
Mom Supporting Mom: Effective Peer Support Intervention for Women with Postpartum Psychological Distress
Antonin Sebela1, 2, Anna Horakova1, 3, Hana Nemcova1,4, Marie Kuklova1, Eliska Noskova1, 2, Patrik Svancer1, 2, Nancy Byatt5, Adela Janovska1, and Kristyna Hrdlickova1,4
1National Institute of Mental Health, Klecany, Czech Republic; 2Charles University, Third Faculty of Medicine, Prague, Czech Republic; 3Charles University, First Faculty of Medicine, Prague, Czech Republic; 4Charles University, Faculty of Arts, Department of Psychology, Prague, Czech Republic; 5UMass Chan Medical School and UMass Memorial Health, Department of Psychiatry, Worcester, Massachsuetts, USA
https://doi.org/10.5093/pi2025a12
Received 22 November 2024, Accepted 13 May 2025
Abstract
Objective: Untreated perinatal mental health disorders can have serious consequences for the whole family system. The purpose of this study was to examine the effectiveness of peer support intervention in improving postpartum psychological distress. Method: We evaluated a remote peer support intervention, Mom Supports Mom, in a randomized controlled trial. The primary study outcome was the level of depressive symptoms at week six after delivery. Secondary outcomes included levels of anxiety symptoms, quality of life and the presence of psychiatric disorders at week six after delivery. Trial protocol was registered at ClinicalTrials.gov (NCT04639752). Results: The study sample consisted of 315 participants in the control group, and 173 participants in the intervention group. The Mom Supports Mom intervention was associated with decreased depressive (Cohen’s d = 0.30, p = .003) and anxiety symptomatology (d = 0.29, p =.003) at week six after birth compared to the control group. Mom Supports Mom intervention was also associated with an increase in health-related quality of life at week six after birth (d = 0.27, p =.008). No statistically significant difference was found between the groups in the presence of psychiatric diagnoses at six weeks postpartum. Conclusions: Peer intervention Mom Supports Mom is effective in reducing depressive and anxiety symptomatology in postpartum women and improving their health-related quality of life. Mom Supports Mom can serve as a low-intensity approach that is effective for mild illness and has the potential to be scalable.
Keywords
Peer support intervention, Psychosocial intervention, Postpartum, Mental health
Cite this article as: Sebela, A., Horakova, A., Nemcova, H., Kuklova, M., Noskova, E., Svancer, P., Byatt, N., Janovska, A., & Hrdlickova, K. (2025). Mom Supporting Mom: Effective Peer Support Intervention for Women with Postpartum Psychological Distress. Psychosocial Intervention, 34(3), 151 - 160. https://doi.org/10.5093/pi2025a12
Correspondence: antonin.sebela@nudz.cz (A. Sebela).
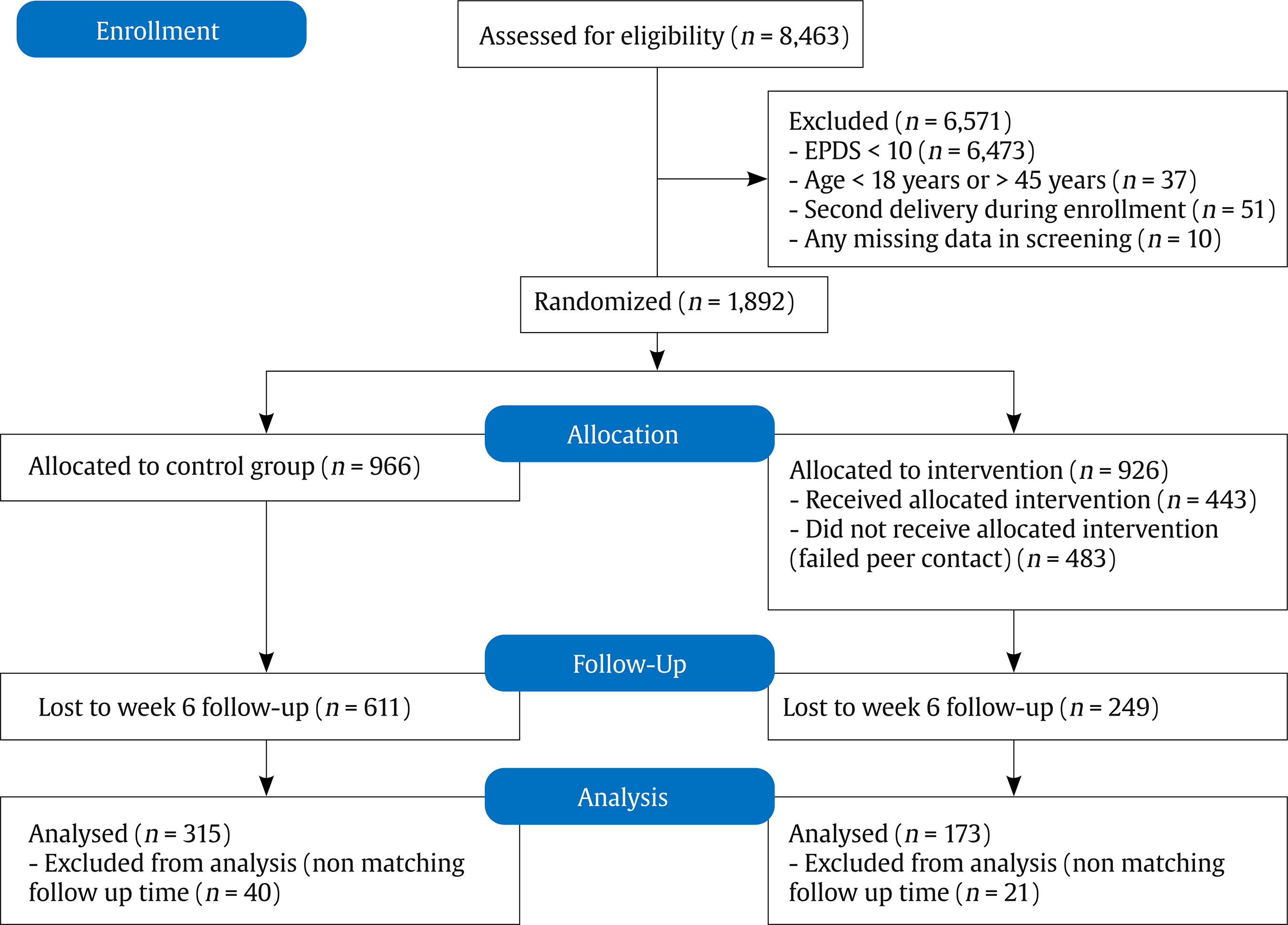
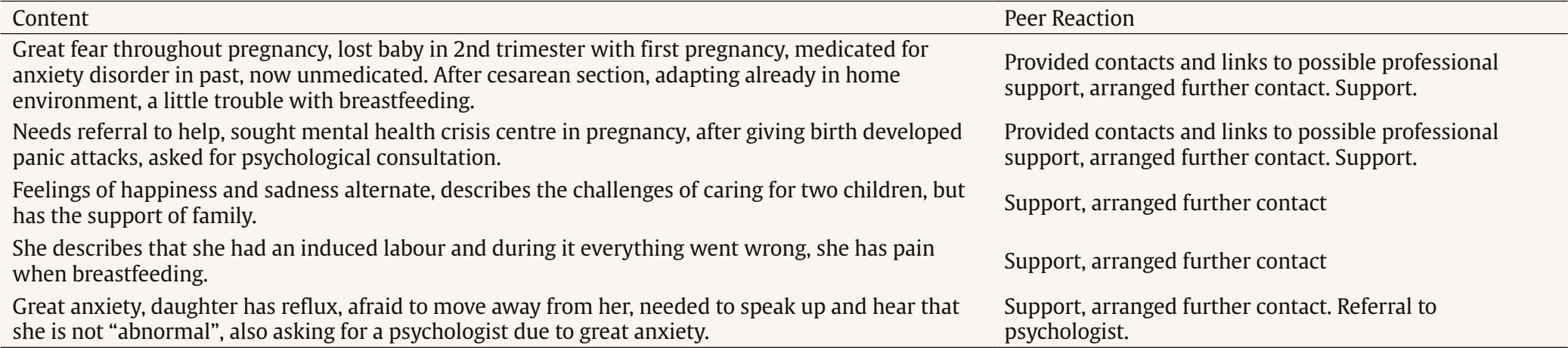
The postnatal period poses a risk of both onset and relapse of mental disorders. Anxiety and depression are the most common, with a reported prevalence of 9% to 20% (Howard & Khalifeh, 2020; Woody et al., 2017). We have recently described that the prevalence of the postpartum mental health disorders in the Czech Republic is 13%, which is consistent with international data (Horáková et al., 2022). Untreated perinatal mental health disorders can have serious consequences for child’s development, the quality of the child-mother relationship and the whole family system (Dubber et al., 2015; Kersten-Alvarez et al., 2012; O’Higgins et al., 2013). Infants of mothers with postnatal depression are less likely to be breastfed (Dias & Figueiredo, 2015), are at a greater risk of malnutrition (Dadi et al., 2020), have poorer cognitive development (Grace et al., 2003; Smith-Nielsen et al., 2016), and show greater social withdrawal (Smith-Nielsen et al., 2019). Perinatal mental health disorders incure a long-term cost to society of approximately £8.1 billion for each one-year birth cohort in the UK, and $14 billion per birth cohort in the US (Bauer et al., 2016; Luca et al., 2020). Perinatal mental disorders affect not only the mother but