illness may make caregivers more prone to have dysfunctional thoughts such as “a caregiver should only seek help from others or find other alternatives when the caregiving situation is at its worst, or when he/she can no longer handle it”, which may contribute to an avoidant coping style. As posited by these authors (Losada, Montorio, Knight et al., 2006), “these types of beliefs may contribute to creating a general attitude of ‘self-sacrifice’ and ‘self-neglect’ among caregivers”, leading to ‘behaviors’ that will result, sooner or later, in negative physical and psychological consequences for the caregiver” (p. 122). Considering that (a) lacking knowledge about Alzheimer’s or related diseases may contribute to the development of maladaptive ways of thinking about caregiving, (b) dysfunctional thoughts about caregiving and experiential avoidance have been suggested as maladaptive resources for adaptive coping with caregiving (e.g., Losada et al., 2010; Losada et al., 2014; Spira et al., 2007), and that (c) these maladaptive ways of thinking have been related to higher levels of blood pressure in caregivers and other populations, the objective of this study is to provide preliminary support to the theoretical cognitive-behavioral model adapted to caregiving, analyzing the association between these variables and caregivers’ blood pressure. Our hypothesis is that having greater knowledge about Alzheimer’s disease will be associated with fewer dysfunctional thoughts about caregiving and less experiential avoidance, and these lower scores on dysfunctional thoughts and experiential avoidance will be associated with lower blood pressure, even when controlling for other variables known to be related to cardiovascular risk (e.g., Body Mass Index and antihypertensive medication). Participants and Procedure Participants in this study were 123 family caregivers caring for a relative with dementia. Inclusion criteria were: a) being the main caregiver of a relative with dementia, b) being at least 18 years of age, c) devoting an average of at least one hour daily to caregiving tasks, and d) providing care for at least 3 consecutive months. Following previous recommendations (Harmell et al., 2011; von Känel et al., 2011), caregivers with severe hypertension (> 200/120 mmHg) were excluded from the study in order to avoid major effects on study outcomes when including people with cardiovascular problems. Caregivers were contacted through social services, health care centers, and adult day services from the city of Madrid (Spain), and were first contacted through a brief telephone interview aimed at confirming the inclusion criteria. All participants were then cited for an individual face-to-face interview at their centers of reference or at home, and provided written informed consent to being studied. The Ethics Committee of [The Ethics Committee of Universidad Rey Juan Carlos] approved the study protocol. Measures Demographic data and health characteristics. Demographic information collected included caregiver age, gender, time since being a caregiver (in months), and illness of the care-recipient. Also, functional status of the care-recipient was assessed through the Barthel Index (Mahoney & Barthel, 1965). Years of formal education were collected using the following scale: 1 = no formal education, 2 = primary education, 3 = lower secondary education, 4 = higher secondary education, 5 = three-year university degree, 6 = five-year university degree, and 7 = PhD or equivalent degree. Although this is assessed as a categorical variable following the Spanish school system, in the analyses it was treated as continuous variable (higher scores, higher levels of formal education) as it facilitates interpretation, similar to what has been done in other studies (e.g., Montorio et al., 2009). Finally, height and weight were collected in order to calculate the body mass index (BMI), and the BMI and the use of antihypertensive medication were collected so that they could be controlled for in the analysis of dimensions associated with blood pressure. Blood Pressure. An electronic sphygmomanometer OMROM M7 (HEM-780-E) was used for measuring resting BP. Following the same procedure as in previous studies (e.g., Márquez-González et al., 2018, Vara-García et al., 2019), three measures of systolic and diastolic BP were taken throughout the individual interview, which lasted an hour and a half approximately. The first BP measure was tested at the