
Stigma towards Child and Adolescent Mental Health Problems among Fathers and Mothers. A Cross-sectional Study
[El estigma de los padres y madres hacia los problemas de salud mental de niños y adolescentes. Un estudio transversal]
Beatriz Moreno-F. Ramiro1, Sara González Domínguez1, and Clara González-Sanguino2
1Cisneros Higher Education Center, Division of Psychology, Madrid, Spain; 2Psychology Department, University of Valladolid, Spain
https://doi.org/10.5093/clysa2024a8
Received 14 March 2023, Accepted 15 December 2023
Abstract
Background: Stigma toward child and adolescent mental health problems among parents has been understudied, despite its importance. Method: Sociodemographic variables, stigma associated with mental health problems in childhood and adolescence, myths about suicide, familiarity with mental health, and seeking professional help were assessed in a cross-sectional study in a Spanish sample (N = 268). Descriptive analyses, mean difference and regression models were carried out. Results: The results reveal medium levels of stigma, the presence of myths about suicide and average familiarity with mental health. Mothers and a higher level of education, showed lower levels of stigma and fewer myths about suicide. A regression model explains the 44% of the variance with myths about suicide, stigma and familiarity with mental health as predictors of seeking professional help attitudes. Conclusions: Stigma, myths surrounding suicide, and parental unfamiliarity with mental health may act as barriers to appropriate diagnosis and treatment. Practical implications and recommendations are discussed.
Resumen
Antecedentes: La estigmatización de los problemas de salud mental en niños y adolescentes en los padres y madres no se ha estudiado lo suficiente a pesar de su importancia. Método: Se evaluaron variables sociodemográficas, el estigma asociado con los problemas de salud mental en la infancia y la adolescencia, mitos sobre el suicidio, conocimiento de la salud mental y la búsqueda de ayuda profesional en un estudio exploratorio transversal en una muestra española de padres y madres (N = 268). Se realizaron análisis descriptivos, de diferencia de medias y modelos de regresión. Resultados: Los resultados revelan un nivel medio de estigma, la presencia de mitos sobre el suicidio y un conocimiento medio con la salud mental. Las madres y un mayor nivel educativo mostraron menores niveles de estigma y menos mitos sobre el suicidio. El 44% de la varianza de la búsqueda de ayuda profesional se explica a través de los mitos sobre el suicidio, el estigma y el conocimiento de la salud mental como predictores de las actitudes de búsqueda de ayuda profesional. Conclusiones: Se establecen recomendaciones prácticas, subrayando cómo el estigma, los mitos sobre el suicidio y la falta de conocimiento de los progenitores de la salud mental pueden actuar como barreras para un diagnóstico y tratamiento adecuados. Se discuten las implicaciones prácticas y las recomendaciones.
Palabras clave
Estigma, Padres, Salud mental, Niños, AdolescentesKeywords
Stigma, Parents, Mental health, Children, AdolescentsCite this article as: Ramiro, B. M., Domínguez, S. G., & González-Sanguino, C. (2024). Stigma towards Child and Adolescent Mental Health Problems among Fathers and Mothers. A Cross-sectional Study. ClĂnica y Salud, 35(1), 27 - 33. https://doi.org/10.5093/clysa2024a8
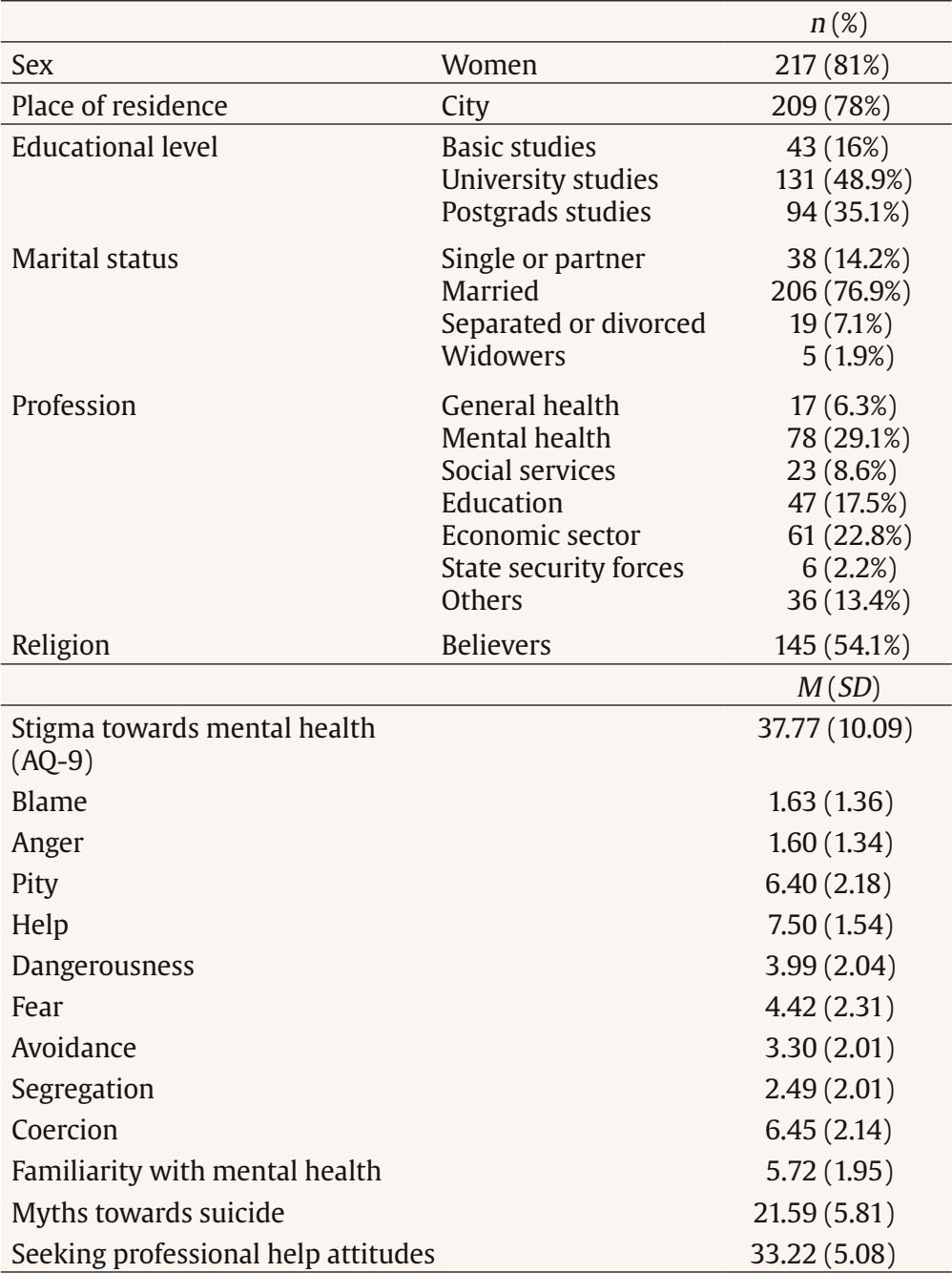
Correspondence: Clara.gonzalez.sanguino@uva.es (C. González-Sanguino).The stigma towards mental health problems (MHP) refers to the prejudices, stereotypes, and discrimination that exist in society towards people with those problems (Corrigan & Watson, 2002). In recent years, research on social stigma has increased notably, revealing that beliefs of dangerousness, unpredictability, and guilt are common, as well as a general lack of knowledge about MHP (Huang et al., 2019; Li & Reavley, 2020). In addition, stigma may also be a barrier to secondary prevention in obtaining specialized psychological or psychiatric care, preventing access at institutional, community, and individual