also her family and society; therefore, addressing perinatal mental health is an important part of both healthcare and societal well-being (Howard & Khalifeh, 2020). Given the negative impact and cost, it is important to identify perinatal mental health disorders early and to treat them effectively, even in the subclinical forms (O’Connor et al., 2019). National health guidelines recommend that gynecological and obstetric care providers assess their patients’ emotional state, including using screening methods (National Institute for Health and Clinical Excellence, 2020; The American College of Obstetricians and Gynecologists, 2023). In the National Action Plan for Mental Health 2020-2030, the Czech Republic has outlined measures to establish a validated system of screening methods for identifying psychosocial risks in pregnant and postpartum women. When implementing perinatal mental healthcare, it is essential to address the barriers that women face in accessing care and support. Barriers include the cost of care, the lack of availability of mental health professionals, and the fear of being judged by others (Prevatt et al., 2018). In the Czech Republic, up to 75% of women experiencing perinatal mental health disorders do not actively seek professional help (Sebela et al., 2021). Many face significant stigma surrounding perinatal mental disorders and often struggle to identify where to seek help (Banasova et al., 2023). Peer support for individuals at risk of perinatal mental health disorders could play a key role in overcoming these barriers (Dennis et al., 2003). In this context, peers refers to women who have personally experienced and recovered from perinatal mental health disorders. Peer interventions focus on offering encouragement, sharing personal experiences, and providing valuable knowledge. Peer support has been found to be effective in alleviating postpartum mental health symptoms (Dennis 2014; Huang et al., 2020; Kamalifard et al., 2013; Manolova et al., 2023; McKimmy et al., 2023; Prevatt et al., 2018). The principle of peer support is that the peer consultant, after receiving training, can provide support without needing to be an expert in the field (Shalaby & Agyapong, 2020). When talking to the help seeker, peer supporters can assist them in naming their difficulties, identifying risk factors, and choosing appropriate professional help (Watson, 2019). In this paper, we report the results of a study investigating the effectiveness of remote peer support (via telephone, messenger applications, and email) provided by trained peer consultants for women experiencing postpartum mental health difficulties in the Czech Republic. Study Design and Aims A randomized controlled trial (ClinicalTrials.gov Identifier: NCT04639752) was conducted in which women were randomized 1:1 to control and intervention groups. The aim of this study was to assess, in a real-world setting, the effectiveness and acceptability of remote peer support intervention for women experiencing mental distress early after delivery. In addition, the study aimed to uncover the adaptations needed for widescale implementation across the Czech Republic. Setting In the Czech Republic, there were 89,084 live births in 2023 (Národní zdravotnický informační portál [NZIP, 2023]). The vast majority of births take place in maternity hospitals. Planned home births are not formally integrated into the public healthcare system. Official statistics on the number of home births are not systematically collected. However, research and expert estimates suggest that home births remain rare in the Czech Republic (Krepelka et al., 2023; Vintrová & Pařízek, 2018). Obstetric care, including prenatal check-ups and delivery, is covered by public health insurance. The Czech Society of Neonatology recommends discharging mothers and newborns from the hospital 72 hours after delivery in cases of uncomplicated births (Mydlilova, 2013). In contrast to countries like the United States or the United Kingdom, the Czech Republic lacks a structured, nationwide system of perinatal mental health care (Horakova et al., 2024). In practice, support