
Mental Illness Stigma. A Comparative Cross-sectional Study of Social Stigma, Internalized Stigma and Self-esteem
[El estigma de la enfermedad mental. Estudio comparativo transversal del estigma social, el internalizado y la autoestima]
Clara González-Sanguino1, Sara González-Domínguez1, 2, Miguel A. Castellanos1, and Manuel Muñoz1
1Complutense University of Madrid, Spain; 2CRPS Mart├şnez Campos, Universidad Cardenal Cisneros, Madrid, Spain
https://doi.org/10.5093/clysa2021a16
Received 29 September 2020, Accepted 20 April 2021
Abstract
The aim of this study was to explore the role of stigma in different diagnoses of mental illness. A cross-sectional study (N = 255) was developed in two groups: users of a rehabilitation network for people with severe mental illness (Group-I) and people with common diagnoses in an ambulatory psychiatric service (Group-II). Internalized stigma, social stigma, self-esteem, and sociodemographic variables were measured. Mean comparisons, ANOVAs, and independent linear regression models were carried out. Similar overall scores were obtained for the internalized stigma, but Group-I reported more discrimination and resistance to stigma and also had less social stigma. The regression model for Group-I revealed social stigma and self-esteem as predictors, while in Group-II only self-esteem was significant. The study reveals differences in internalized stigma according to the care resource and diagnoses, suggesting different intervention lines and underlining the importance of further research on this topic.
Resumen
El objetivo de este estudio ha sido explorar el papel del estigma en los diferentes diagnósticos de la enfermedad mental. Se llevó a cabo un estudio transversal (N = 255) en dos grupos: usuarios de una red de rehabilitación para personas con enfermedad mental grave (grupo I) y personas con diagnósticos comunes en un servicio psiquiátrico ambulatorio (grupo II). Se midió el estigma internalizado, el social, la autoestima y las variables sociodemográficas. Se llevaron a cabo comparaciones medias, ANOVA y modelos de regresión lineal independientes. Se obtuvieron puntuaciones generales similares para el estigma internalizado, pero el grupo I manisfestó más discriminación y resistencia al estigma y también menor estigma social. El modelo de regresión para el grupo I mostró como predictores el estigma social y la autoestima, mientras que en el grupo II sólo la autoestima era significativa. El estudio muestra diferencias en el estigma internalizado según el recurso de atención y los diagnósticos, lo que sugiere diferentes líneas de intervención y subraya la importancia de seguir investigando en este tema.
Palabras clave
Estigma internalizado, Estigma social, Autoestima, Enfermedad mental grave, Psicosis, Depresi├│n, AnsiedadKeywords
Internalized stigma, Social stigma, Self-esteem, Severe mental illness, Psychosis, Depression, AnxietyCite this article as: González-Sanguino, C., González-Domínguez, S., Castellanos, M. A., & Muñoz, M. (2022). Mental Illness Stigma. A Comparative Cross-sectional Study of Social Stigma, Internalized Stigma and Self-esteem. Cl├şnica y Salud, 33(2), 59 - 64. https://doi.org/10.5093/clysa2021a16
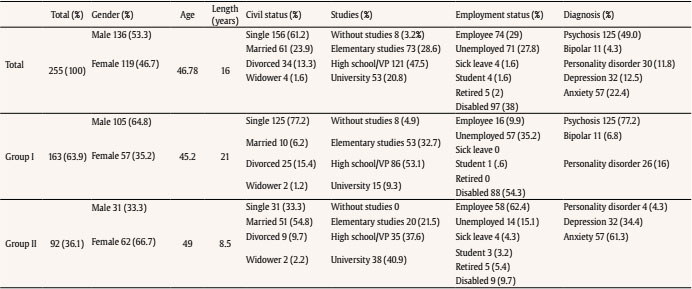
clagon06@ucm.es Correspondence: clagon06@ucm.es (C. Gonz├ílez-Sanguino)Stigma associated with mental illness includes stereotypes, prejudices, and negative behaviours towards people suffering psychological problems (Ottati et al., 2005). This means the existence of beliefs about the lack of ability or skills as well as judgments of dangerousness and unpredictability that generate negative emotional reactions, which often end up being translated into acts of discrimination against these persons (Corrigan & Watson, 2002). In relation to this construct it is necessary to differentiate three levels (Livingston & Boyd, 2010): a first structural level, referring to laws and institutions; a second level with social or public stigma, which refers to the stereotyped beliefs and discriminatory behaviours of the general population towards people who suffer these problems; and finally, a third level involving internalized stigma (IS), referring to the stigma felt by each person. The IS arises when a person with mental health problems accepts the stereotypes and beliefs that society shares and applies them to him/herself. Internalized stigma is also known as perceived stigma (knowledge of stereotypes about disease) (Ertugrul & Ulug, 2004) or experienced stigma (direct suffering from experiences of discrimination) (Link et al., 2001). Among others, several models highlight as relevant factors for the formation of IS the existence of previous social stigma and experiences of discrimination, self-concept, coping style, and even self-judgmental emotional reactions (Muñoz et al., 2011; Vauth et al., 2007; Yanos et al., 2011). Regarding the prevalence of IS in people with psychological problems, few studies carried out on a large scale provide data on the subject, highlighting a European study, in which around 15% of people diagnosed with various pathologies (from schizophrenia to anxiety) showed IS (Alonso et al., 2009). It should be