levels (Henderson et al., 2013), which results in delays in seeking PH interrupted treatment and generally poorer quality of care (Knaak et al., 2017). In children and adolescents, the prevalence of MHP ranges between 17% and 26% (Amerian Psychiatric Association [APA, 2013]), being necessary to highlight the enormous psychological impact that the Covid-19 pandemic has had on the young population (Panchal et al., 2021), as well as recording alarming increases in suicide rates (Mayne et al., 2021). In this population, stigma also has negative effects, finding that children and adolescents often feel rejected, have feelings of shame or guilt and try to keep their problems hidden by not seeking PH (Ferrie et al., 2020). In this context children and adolescents appear to be a particularly vulnerable group. Therefore, progenitors are of vital importance, since as primary caregivers and socializing agents they can have a strong influence on the approach and management of their children’s MHP (Sayal, 2006; Stiffman et al., 2004). Parental negative attitudes have been found to affect the stigma that children may experience (Ferrie et al., 2020), determining negative beliefs towards taking medication or affecting self-labelling as “crazy” or “psychopathic” by family role models (Kranke et al., 2010), linking positive family beliefs to lower stigma in children (Moses et al., 2009). However, despite the importance of attitudes towards mental health in fathers and mothers, few studies have focused on stigma among them. The research on the subject has found that, in general, when adults are asked about stigma in childhood, attitudes are negative. Pescosolido et al.(2007) found that 45% of their sample of more than 1,300 people from the general population, thought that a child with MHP would be ostracized at school, or would suffer in the future if someone else found out that they had MHP, with 36% of people saying that a parent would feel like a failure if their child had to receive psychological treatment. In studies conducted directly with parents, we found that progenitors of children with developmental disorders or MHP report higher levels of shame and stigmatization, and perceive the stigma associated with these problems as a source of chronic stress (Song et al., 2018). Another study shows the mediating role of parental self-stigma between insight and parental stress (Hasson-Ohayon et al., 2012). On the other hand, Villatoro et al. (2018) showed how stigma can bias recognition of mental illness, finding that greater stigmatizing beliefs mean a lower likelihood of believing that a child may have a mental health problem. These findings are in line with those found by Chavira et al. (2017), who found that around 40% of parents interviewed in their study report anxiety-related stigma in children, identifying it as a barrier to the use of mental health services. Also, a study of Polaha et al. (2015) found that higher parental perception of stigma was associated with lower willingness to seek services in a mental/behavioral health centre or in schools. A special mention should be made of suicide-related stigma, where, so far, work addressing stigma directly related to suicide is scarce (Zamorano et al., 2022). Existing assessment instruments determine the consequences for the occurrence of suicide, the opinion on assisted suicide, the rights of individuals, training, and the work of professionals in adult population (Eshun, 2006; Lee et al., 2007; Ouzouni & Nakakis, 2009; Renberg & Jacobsson, 2003). However, they do not include the most frequent myths about suicide (Eshun, 2006; Lee et al., 2007; Ouzouni & Nakakis, 2009; Renberg & Jacobsson, 2003). It is possible to cite a single study, as far as we are aware of, where stigma towards their children’s suicidal behavior was assessed in 103 parents, detecting how attitude towards psychiatric help and stigma in depression directly and indirectly influenced children’s depression (Jeong & Park, 2020). Considering the above, our main hypothesis is that the stigma related to child and adolescent MHP exists among both fathers