beginning of the interview (after the informed consent was signed), the second BP measure was taken in the middle of the interview (approximately 45 minutes after the first assessment), and the third BP assessment approximately one hour and a half after the first assessment (at the end of the interview). Then, a mean score of these three measurements was computed in order to establish a more reliable and stable measure of BP. Finally, mean arterial pressure (MAP) was calculated with the following formula: (Systolic BP + 2 * Diastolic BP)/3. Knowledge about Alzheimer’s disease. Considering time pressure constraints for the assessment of dementia family caregivers, and that knowledge about Alzheimer’s disease was not the main target variable of a larger project in which this study was framed (Losada et al. 2015), only nine items of the Alzheimer’s Disease Knowledge Scale (ADKS; Carpenter et al., 2009) were assessed. Specifically, the assessed items corresponded to the factors “caregiving” and “symptoms” from the ADKS (e.g., “when people with AD repeat the same question or story several times, it is helpful to remind them that they are repeating themselves”). The items are rated on a true or false scale. The original scale reported low internal consistency indexes (Cronbach’s alpha) for the subscales of the ADKS ranging from .26 to .60 (Carpenter et al., 2009). The reliability (Cronbach’s alpha) of the ADKS items which were included in the present study also has a very low internal consistency index (Cronbach’s alpha = .20). Carpenter and his collaborators (Carpenter et al., 2009) commented that the low reliability had to do with the true/false response format and that the ADKS is not an exhaustive scale of knowledge about Alzheimer’s and related disorders. In spite of these limitations, Carpenter et al. (2009) stated that the ADKS is a useful tool for measuring knowledge, with a design based on 21 other scales developed for measuring this same variable, although improvements of the scale are necessary. Dysfunctional thoughts about caregiving. The dysfunctional thoughts about caregiving questionnaire (DTCQ; Losada, Montorio, Izal et al., 2006) was used. This is a 16-item scale (e.g., “It is logical for caregivers to give up their own needs, setting aside their own life satisfaction in favor of their relative’s needs”) with items rated on a 5-point Likert-type scale between 0 (totally disagree) and 4 (totally agree). This scale has proven to have good psychometric properties (Montorio, et al., 2009). The internal consistency (Cronbach’s alpha) for this scale in the present study was .90. Experiential avoidance in caregiving. The Experiential Avoidance in Caregiving Questionnaire (EACQ; Losada et al., 2014) was used. The EACQ has 15 items (e.g., “One should not have bad thoughts about the person one is caring for”) which are rated on a 5-point Likert-type scale between 1 (not at all) to 5 (a lot). This scale has proven to have acceptable psychometric properties (Losada et al., 2014). The internal consistency (Cronbach’s alpha) for this scale in the present study was .66. Statistical Analyses Following Tabachnick and Fidell’s (2001) criteria, analyses for sample normality and outliers (univariate and multivariate were conducted). No univariate or multivariate (Mahalanobis’ distance of p <.001) outliers were found. Then, in order to control for potential variability in BP derived from the potential stressful situation of the interview with caregivers, in which discussions of difficult circumstances occurred, we tested if changes in blood pressure over the interview (at three separate moments) were significant. With this objective, mixed model analyses considering the three measures of blood pressure as dependent variables and time as predictor were conducted. In order to analyze the relationship between the variables of the study, correlation analyses were done. On the basis of the obtained correlations, and drawing upon the cognitive-behavioral model adapted to the caregiving process (Losada, Montorio, Knight, et al., 2006), a path model was developed. This model included sociodemographic variables (caregivers’ age, gender, and level of formal education), physical health variables (BMI and use of antihypertensive medication) and contextual variables (knowledge about AD) as dimensions that may have an influence on dysfunctional thoughts about caregiving and experiential avoidance which, in turn, may influence the consequences