noted that most studies are carried out on samples in which the main diagnosis is severe mental illness (SMI) (Del Rosal et al., 2020), with a prevalence of the IS between 30% and 41.7% (Livingston & Boyd, 2010). However, studies with samples with other types of pathologies, such as depression or anxiety, are less frequent and the existing research show that internalized stigma is present in around 22.1% and 11.7%, depending on the country of origin (Alonso et al., 2008). In addition, it is necessary to highlight the importance of the IS due to its relationship with other clinically relevant variables. On the one hand, research focused on people with SMI shows an IS relationship with lower satisfaction in social relationships (Oliveira et al., 2015), worse quality of life and self-esteem (Vrbova et al., 2017), worse adherence to treatment (Çuhadar & Çam, 2014), and worse recovery (Kim et al., 2015). On the other hand, studies with people with depression or anxiety problems find correlations between IS and levels of anxiety and depression (Ociskova et al., 2014), correlation with lower self-esteem (Oliveira et al., 2015), worse adherence to treatment (Sedlácková et al., 2015), and in general the relationship of IS with poorer quality of life and subjective well-being (Oliveira et al., 2015). In studies carried out with samples in which all types of psychological problems were included (diagnoses of both psychosis and anxiety, depression or personality disorders), relations are found between IS and number of hospitalizations and severity of the disorder (Grambal et al., 2016), as well as the importance of its relationship with self-esteem (Picco et al., 2017). The differentiation between SMI and other disorders also often leads to differences in the type of therapeutic and psychiatric care. From the 1950s onwards, with the start of the psychiatric reformation, rehabilitation resources began to be created to cover the specific needs of people with SMI, and often these people were attended in day centres and psychosocial or occupational rehabilitation centres. However, “more common” diagnoses are usually treated through psychological or psychiatric outpatient consultations, being unusual for people affected, for example, by an anxiety disorder, having specific resources available. The relevance and usefulness of rehabilitation networks are well established (Rössler, 2006), although the role it can play in variables such as IS associated with mental illness is unknown, with few studies comparing this variable according to the type of care resource people attend. The present paper focuses on IS and its relationship with variables proved relevant in previous studies in two different groups: one formed by people diagnosed with SMI who were users of the psychosocial rehabilitation network and another made up by people with diagnoses of anxiety and depression attended in outpatient hospital consultations. Our main aim is to explore how the stigma of these diagnoses is and whether a difference exists between the two groups. Procedure Upon approval by the ethics and research committees of the different rehabilitation centres, the hospital psychiatry service and the university, all participants were informed in writing of the purpose of the research and completed an informed consent. They were briefed by the professionals who regularly treated them on the existence of the study and the possibility of participation. Evaluations were subsequently conducted through individual interviews. All procedures performed in the study were in accordance with the ethical standards of the ethics and deontology committee of the university and centers and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Participants A convenience sample (N = 255) was used to select two groups of participants throughout 2017-2020. On the one hand, users of the psychosocial rehabilitation network diagnosed with SMI (Group-I, n = 163) and, on the other hand, people with diagnoses of anxiety and depression who were attended in an ambulatory outpatient psychiatric service of a hospital consultation (Group-II, n = 92). The users of the rehabilitation network were recruited from the different resources that compose it: psychosocial rehabilitation centres (n = 46), day centres (n = 34), labour rehabilitation centres (n = 32), people in care by socio-community support teams (n = 14), mini-residences, and supervised apartments (n = 36). The inclusion criteria for Group-I were: age between 18 and 67 years, having a severe and long-lasting mental disorder (schizophrenia, manic-depressive disorder, severe and recurrent depressive disorder, paranoid disorders, and other psychoses) with disability and difficulty in community integration. The following exclusion criteria were established: acute psychotic symptoms, severe cognitive impairment and manic and/or agitated states that prevented the completion of the evaluation protocol. For Group-II the inclusion criteria were: age between 18-67 years and to be receiving treatment in the external consultations of the psychiatry service. The exclusion criteria established were: to have a serious and lasting mental