and mothers, and that it may act as a barrier to seeking specialized professional care. In response to this hypothesis, an exploratory cross-sectional study is conducted in a sample of parents to describe and relate attitudes toward mental health in children and adolescents along with myths associated with suicide in this population, familiarity with mental health, and potential professional help-seeking. Procedure After approval by the university ethics committee and prior to data collection, all participants were informed in writing about the characteristics of the study and the voluntary nature of their participation by completing the informed consent form. Subsequently, the assessments were carried out individually using the Google Forms tool. The average time to complete the evaluation was 10 minutes. Participants The final sample, obtained by the snowball method, consisted of 268 participants from the general population in Spain. Participants were recruited through various social media networks (WhatsApp, email, Facebook, Twitter). Since the interest was to recruit fathers and mothers of children and adolescents, the legal age of the children was the main inclusion and exclusion criterion. In Spain, the legal age is 18 years, which is also considered the approximate limit between adolescence and young adulthood. Inclusion criteria were: a) being of legal age themselves (over 18 years) and b) having at least one minor child (under 18 years) at the time of the assessment. Exclusion criteria: a) having children of legal age (over 18). Variables and Instruments Sociodemographic Variables Ad hoc questions were developed to collect data on age, sex (male, female), educational level (basic, university, postgraduate), profession (general health, mental health, social services, education, economic sector, state or security forces, others), marital status (single or partner, married, separated or divorced, widowers), place of residence (city vs. rural places), and religion (believer in any religion vs. non-believer). Psychosocial Variables Stigma towards Mental Health in Childhood and Adolescence. It was measured through the Attribution Questionnaire-9 (AQ-9; Corrigan et al., 2014) in its Spanish version of 9 items (Muñoz et al., 2015). This instrument assesses stigmatizing attributions about mental illness through questions that follow a vignette with a mental health problem case example. The vignette in this case included the description of a mental health problem in a minor (age limit between childhood and adolescence) attending a regular school with MHP who has visited a hospital care unit in the past. The scale consists of 9 Likert-formatted items with 9 response alternatives ranging from not at all to very much. The questionnaire consists of the following factors: blame, anger, pity, help, dangerousness, fear, avoidance, segregation, and coercion. The higher the score, the more stigmatizing the attributions. Cronbach’s α = .76. Myths about Suicide Noting the lack of tools describing myths about suicide (Eshun, 2006; Lee et al., 2007; Ouzouni & Nakakis, 2009; Renberg & Jacobsson, 2003), 12 questions were developed that included the most frequent myths according to the literature: “most suicides happen suddenly without prior warning” (Castellvi & Piqueras, 2018; Martín, 2016); “whoever commits suicide is brave” (Martín, 2016; Montés et al., 2019; Piedra et al., 2019); “people who talk about suicide will not attempt suicide or will not commit suicide” (Dumon & Portzky, 2014; Martín, 2016; Piedra et al., 2019); “everyone who attempts suicide has depression” (Castellvi & Piqueras, 2018; Martín, 2016; Piedra et al., 2019); “genetic predisposition alone does not determine whether a suicide attempt is made” (Martín, 2016; Montés et al., 2019; Piedra et al., 2019); ”people who attempt suicide do not want to die, they only brag about it or try to draw attention to themselves” (Castellvi & Piqueras, 2018; Martín, 2016; Piedra et al., 2019); “suicide cannot be prevented” (Castellvi & Piqueras, 2018; Dumon & Portzky, 2014; Piedra et al., 2019); “anyone who commits suicide