for caregivers’ blood pressure. In a first step, all the correlations that were shown to be significant in the correlation analyses were established as paths in the model. Finally, following the suggestions by Jöreskog and Sörbom (1993), only those associations that remained significant after the first path analysis were included in the final model (see Figure 1). In addition to the chi-square (χ2) statistic, the chi-square value divided by the degrees of freedom (χ2/df) was considered, with values under or near 3 indicating a good model fit (Bollen, 1989). The root-mean-square error of approximation (RMSEA), the comparative fit index (CFI) and the Tucker-Lewis index (TLI) were also assessed as additional indicators of model fit, with values of RMSEA under .05 and of TLI and CFI over .95 representing an excellent fit of the data. Mediation was analyzed following the bootstrapping approach recommended by Preacher and Hayes (2004), using 1,000 bootstrap samples, with a bias-corrected confidence interval of .95. Also, following the suggestions made by Byrne (2016), a Bollen-Stine bootstrap (Bollen & Stine, 1992) was also conducted for testing the null hypothesis that the specified model is correct. Descriptive Data The characteristics of the sample are shown in Table 1. The mean age of the participants was nearly 60 and most of the caregivers were female (79.7%). The most common educational levels were higher secondary school (28.5%) and 5-year university degree (26%). Measurement of Blood Pressure Regarding changes in blood pressure during the assessment process (three measurements of blood pressure were made throughout the interview), the results of the mixed model analysis showed no significant effects on MAP either from the beginning to the second measurement point of the interview, (intercept = 97.28, estimate = -.79, SE = .42, df = 122, t = -1.90, p = .06, 95% confidence interval (CI), lower bound = -1.62 and upper bound = .034), or from the beginning to the end of the interview, (intercept = 95.44, estimate = .13, SE = 0.42, df = 122, t = 0.31; p = .76, 95% (CI), lower bound = -.70 and upper bound = .95). Similarly, results showed no significant effects of time on systolic or diastolic BP measures either from the beginning to the second measurement point of the interview, systolic BP, (intercept = 127.56, estimate= -.76, SE =.0 52, df =122, t = -1.45, p = .15, 95% confidence interval (CI), lower bound = -1.78 and upper bound = .27); diastolic BP, (intercept = 82.14, estimate = -.80, SE = 0. 42, df = 122, t = -1.60, p = .11, 95% confidence interval (CI), lower bound = -1.81 and upper bound = .19), or from the beginning to the end of the interview, systolic BP, (intercept = 126.64, estimate = -.30, SE =0. 57, df = 122, t = -0.53, p = .60, 95% (CI), lower bound = -1.14 and upper bound = .82); diastolic BP, (intercept = 79.83, estimate = .34, SE = o.46, df =122, t = .73, p = .47, 95% confidence interval (CI), lower bound = -.58 and upper bound= 1.27). Correlational Data The correlation matrix of the assessed variables is shown in Table 2. As can be seen, knowledge about AD was significantly and negatively correlated with age, experiential avoidance, dysfunctional thoughts, systolic and diastolic BP, and significantly and positively correlated with the level of formal education. Dysfunctional thoughts were significantly and positively correlated with age, experiential avoidance and systolic BP, and significantly and negatively correlated with level of formal education and knowledge about AD. Finally, experiential avoidance was significantly and positively correlated with age, dysfunctional thoughts and systolic BP, and significantly and negatively associated with level of formal education and knowledge about AD. Gender was not significantly correlated with the assessed variables and, for this reason, was not included at the final model. Diastolic BP was found to be significantly correlated only with BMI, use of antihypertensive medication, knowledge of AD, and systolic BP, but not with dysfunctional thoughts and experiential avoidance. Finally, MAP was significantly correlated with age, BMI, use of antihypertensive medication, knowledge of AD, dysfunctional thoughts, experiential avoidance, systolic and diastolic BP. The path model was tested with the three measures of BP (systolic, diastolic, and MAP) in accordance to their significant correlations. Path analyses of knowledge about Alzheimer’s disease, dysfunctional