disorder, severe cognitive impairment, to present as the main pathology the consumption of substances and/or manic or agitated states that prevented the completion of the evaluation. Variables and Instruments The variables and instruments used are detailed below. Sociodemographic variables. Using a personalised data sheet, the following variables were collected: age, gender, civil status (married, single, divorced, widowed), last studies undertaken (without studies, elementary studies, high school/vocational training-VT, university), occupation (employee, sick leave, unemployed, disabled, retired), diagnosis (psychosis, bipolar, personality disorder, depression and anxiety). Self-esteem was evaluated with the Rosenberg Self-esteem Scale (RSE) (Rosenberg, 1965). This questionnaire is used to explore personal self-esteem understood as feelings of personal worth and self-respect. It consists of 10 items with Likert format in which high scores indicate a higher self-esteem. Cronbach α = .84. Social stigma was measured by the Attribution Questionnaire-9 (AQ-9) (Corrigan et al., 2014). A Spanish version of the 9-item Attribution Questionnaire-9 was used (Muñoz et al., 2015). It evaluates a series of constructs that explain attitudes, affections, and behaviours related to a hypothetical person suffering from mental illness. In this case a person’s neutral description was chosen. Then 9 items were included in a Likert format with 9 response alternatives ranging from not at all to very much. The questionnaire consists of the following factors: pity, dangerousness, fear, blame, segregation, anger, help, avoidance, and coercion. The higher the score, the more stigmatising the person has. Cronbach α = .66. Internalized stigma was measured by the Spanish adapted version of the Internalized Stigma of Mental Illness (ISMI) (Ritsher & Phelan, 2004), a scale that evaluates the subjective experience of stigma or internalized stigma by those with mental illness. It consists of 29 items in Likert format. They are grouped in 5 factors: alienation, stereotype endorsement, discrimination, social withdrawal, and stigma resistance. A cut-off of 2.5 is suggested to be an indicator of presence or absence of stigma (Ritsher & Phelan, 2004). Cronbach α = .82. Analysis Comparisons of means were carried out with Student t-tests and ANOVAs of independent samples in the two groups of the sample, according to the different variables collected. The Bonferroni test was used as a post hoc comparison. In order to test the relationship between IS, SS, and self-esteem, independent linear models were carried out for each group of the first variable over the other two. Models were adjusted for least squares and the definitive model was established by contrasting models that are based on the significant increase in R2. Compliance with the assumptions was assessed by visual inspection of the linearity, normality, and homogeneity of wastes. The results provide correlation matrices for both studies and the values of the coefficients of definitive models, with their contrasts and R2 values. All analyses were conducted using R version 3.1 (R Core team, 2015). Description of the Sample The total sample was gender-balanced, with an average age of 46.78 years and with predominant diagnoses of psychosis (49%) and anxiety (22.4%). In Group-I the number of men represented the majority (64.8%), and the main diagnosis found was psychosis (77.2%), along with personality disorders (16%), with an average duration of the disorder of 21 years. In this group the majority of subjects were single (77.2%) or divorced (15.4%), and with mostly elementary studies (32.7%) or high school/VT (53.1%). Regarding occupation, most subjects showed an incapacity that made it impossible for them to work (54.3%), finding a small percentage of employed persons (9.9%). Conversely, in Group-II, women were in the majority (66.7%) with main diagnoses of anxiety (61.3%) along with depression (34.4%), with an average duration of the disorder of 8.5 years. Most of the subjects were married (54.8%) and had university studies (40.9%), as well as the majority were working (62.4%). A detailed description of age, gender, civil status, duration of disorder, studies, occupation, and type of diagnosis of participants can be seen in Table 1. Internalized Stigma Total scores were slightly higher in Group-I, although these differences were not statistically significant. However, there were significant differences in ISMI factors of “discrimination” and “non-resistance to stigma”, with higher scores in Group-I, t(253) = 2.08, p < .05, η2 = .16; t(253) = -3.8, p < .00, η2 = .20. Other differences in the ISMI based on socio-demographic variables such as occupation, gender or marital status were not found. Social Stigma In relation to stigmatizing attributions we found significantly lower scores in Group-I with respect to Group-II, t(253) = -7.55, p < .00, η2 = .18. These significant differences were observed in all factors of the questionnaire except for “fear”, “segregation”, and “coercion”. Self-esteem No significant differences were found in Group-I and II, although Group-II had lower scores. In Table 