is a coward” (Martín, 2016; Montés et al., 2019; Piedra et al., 2019); “anyone who has ever attempted suicide will never stop trying” (Castellvi & Piqueras, 2018; Organización Mundial de la Salud [OMS], 2014), “a person who attempts suicide is determined to die” (Castellvi & Piqueras, 2018; OMS, 2014); “talking about suicide openly and honestly can give the person the possibility to consider other options or the time to think about their decision” (Dumon & Portzky, 2014; Piedra et al., 2019); and “one does not necessarily have to have a mental disorder to make a suicide attempt” (Montés et al., 2019; Piedra et al., 2019). The items were Likert-type with 4 response alternatives ranging from strongly disagree to strongly agree. The higher the score, the more myths towards suicide are detected. Cronbach’s α = .79. Attitudes towards Seeking Professional Help Assessed through the Attitudes toward Seeking Professional Psychological Help Scale-Short Form (ATSPPH-S; Elhai et al., 2008). It explores the importance and usefulness that the person (in this case a father or a mother) finds in the use of psychological services. It consists of 10 items, with a Likert-type scale response with 4 response alternatives ranging from strongly disagree to strongly agree (1-4). Several items were adapted to make reference to seeking PH for a child. The higher the score, the more help-seeking. Cronbach’s α = .81. Familiarity with Mental Health It was assessed with the Level of Familiarity Questionnaire (Corrigan et al., 2001). This questionnaire, through 11 dichotomous (yes/no) response situations, assesses the degree of familiarity that a person has with others who have a mental disorder. The higher the score, the higher the level of contact with people with mental illness. Cronbach’s α = .61. Analysis For the description of the sample, different descriptive statistics, means, standard deviations, frequencies, and percentages were estimated. Means comparisons were performed with Student’s t-tests, and ANOVA of independent samples in the different groups were carried out. The Bonferroni test was used as a post hoc comparison. To test the relationship between the quantitative variables in the study, Pearson correlations were conducted. To identify predictors of the help-seeking variable, a stepwise multiple regression analysis was performed with the total help-seeking score as the criterion variable and variables that were hypothesized to predict help-seeking and that showed significant correlations with the Help-Seeking Questionnaire (ATSPPH-SF) as predictors. All statistical analyses adopted a significance level of .05 and were conducted using SPSS statistical processing software version 25.0. Socio-demographic Characteristics of the Sample The sample consisted of a majority of mothers (81%) with a mean age of 42 years (SD = 7.45). Most people lived in a city as opposed to rural areas (78%), married or in a couple (91%) and with university or postgraduate studies (84%). The majority of the sample showed religious beliefs (54%), with a variety of professional areas. In Table 1 these results can be seen in detail. Stigmatizing Attributions to MHP Regarding stigma, the results show average levels of stigma in the sample towards MHP in childhood and adolescence (M = 37.77, SD = 10.09). When analyzing each subscale of the questionnaire, we found that the most stigmatizing attributions have to do with “help” (M = 7.50, SD = 1.54), followed by “coercion” (M = 6.45, SD = 2.14) and in third place “pity” (M = 6.40, SD = 2.18). The least stigmatizing attributions refer to “anger” (M = 1.60, SD = 1.34), then “blame” (M = 1.63, SD = 1.36), and the third least stigmatizating is “segregation” (M = 2.49, SD = 2.01). Furthermore, we found significant differences in relation to gender identity, with the highest presence of stigma in the group of men, t(266) = - 5.56, p < .001, np2 = .10. Likewise, in relation to religion, where believers have greater stigma towards mental health, t(266) = 2.26, p > .001, νp2 = .01. There were also differences according to educational level, F(2, 265) = 8.11, p < .001, ηp2 = .06, with post hoc analyses revealing significant differences between the group with the lowest educational level and those with postgraduate studies (p < .001). On the other hand, significant differences were observed according to profession, F(6, 261) = 8.39, p < .001, ηp2 = .16. Post hoc analyses show significant differences when comparing mental health and social service professionals with those in education (p < .001) and business (p < .001). These results can be observed in detail in Table 2. Table 2 Stigma towards Mental Health and Familiarity in Relation to Sociodemographic Variables  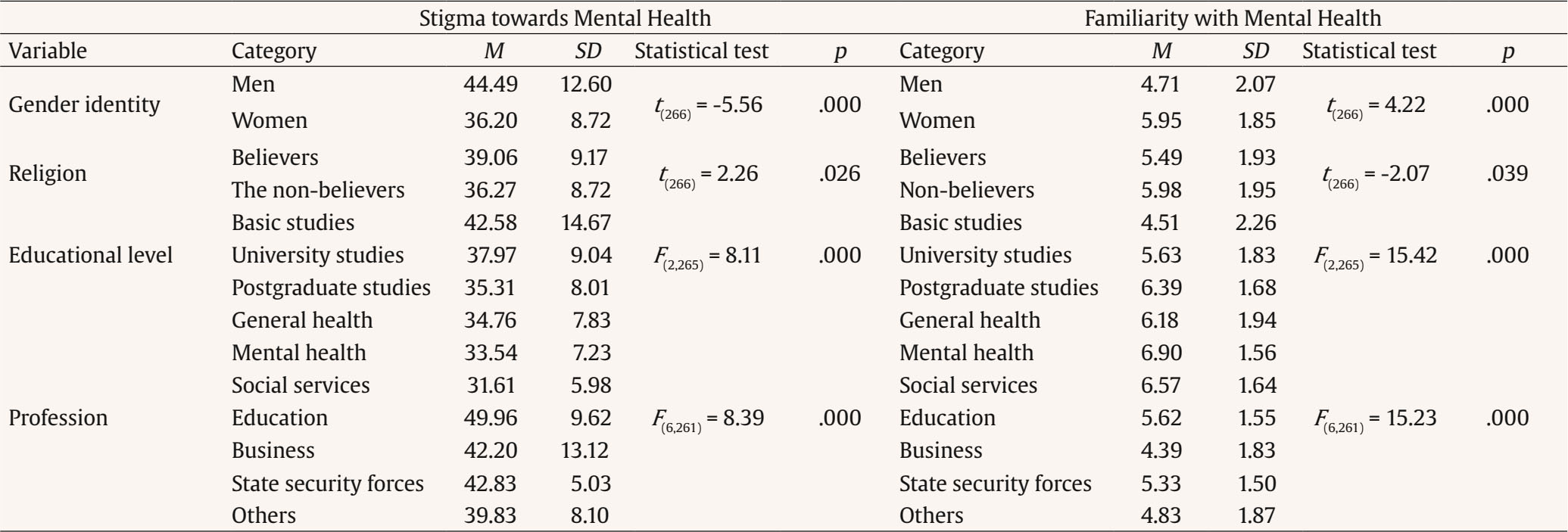 Note. M = mean; SD = standard deviation. Familiarity with Mental Health The general results show average values with respect to the familiarity of the sample (M = 5.72, SD = 1.95). Significant differences were found in relation to gender identity with greater familiarity with mental health in the female group, t(266) = 4.22, p < .001, ηp2 = .06. In relation to religion, non-believers have higher familiarity, t(266) = -2.07, p > .001, ηp2 = .01. There were also differences in educational level, F(2, 265) = 15.42, p < .001, ηp2 = .10, with post hoc analyses showing significant differences between the group with the lowest educational level and university and postgraduate students (p < .001), as well as between undergraduate and postgraduate students (p < .001). Significant differences were also found according to the profession of the participants, F(6, 261) = 15.23, p < .001, ηp2 = .26. Post hoc analyses apply significant differences between mental health professionals with respect to those in teaching (p < .001), those in business (p < .001) and those in other professions (p < .001), as well as those in general health versus business (p < .001). We also found significant differences between the group of social service professionals with the group from the company (p < .001) and from other professions (p < .001). These results can be observed in detail in Table 2. Myths towards Suicide Regarding the myths towards suicide, we found average scores (M = 21.59, SD = 5.81) that reveal the presence of myths towards suicide among the fathers and mothers of the sample. The results are shown in detail in Table 3. Table 3 Myths towards Suicide and Seeking Professional Help Attitudes in Relation to Sociodemographic Variables  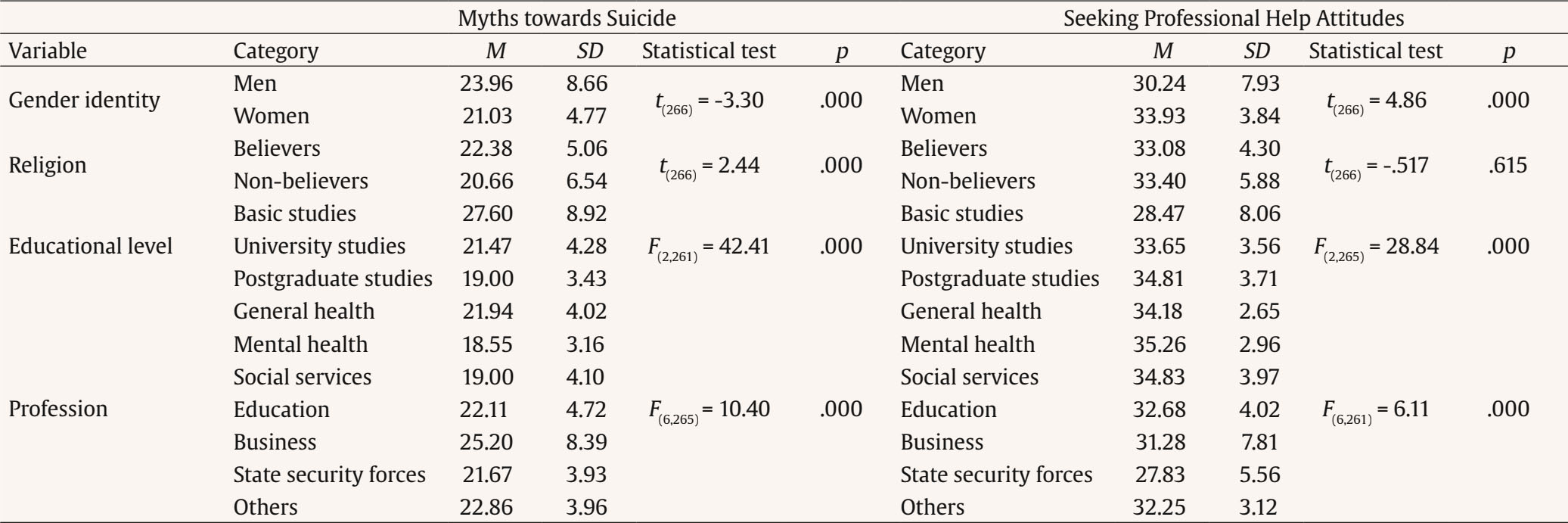 Note. M = mean; SD = standard deviation. Significant differences are observed in relation to gender identity, with men having a higher level of myths about suicide, t(266) = -3.30, p < .001, ηp2 = .06, as well as in relation to religion, where believers have a higher number of myths about suicide, t(266) = 2.44, p < .001, ηp2 = .01. There were also differences according to educational level, F(2, 261) = 42.41, p < .001, ηp2 = .24, with post hoc analyses revealing significant differences between the group with the lowest level of education with university studies (p < .001) and with postgraduate studies (p < .001). Significant differences were also found according to profession, F(6, 265) = 10.40, p < .001, ηp2 = .19. Post hoc analyses show significant differences when comparing mental health professionals with the rest of the professions (p < .001). We also found significant differences between the group of social service professionals and the group from the company (p < .001). The results are shown in detail in Table 3. Attitudes towards Seeking Professional Help Regarding help seeking, the general results show somewhat higher levels in the sample of fathers and mothers and there seems to be a greater commitment in terms of seeking PH attitudes (M = 33.22, SD = 5.08). Furthermore, we found significant differences in relation to gender identity, with women being more likely to seek professional help, t(266) = 4.86, p < .001, ηp2 = .08. The same occurs in relation to religion, where non-believers are more likely to seek help, t(266) = -.517, p > .001, ηp2 = .001. There were also differences according to educational level, F(2, 265) = 28.84, p <.001, ηp2 = .18), with post