thoughts, and experiential avoidance on blood pressure Figure 1 shows the associations obtained through the path analysis for systolic BP. As mentioned in the data analysis section, only significant paths are considered in the final model. Higher caregiver age (standardized direct effect: .37, p <.01, SE =.080, CI = .24, .48) and higher BMI (standardized direct effect: .24, p <.01, SE =.07, CI = .11, .35) were positively associated with higher levels of systolic BP. Also, a positive association between systolic BP and experiential avoidance (standardized direct effect: .16, p < .05, SE =.08, CI = .03, -.29) was found. The positive correlation that was found between knowledge about AD and systolic BP is no longer significant in this analysis, suggesting that the association may be mediated by dysfunctional thoughts and experiential avoidance. The results of the mediation analysis are significant (standardized indirect effect: -.02, p < .05, SE =.01, CI = -.047, -.003), showing that the effect of knowledge about AD and systolic BP is indirect, through its direct association with dysfunctional thoughts (standardized direct effect: -.19, p < .01, SE = .08, CI = -.323, -.077) and its indirect association with experiential avoidance (standardized indirect effect: -.101, p < .01, SE = .04, CI = -.179, -.038), mediated by a direct association between dysfunctional thoughts and experiential avoidance (standardized direct effect: .52, p < .01, SE = .08, CI = .374, .634). A similar finding was obtained regarding the association between dysfunctional thoughts and systolic BP. The significant association between these variables that was obtained in the correlational analysis is no longer significant, suggesting that the effect of dysfunctional thoughts on systolic blood pressure is mediated by experiential avoidance (standardized indirect effect: .08, p < .05, SE = .05, CI = .02, .16). The final model explains 25% of the variance of systolic BP. Figure 1 Path Diagram for Systolic Blood Pressure.  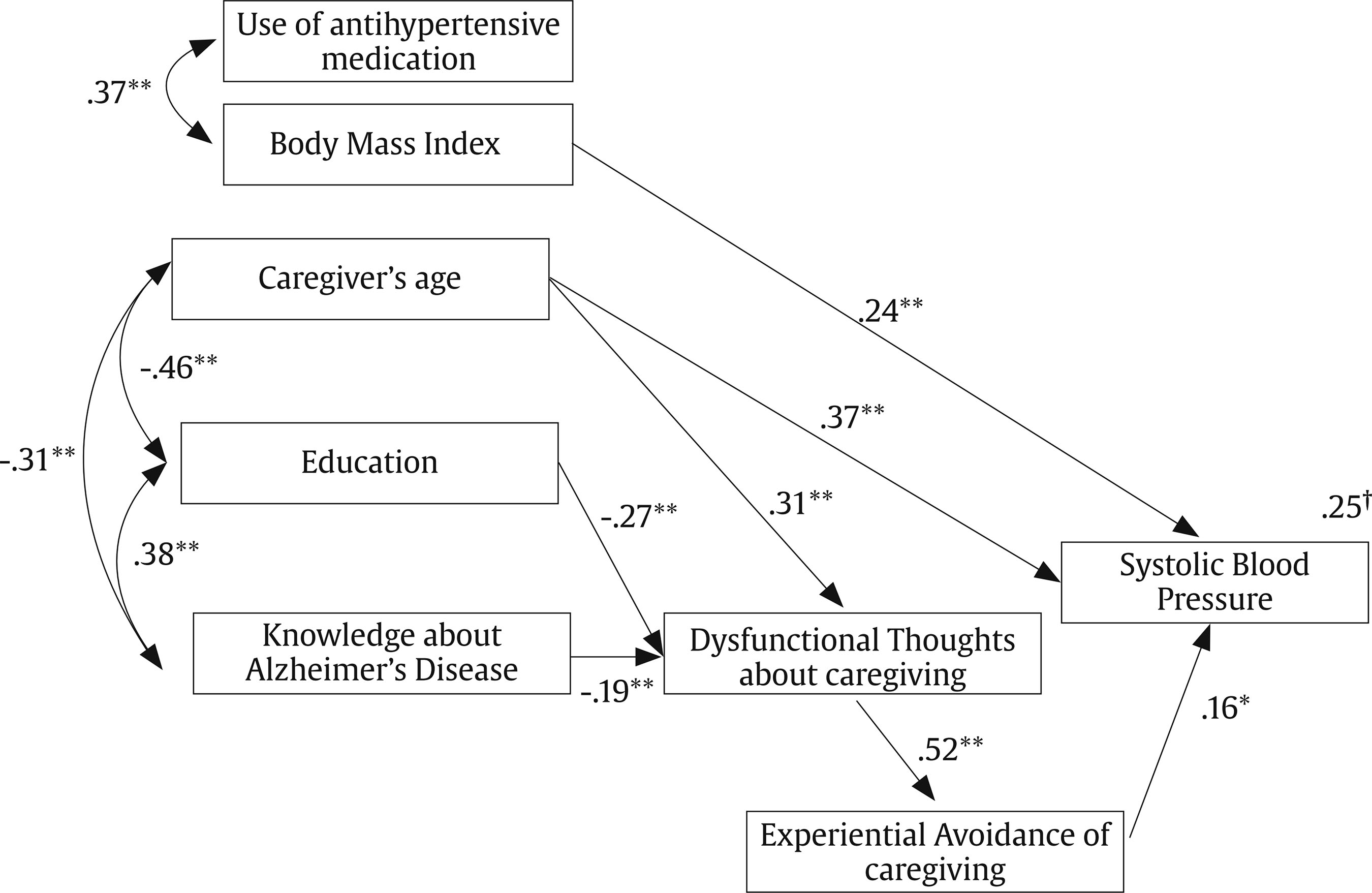 †Variance explained by the model *p < .05, **p < .01. The obtained fit indexes suggest an excellent fit of the path model to the data (χ2 = 19.192, p = .318; χ2/df = 1.129, RMSEA = .033, CFI = .989, and TLI = .982). The Bollen-Stripe bootstrap also showed a good fit of the model, testing the null hypothesis that the model is correct with p = .304. The same model was tested with diastolic BP and MAP, but no significant relationships were found between the assessed variables and these variables, as was expected from the correlations shown previously. The aim of this study was to carry out an analysis of the relationship between caregivers’ knowledge about AD, dysfunctional thoughts about caregiving, and experiential avoidance and blood pressure, after controlling for known predictors of cardiovascular health, drawing upon a hypothesis derived from the cognitive-behavioral model adapted to caregiving (Losada, Montorio, Knight et al., 2006). Our hypothesis suggesting an association between caregivers’ knowledge about AD, dysfunctional thoughts about caregiving and experiential avoidance is supported by the results: caregivers with less knowledge about Alzheimer’s report more dysfunctional thoughts and experiential avoidance. In addition, these three variables were found to be correlated with systolic blood pressure: less knowledge and more dysfunctional thoughts and experiential avoidance are associated with higher systolic blood pressure. The results of the tested model suggest that the association between knowledge about Alzheimer and blood pressure is not direct, but mediated through its effect on dysfunctional thoughts about caregiving and experiential avoidance. According to the model, caregivers with a lower level of knowledge about their relatives’ illness have higher scores on dysfunctional thoughts and experiential avoidance and, finally, higher systolic blood pressure. The results obtained are in line with previous studies in the association found between experiential avoidance (Spira, 2007), dysfunctional thoughts (Stebbins & Pakenham, 2001), and caregiver health. These findings thus provide support for the idea that dysfunctional thoughts and experiential avoidance are not only related to mental health problems (e.g., depressive symptomatology) in dementia family caregivers, but also to their physical health, specifically blood pressure. As far as we are aware, this is the first study to