2 the scores and analysis results may be observed. Table 2 Instruments and Scores  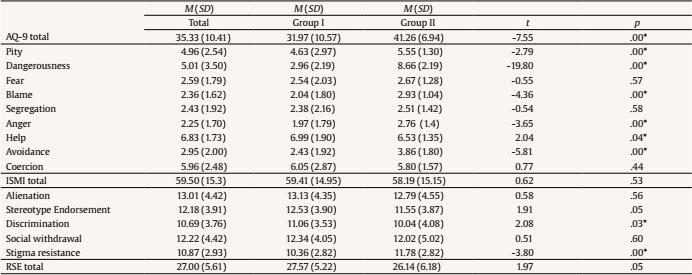 Note. M = mean; SD = standard deviation; AQ-9 = attributional questionnaire; ISMI = internalized stigma of mental illness scale. *p < .05. Relation between IS and Other Variables In Group-I, both social stigma and self-esteem were found to be significant (both with p < .001), jointly explaining 50% (R2 = .50) of the variability of IS. For Group-I the only significant variable was self-esteem (p < .01) while the SS was not significant (p = .473). Although self-esteem was significant, this variable only accounts for 7% of the stigma variability (R2 = .07). The visual inspection of the residues offered a reasonable fulfilment of the assumptions. The results described can be seen in Table 3. Table 3 Regression Results   Note. β = beta; SE = standard error; R2 = regression coefficient; RSE = Rosenberg Self-esteem Scale; AQ-9 = Attribution Questionnaire 9. *p < .05, **p < .01, ***p < .001. The obtained results reveal the presence of IS in the whole sample, with slightly higher IS scores in Group-I, even though these differences were not statistically significant. These results are similar to other studies where the presence of moderate IS is also observed throughout the sample, but significant differences in IS scores were normally found in these studies, with more IS in people who had a diagnosis of SMI (Alonso et al., 2008; Holubova et al., 2018; Karidi et al., 2015; Maharjan & Panthee, 2019). In relation to these results we consider important to highlight that, although total scores are not significantly different, the answers in the ISMI subscales indicate that IS in both groups is not equal. Scores in Group-I are considerably higher for the behavioural dimension of reported discrimination and a greater resistance to stigma compared with Group-II. These results are consistent with previous literature, where higher levels on the discrimination dimension of the ISMI have also been found in people with SMI versus other diagnoses (Fadipe et al., 2018; Ran et al., 2017; Szczesniak et al., 2018). These findings emphasize discrimination against people with SMI, which may be due to the fact that schizophrenia and similar diagnoses are associated with more stigmatising attributions, such as inability to recover, blame, and stereotypes (Wood et al., 2014), and therefore people show greater desire for social distance (Utz et al., 2019), which often ends up in more negative behaviours towards these people. The effects of discrimination are numerous, including increased time in accessing health care resources (Gronholm et al., 2017; Kular et al., 2019), and even in relation with depressive symptomatology and a longer disease duration (Pellet et al., 2019). On the other hand, Group-I also shows greater stigma resistance compared with Group-II. This means that people with SMI are more able to resist, counteract, or otherwise remain unaffected by the stigma of mental illness. Additionally, stigma resistance has been shown to be related with higher self-esteem (Brohan et al., 2011), which is consistent with the results obtained in our study, where Group-I also revealed more self-esteem than Group-II. The fact that people with SMI exhibit more resistance to stigma, despite being more discriminated against and having slightly higher scores in the total IS, although it may seem paradoxical, might be explained by social experiences and socio-demographic characteristics. Group-I people, mostly with longer and more serious problems, single, declared disabled, and unemployed, have had experiences that favour the acceptance of certain stereotypes. However, they also seem to have learned and implemented more strategies to combat the phenomenon and to be less affected. In addition, the type of care resource can also be a key factor in IS. More interventions focused on providing coping skills to fight stigma are common in rehabilitation resources, while in regular outpatient psychiatry sessions care tends to be directed towards more symptom-focused therapies. On the other hand, it is also understandable that Group-II, who has not experienced so many discriminations, has less in mind and makes less effort not to be identified with stigmatizing stereotypes. However, rehabilitation resources can also have a negative side, since the simple fact of being referred to one of them can be experienced as stigmatizing, just as it is more likely that by going to these centres and being labelled as a person with SMI more experiences of discrimination can occur, even though these resources provide more strategies to fight IS, according to the results. In relation to other variables studied, we highlight the differences between both groups in social stigma, finding that Group-I shows fewer stigmatizing attitudes than Group-II in all dimensions, except for fear, segregation, and coercion. This may be due to the fact that the subjects of Group-I in their care resource coexist daily with people with different psychiatric diagnoses and identify themselves as part of that group, so it is coherent that they show fewer stigmatizing