hoc analyses revealing significant differences between the group and the lowest educational level and the rest (p < .001), as well as according to profession, F(6, 261) = 6.11, p < .001, ηp2 = .12), where the post hoc analyses show significant differences between mental health professionals and those in the company (p < .001). The results are shown in detail in Table 3. Correlations A direct, significant and positive correlation was found between myths about suicide and stigma (r = .537, p < .001), and between seeking PH attitudes and familiarity with mental health (r = .384, p < .001). The correlation between familiarity and mental health and myths about suicide was negative and significant (r = -.415, p < .001), as was the correlation between seeking PH attitudes and myths about suicide (r = -.639, p < .001). Significant negative correlations were also found between stigma towards the child/youth population and help-seeking (r = -.489, p < .001), and between stigma and familiarity (r = -.337, p < .001). Regression Model A significant model was obtained that explained 44% of the variance, F(3, 264) = 71.70, p < .001, R2 = .449, R2 corrected = .443. Suicide myths were the variable that contributed the most to the prediction model, explaining 40.8% of the variance in seeking PH, followed by mental health stigma and finally mental health familiarity. In Table 4 the model developed can be observed in detail. Table 4 Correlations between Stigma, Familiarity, Attitudes towards Professional Help-seeking and Myths about Suicide  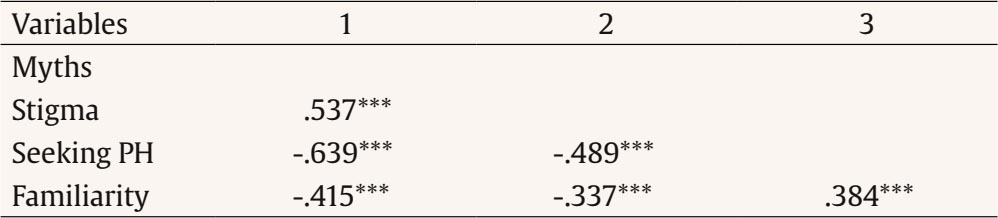 Note. PH = professional help. ***p < .001. The present research addresses the stigma associated with MHP in childhood and adolescence in a sample of fathers and mothers, analyzing the main stigmatizing attitudes, myths associated with suicide and familiarity with mental health, as well as the main predictors of help-seeking in these types of problems. The results show mean levels of stigma towards MHP in childhood and adolescence slightly higher than those obtained in previous research with the same assessment instrument focused on mental health in adults (Corrigan et al., 2014), and consistent with other studies on stigma in childhood and adolescence (Pescosolido et al., 2007; Song et al., 2018). More specifically, we found that the dimensions of stigma with the highest scores were help, coercion and grief, showing attributes of overprotection, which may hinder independence and autonomy processes, necessary for adequate development at this stage. Parental stigma towards children with MHP seems to be a major problem to be faced, which even exceeds the data found in the adult population, which is already alarming. Regarding myths about suicide, the results also show mean scores (Mmyths = 21.59) that reveal the presence of myths about suicide in childhood and adolescence in the sample studied. These results are consistent with other studies on suicide myths in the adult population (Nicholas et al., 2020), but cannot be compared with myths about suicide in the children and adolescent population, due to the lack of previous research. Therefore, further research in this line is essential to allow comparisons and more in-depth analysis of this phenomenon, the frequency of which has increased in recent years (Mayne et al., 2021).On the other hand, in relation to familiarity with mental health, we observed that the scores were also average, although these values revealed less familiarity than in the original study on the scale (Corrigan et al., 2001). Concerning help-seeking scores, the results were lower than those found in previous studies conducted in adults (Elhai et al., 2008). Thus, the parents evaluated showed a lower valuation of the usefulness, importance and use of psychological services in childhood and adolescence. In relation to the differences in the sociodemographic variables studied, it is observed that in general stigmatizing attitudes and myths about MHP are significantly higher in fathers than in mothers (p < .001), with religious beliefs, with a lower level of education (p < .001), and