postulate an effect of this knowledge on caregivers’ ways of thinking, analyzing the joint effect of dysfunctional thoughts and experiential avoidance on blood pressure. The results of this study suggest that dysfunctional thoughts are associated with worse health outcomes in dementia caregivers, as it has been previously found in other populations (Ottaviani et al., 2016). In addition, this study addresses the potential association or effect that could exist between caregivers’ levels of dysfunctional thoughts and experiential avoidance that was previously suggested by Losada et al. (2014). The results suggest that there is a strong association between dysfunctional thoughts and experiential avoidance, and that some of the negative consequences of this variable on caregivers’ health could be potentially mediated by experiential avoidance. As Montorio et al. (2009) suggested, dysfunctional thought may be affecting caregivers’ health by preventing them from expressing emotional distress, as they may feel that it is not correct or respectful to complain or express any negative feeling related to care. It may be possible that caregivers with higher levels of dysfunctional thoughts may also be more prone to avoid such negative emotions and to try to convince themselves that they are not actually feeling such emotions. However, such degrees of denial, avoidance or emotion repression may be harmful for caregivers’ health, as suggested in this study. Such an association has been suggested with similar coping strategies, such as avoidant coping (Kim et al., 2007). In addition, this study also supports the idea expressed by the cognitive-behavioral model adapted to caregiving (Losada et al., 2006), that dysfunctional thoughts are related to cultural and contextual values, as suggested by the paths found between this variable and formal education, and more interestingly between dysfunctional thoughts and knowledge about Alzheimer’s disease. Formal education has been extensively studied in the caregiving context, suggesting that higher levels of education are associated with better physical health (Pinquart & Sörensen, 2007). Conversely, research conducted on knowledge about AD and caregivers’ health outcomes is very scarce. To our knowledge, only one study has analyzed these constructs together (Graham et al., 1997), suggesting that a lower level of knowledge is associated with higher levels of depressive symptoms. However, although these authors suggested that there could be a causal path between these two variables, they did not present any specific pathway. One potential pathway that we could suggest is that greater knowledge about the relative disease could help caregivers assess more precisely the capacities of their care-recipients. It has been suggested that caregivers who attribute a lower capacity to their relatives than the relatives perceive they have are the caregivers experiencing a higher level of burden (Izal et al., 2005). Consequently, it would make sense that caregivers with lowers levels of knowledge had poorer expectations for the functional capacities of their relatives, and could be increasing their frequency of dysfunctional thinking and avoidance of emotions, which could finally contribute to higher cardiovascular risk. However, as expectations and assessment of function of the care-recipient by the caregiver have not been assessed, further studies should be conducted to test this hypothesis, if possible, through longitudinal methodologies. Finally, it could be interesting to highlight that the associations tested were only found to be significant for systolic BP, but not for diastolic BP nor MAP. Although this is similar to what has been found in other studies, in which avoidant coping is only associated with systolic but not diastolic BP (Kim et al., 2007), no clear explanation has yet been found about why some variables are uniquely associated with one component of BP but not the other. Further studies should be conducted, not only in caregiving populations, to clarify how the different components of blood pressure and other cardiovascular outcomes react to emotional changes. This study has several limitations. First of all, the design of the study is cross-sectional, so the direction of the associations may not be the one presented in the model (e.g., those with more dysfunctional thoughts may not be likely to ask for information about the disease). Longitudinal and experimental studies are needed in