attitudes, supporting the hypothesis of social contact to reduce social stigma (Corrigan, 2005). Regression models are useful to know which variables predict stigma depending on the type of group. Tests were carried out with all the variables of the study, with the models presented being those that provided the best results when explaining IS. While for Group-I both self-esteem and stigmatising attributions seem to predict IS, explaining 50% of variability, for Group-II only self-esteem was significant, explaining only 7%. Although the importance of stigmatizing attitudes and self-esteem in relation to IS is consistent with several previous studies (Holubova et al., 2018; Picco et al., 2017), the difference in both models predicting IS is novel and highlights the need for more research on people who present common problems and seek treatment in general resources. On the other hand, these differences in predicting internalized stigma may also be due to the close relationship between different symptomatology, such as the presence of psychotic experiences and a poorer quality of life, which is common in people with SMI (Holubova et al., 2018). Thus, López-Navarro et al. (2018) also account for the close relationship between psychotic experiences and quality of life associated with social relationships, which probably has a close relationship with internalized stigma. Differential models explaining IS depending on the type of care resource attended and diagnoses, and knowing how IS is in this different groups, might also be useful to implement better intervention strategies to reduce IS. Programs focused on improving stigma coping skills may be more effective in anxiety and depression diagnoses in general outpatient care, but focus on the cognitive or emotional dimensions of stigma may be more beneficial in rehabilitation resources, as they already seem to have more resistance to stigma. On the other hand, interventions that address self-esteem may be positive for both groups, as it is a predictor variable in both cases. Regarding social stigma, the various existing campaigns at a social level could increase efforts to address discrimination suffered by people who attend rehabilitation resources, as we know that it is greater than that suffered by people who attend other types of outpatient clinics. Furthermore, in relation to discrimination and stigma suffered by people with SMI, it would also be particularly interesting to make an effort to modify causal attributions about the origin of psychological problems of professionals and the general population, where biological explanations alone are associated with a greater chronicity of the problem, and in comparison with the general population, professionals have a better perception of psychological problems (Castro-de Diego & Vicente-Colomina, 2019). Limitations in our study include lack of gender balance in both groups (although this may be representative of gender characteristics in each group). In addition, in the recruitment of the sample, only those people who wanted to do it voluntarily participated, maybe creating a bias in the sample. Regarding method, it was cross-sectional, so it is not possible to establish causal relationships. Furthermore, we consider that including variables such as quality of life or disorder severity would have been interesting when explaining IS in the second group, taking this into account for future lines of research. In accordance with the aforementioned, our study shows differences in content and formation of IS in two well-differentiated groups, one with SMI treated in rehabilitation services and the other with common diagnoses, attended in an outpatient clinic of a psychiatric service. This research highlights the difference in IS depending on the type of care resource and diagnoses, suggesting different lines of intervention in preventing and reducing IS, as well as underlines the need for further specialized study related to stigma in common diagnoses not attended by specialized resources, which, in the long term, will allow more effective interventions on IS. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgment Our acknowledgement to the Management of Social, Educational and Professional Services (Group 5), and San Telmo University Hospital Complex for providing the sample of participants. Cite this article as: González-Sanguino, C., González-Domínguez, S., A. Castellanos, M., & Muñoz M. (2021). Mental illness stigma. A comparative cross-sectional study of social stigma, internalized stigma and self-esteem. Clínica y Salud, 33(2), 59-64. https://doi.org/10.5093/clysa2021a16 Funding: This research was supported by the UCM-Santander financing predoctoral grant (CT42/18-CT43/18). References |
Cite this article as: González-Sanguino, C., González-Domínguez, S., Castellanos, M. A., & Muñoz, M. (2022). Mental Illness Stigma. A Comparative Cross-sectional Study of Social Stigma, Internalized Stigma and Self-esteem. Cl├şnica y Salud, 33(2), 59 - 64. https://doi.org/10.5093/clysa2021a16
clagon06@ucm.es Correspondence: clagon06@ucm.es (C. Gonz├ílez-Sanguino)Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