who did not have professions related to mental health or social services (p < .001). Similarly, these individuals also showed significantly lower scores for familiarity with MHP in childhood and adolescence (p < .001) and help-seeking in the face of MHP (p < .001). The data obtained on stigma and myths about suicide are consistent with previous studies that analyzed some of these sociodemographic variables in adult population (Na et al., 2018; Nicholas et al., 2020; Pereira & Cardoso, 2019), as well as in studies focused on the stigma associated with MHP in childhood and adolescence, where the results coincide on a greater stigma in men (Pescosolido et al., 2007; Song et al., 2018). These data reveal the importance that certain social and cultural variables may have in relation to mental health. Perhaps the traditional caregiving role of Western culture with greater empathy, which is usually more represented by mothers, is related to less stigma and myths, and to greater familiarity with MHP and search for help for their children. However, there is still a need for parenting models in which fathers can develop, in the same proportion as mothers, less stigmatizing and more care-seeking attitudes towards MHP for their children. Secondly, it seems that the educational level is also key, since lower educational levels have more stigma and myths, and at the same time they are less familiar with mental health and seek less help. Access to information has been shown to be a protective factor against stigma and gives people a better problem-solving repertoire (Corrigan et al., 2005). On the other hand, the type of profession also marks differences, supporting the hypotheses on contact as a strategy to reduce stigma (Schenner et al., 2011), as people with professions related to mental health show better attitudes and a greater predisposition to seek help. Another interesting factor is religiosity. It seems that those with religious beliefs present more myths toward suicide and more stigmatizing beliefs toward MHP in childhood than those who do not consider themselves religious. This is also found in studies conducted in adult population (Moksony & Hegedus, 2021). It is known that certain MHP have been considered as divine punishments (Stucchi-Portocarrero, 2013). Suicide was also silenced among believing populations. Moral objections to suicide, especially the conviction of going to hell after committing suicide, have a restraining effect on suicide and suicidal tendencies (Van den Brink et al., 2018). Table 5 Results of the Multiple Regression Analysis on the Variable Attitudes towards Seeking Professional Help  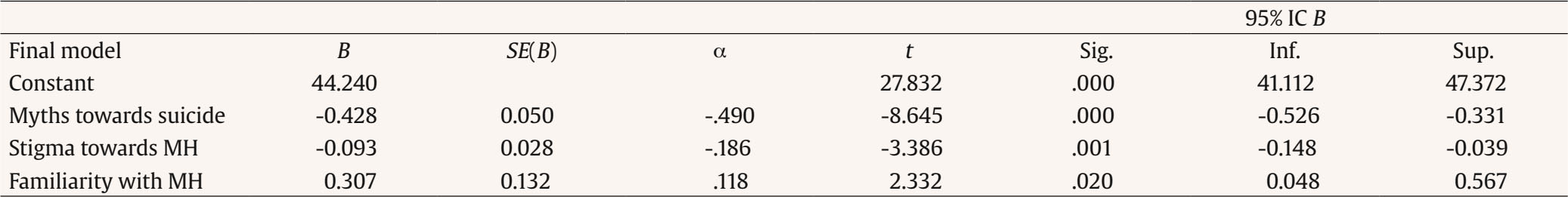 Note. B = unstandardized coefficient; SE(B) = standard error of B; a = standardized coefficient; t = contrast statistic; Sig. = statistical significance; 95% CI B = 95% interval for B; Inf. = lower, Sup. = upper; MH = mental health. The regression model developed confirms our main hypothesis, revealing stigmatizing parental attitudes as a barrier to seeking specialized professional help when necessary. The model shows how negative attributions along with the presence of myths about suicide and low familiarity with MHP are key variables that may prevent parents from seeking PH, explaining 44% of the variance of this variable. The suicide myths alone predicted the highest percentage of the total variance of the negative help-seeking attitudes, followed by stigma and finally by the familiarity. Previous studies have already warned of the detrimental impact of parental stigma on children (Ferrie et al., 2020; Kranke et al., 2010; Moses et al., 2009). Considering the results obtained in the present study, the impact could be doubly negative: parents with stigmatizing attitudes towards mental health will not only transmit them to their children, but these children will also be less likely to be attended by a professional, and therefore receive early diagnosis and the necessary care. Addressing the variables proposed seems key in providing adequate child and adolescent mental health care and secondary prevention. Demystifying