order to confirm these results. Another limitation of this study is that resting blood pressure was not assessed prior to initiating the caregiver interviews. Instead, the three BP assessments by different evaluators were conducted prior to, during, and after completing the assessment interviews. Although the levels of BP found in this study are similar to other studies conducting a standardized measurement of BP (e.g., Chatillion et al., 2013), the procedure used in this study may have caused variation in blood pressure due to the potentially stressful nature of the questions being asked. Although we found no significant changes in BP over the interview, we still encourage caution when interpreting the obtained findings, and suggest that future studies assessing BP at rest do so prior to conducting any psychosocial assessments. Also, as in the original study (Carpenter et al., 2009), the scale used for measuring caregivers’ knowledge about AD has very low reliability. However, knowledge about AD is a complex and multifaceted variable, and most people non-professionally involved with AD are not familiar with many of its symptoms, nor with strategies to treat people with this illness. Most of them are familiar with some “tips or clues” about AD, but not with all of them. In this regard, Carpenter et al. (2009) suggested that the low reliability of the scale and its factors might be reflecting that “items were written to tap multiple facets of knowledge in people who themselves may have idiosyncratic information about AD” (p. 246), suggesting that participants may have their own bias and preconceived ideas about AD, based on their own personal experiences, which may be interfering with their knowledge about the disease. This is quite likely to be the case with dementia family carers. This fact, together with the true/false response option, as well as the lack of exhaustiveness of the scale (meaning that not all of the possible behaviors, symptoms and situations of the relative and the caregiving context may be represented in the scale), could explain why both studies (Carpenter et al.’s, 2009, and ours) find low reliability for this scale or its subscales. In addition, the high percentage of correct answers to our short version of the ADKS (66%) may be considered a potential limitation as it may not represent the reality of the Spanish caregivers’ population. However, this score is not far from the one found in the original study by Carpenter et al. (2009), who suggested that caregivers tend to show certain, although not perfect, degree of knowledge about their relatives’ disease. Another potential limitation could be related to the level of formal education reported by the participants in our study, that seems to be higher to levels reported in other studies carried out with Spanish samples. The obtained associations between educational level and knowledge about AD and dysfunctional thoughts may not be generalizable to other samples, and so the findings should be treated with caution. For example, in caregivers showing lower levels of formal education the contribution of knowledge about AD or dysfunctional thoughts to the explanation of experiential avoidance or blood pressure could be different. Another limitation that could be playing a role here is the potential overlapping of the measures of dysfunctional thoughts and experiential avoidance, given the high correlation coefficient between them. Finally, participants volunteered to take part in the study, which limits the generalizability of the results to other caregivers. Despite its limitations, this study is presented as a first and preliminary approach to the analysis of the associations between knowledge about AD, dysfunctional thoughts about caregiving, experiential avoidance, and blood pressure. Although the limitations recommend that the results be considered with caution, our findings suggest that caregivers with low levels of knowledge about AD may be more vulnerable to the effects of the caregiving process on their blood pressure than caregivers with more knowledge about AD. Although no clear path is stablished in the literature on how a lower knowledge about Alzheimer disease may contribute to higher CVD risk, the obtained associations in our study suggest a potential path relating a lower knowledge about AD with higher levels of dysfunctional thoughts and experiential avoidance related to caregiving situations. Previous research has suggested two paths through which experiential avoidance may contribute to the explanation of cardiovascular risk (Hildebrandt & Hayes, 2012): 1) by increasing the levels of autonomic function and 2) by contributing to worse patterns of health behaviors (e.g., alcohol consumption or binge eating; Kingston et al., 2010). Although these paths remain understudied in the context of dementia family caregiving, future studies should analyze the contribution of these two paths to the explanation of the associations found in this study. This analysis may contribute to clarifying how cognitive or cultural related variables may pave the way to the emergence of cardiovascular diseases. In light of these results, some clinical implications may be highlighted. Increasing the knowledge related to the identification of dementia symptoms and the management of these, through psycho-educational sessions or educational programs, for both family caregivers (e.g., Chien & Tann, 2019) and gerontology professionals (Imre et al. 2019) seems to be beneficial and recommended. It has been suggested that a greater satisfaction with information about a relative’s illness is associated with lower distress in critical patient family carers (Gómez-Carretero et al., 2009). Gerontology professionals working with dementia patients should try to transmit their knowledge about the illness (which has recently been suggested to be adequate, Imre et al. 2019) in a better and more efficient way to caregivers. Further, such educational sessions should be integrated in clinical interventions which may change caregivers’ maladaptive ways of thinking and coping, as the effect of this knowledge on caregiver health seems to be mediated by higher levels of dysfunctional thoughts and experiential avoidance. Increasing the availability of these interventions has been suggested as a way of raising the number of caregivers trained in strategies for coping with a role for which they have not been trained, in which the dementia illness is perceived as a threat that has a significant impact on both the caregiver and the care-recipient (Kovaleva et al., 2019). Finally, working not only with the way caregivers think (dysfunctional thoughts), but also with the acceptance of emotions and thoughts derived from the caregiving process (in contrast to the experiential avoidance coping strategy) (Kishita et al., 2018) may result in greater effects on caregivers’ health. Future studies are needed to confirm the findings shown in this study, which may be helpful in designing clinical interventions for supporting dementia family caregivers. In addition, further studies may analyze if these results are similar not only in other family caregiver populations, but formal caregivers as well. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgements We thank all the caregivers for their participation in the study and also the following centers for collaborating with us in the project: Fundación Cien, Fundación Maria Wolff, Centro de Salud General Ricardos, Centro de Salud García Noblejas, Centro de Salud Benita de Ávila, Centro de Salud Vicente Muzas, Centro Reina Sofía de Cruz Roja, Centro de Psicología Aplicada de la Universidad Autónoma de Madrid, and Servicios Sociales de Getafe. Cite this article as: Vara-García, C., Romero-Moreno, R., Márquez-González., Barrera-Caballero, S., Pedroso-Chaparro, M., & Losada-Baltar, A. (2021). Knowledge about Alzheimer’s Disease, Dysfunctional Cognition, and Coping on Caregiver’s Blood Pressure. Clínica y Salud, 32(2), 79-87. . https://doi.org/10.5093/clysa2020a33 Funding: The preparation of this paper was supported in part by grants from the Spanish Ministry of Economy and Competitiveness under grants PSI2012-31239 and PSI2015-65152-C2-1-R, and by the Comunidad Autónoma de Madrid, through a pre-doctoral scholarship for the first author of this work. Samara Barrero was supported by a FPU grant from the Spanish Ministry of Education, Culture and Sport. References |
Cite this article as: Vara-García, C., Romero-Moreno, R., Márquez-González, M., Barrera-Caballero, S., Pedroso-Chaparro, M. D. S., and Losada-Baltar, A. (2021). Associations of knowledge about AlzheimerŌĆÖs disease, dysfunctional cognition, and coping with caregiverŌĆÖs blood pressure. Cl├Łnica y Salud, 32(2), 79 - 87. https://doi.org/10.5093/clysa2020a33
carlos.vara@urjc.es Correspondence: carlos.vara@urjc.es (C. Vara Garc├Ła).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 CrossRef
CrossRef JATS
JATS