irrational ideas about suicide, combating stigma and normalization, and promoting contact with mental health should be included in mental health campaigns targeting parents of children and adolescents. This model may be particularly relevant due to the lack of previous studies in this population analyzing the relationship between stigma and help-seeking in parents. Stigma towards MHP is not limited to the adult population, but also extends to the children and adolescence, having important practical implications that may determine the detection, approach, and avoidance of the chronification of psychological problems in young people (Pescosolido et al., 2007). The present study has constraints that should be mentioned. First, the type of sampling used, as well as the high presence of women in the sample compared to men. The fact that the majority of the sample is made up of women may have certain implications. Some studies have noted that MHP stigma tends to be lower in women (Bradbury et al., 2020), as well as in general women have a greater tendency to seek help (Holzinger et al., 2012), so a higher proportion of men in the study could change the results by leading to more stigma and less help-seeking. In addition, it is interesting to mention that mothers still seem to be the ones who primarily continue to take on care giving (Moreira da Silva & de Carvalho, 2021).This may also explain why women are the most involved in this type of surveys aimed at families in general. On the other hand, it is necessary to also point out that the sample is highly educated. Several studies have pointed out that people with a higher educational level show lower levels of stigma (González-Sanguino et al., 2023; Zamorano et al., 2023), so that in the same way as in relation to gender it would be interesting to analyze a sample with greater diversity in terms of education. Secondly, we consider it necessary to point out that since this is an evaluation of a sensitive subject, it is possible that there may be certain biases in the responses, given the possible desirability. Thirdly, it is necessary to refer to the questionnaire to assess myths about suicide created ad hoc for the study. Although the ideal is to use previously validated instruments, the use of a tool created ad hoc for the present research is due to the lack of previous instruments to evaluate the construct, revealing the lack of research in the field (Eshun, 2006; Lee et al., 2007; Ouzouni & Nakakis, 2009; Renberg & Jacobsson, 2003). Therefore, this study opens the door for future studies to try to create specific instruments to evaluate this variable. On the other hand, we believe it is necessary to comment that the sample is focused on a Spanish population, so the results have a clear cultural limitation. The search for professional help by parents is of vital importance to ensure an adequate approach to the mental health of children and adolescents in a context in which these problems have increased significantly in recent years. Given that this help-seeking has been hampered by myths about suicide, stigma, and familiarity with MHP, anti-stigma awareness campaigns targeting the parental population are necessary. In addition, certain groups with higher levels of stigma and myths are suggested, such as men, religious people, people with low educational level, and those with professions far from mental health. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Moreno-F. Ramiro, B., González Domínguez, S., González-Sanguino, C. (2024). Stigma towards child and adolescent mental health problems among fathers and mothers. A cross-sectional study. Clínica y Salud, 35(1), 27-33. https://doi.org/10.5093/clysa2024a8 References |
Cite this article as: Ramiro, B. M., Domínguez, S. G., & González-Sanguino, C. (2024). Stigma towards Child and Adolescent Mental Health Problems among Fathers and Mothers. A Cross-sectional Study. ClĂnica y Salud, 35(1), 27 - 33. https://doi.org/10.5093/clysa2024a8
Correspondence: Clara.gonzalez.sanguino@uva.es (C. González-Sanguino).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