is typically provided by individual professionals from general psychiatry or psychology. Women who require psychotropic medication must consult a psychiatrist in person, as prescriptions cannot be issued without a face-to-face appointment. The first routine gynecological check-up following childbirth usually takes place around six weeks postpartum. There is currently no standardized mental health screening protocol for the perinatal period, although the Edinburgh Postnatal Depression Scale (EPDS) is utilized in some maternity hospitals and gynecology clinics. Participants and Recruitment Participants were recruited from May 2021 to April 2023 in five maternity hospitals across three regions of the Czech Republic. Participants were informed about the study by a nurse or midwife in the maternity unit. The recruitment criteria included women aged 18-45 years who spoke Czech, had an email address, had given birth in a hospital, and scored ≥ 10 on the Edinburgh Postnatal Depression Scale (EPDS). These women were then invited to participate in the study. The cutoff score 10 on the EPDS was used to identify women who show symptoms of depression. Based on an analysis of the available evidence, the authors describe that women who score more than 10 on the EPDS may already be signaling the presence of distress and depressive symptoms, and omitting them from population-based interventions could lead to the under-detection of women and their families who deserve intervention so that their psychological state does not deteriorate further (Khanlari et al., 2019). Women with an EPDS score < 10 were sent an automated email thanking them for their interest in the study and informing them that they were at a low risk for postpartum distress; these women were not included in the trial. After obtaining informed consent, a nurse or midwife provided the woman with a tablet containing online questionnaires on the second day after delivery. To maintain the usual clinical workflow, the recruitment and study procedures were integrated into the classical clinical workflow of the maternity wards. Teams in the participating maternity hospitals received a small financial remuneration from the study budget of 60,000 Czech crowns per year (2,640 USD per year per team). Women with a score of ³ 10 on the Edinburgh Postnatal Depression Scale (EPDS) were invited to participate in the study. The system did not provide the maternity hospital staff with information regarding the participants’ scores. Procedure After completing informed consent and baseline questionnaires, women with an EPDS ≥ 10 were randomized 1:1 to control and intervention groups. All women received an information email with the results of their EPDS screening. Women in the intervention group were informed that they were at higher risk of psychological distress based on the screening results and that a peer consultant would contact them within the next 2-3 days (see the Intervention section for more details). The control group was also informed of their higher risk based on the screening results but was provided with mental health care information and resources instead. Each participant received an email invitation to complete a follow-up questionnaire six weeks after their enrollment. If a participant did not complete the follow-up questionnaire, an automated reminder was sent three times over the next three days. Participants were not financially or otherwise motivated to complete a follow-up questionnaire. Participants who completed the questionnaire later than seven weeks after delivery were excluded from the analysis due to a non-matching follow-up time. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of National Institute of Mental Health (2020). Informed consent to participate was obtained from all individual participants included in the study. Intervention In this study, we implemented the Mom Supports Mom intervention to provide peer support for women experiencing postpartum mental health challenges. A peer consultant contacted participants assigned to the intervention group within three days of completing the questionnaires. The peer consultant contacted the participant by phone, text message, and email up to three times or until the participant responded to the offer of support. Each reciprocal interaction, i.e., a contact from the consultant and a response from the participant, was counted as one contact with the peer consultant. If there was no reciprocal contact, we labeled the intervention as an unrealized peer contact, and these participitants were removed from the analyses. The conversation between the participant and the peer consultant ended when the woman stated that she had no problems to discuss, felt fine, or was not interested in further conversations. In this case, the peer consultant reassured the woman that she could seek support at any time in the future and sent her a text message or email with contact information for seeking help if needed. If the woman at risk stated that she was not feeling well and agreed to continue the conversation, the peer consultant proceeded to help her identify the difficulties she was experiencing. The peer consultant helped participants to cope with mild symptoms related to common maternity problems directly (through listening, emotional release, relaxation techniques, etc.). For moderate to severe symptoms that interfered with the woman’s normal functioning (e.g., suicidal thoughts, sleep disturbances, deteriorating mental state), the peer consultant would refer the woman to professional medical or psychological help. The main indicator of whether the peer counsellors should consider the symptoms as mild or more severe was whether the difficulties described by the woman affected her daily functioning. If the woman was interested, contact with the peer consultant could be repeated; the frequency and form of further consultations would depend on mutual agreement. We designed the Mom Supports Mom intervention, which follows the mental health screening in maternity hospital, in line with the WHO recommendations described in the Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services (World Health Organization, 2022). Further information on the methodology of the Mom Supports Mom intervention is described in the Appendix. The peer team consisted of ten consultants and was further divided into two regional teams. The regional team consisted of one senior peer consulant (coordinator and team intervisor) and four peer consultants. Before the onset of the trial, all peers participated in an initial eight-hour in person-training session. The training covered the following areas: the psyche of women in the perinatal period and an overview of psychological difficulties, methods and principles of peer support, basics of crisis communication and psychological first aid, basics of psychotherapy, and basics of mental hygiene for peer consultants (Curry et al. 2019; Mulvale et al. 2019; Prevatt et al. 2018). At the end of the training, the peer consultant took a test to verify the knowledge acquired. Training was conducted by psychiatrists, psychologists, and senior peer consultants from the Centre of Perinatal Mental Health at National Institute of Mental Health, Klecany, Czechia, as well as representatives from the patient non-govermental organization Mom’s Smile. Further, each peer consultant was supervised and intervised once a month, either by sharing among other peer consultants in the regional team (intervision) or under the guidance of a psychologist, psychotherapist, or psychiatrist (supervision). In addition to the regular monthly interviews and supervision, peers could request additional sessions as needed. Intervisions and supervisions took place via video communication channels. The cost per regional peer team was 108,000 Czech crowns ($4, 680) per year and was covered by the study budget. Outcomes Primary outcome was the change in depressive symptoms between delivery and the sixth week after delivery, comparing the experimental and control groups. Secondary outcomes included changes in anxiety symptoms, health-related quality of life, and the presence of psychiatric diagnoses at the sixth week after birth. Outcome Measures Participants completed all baseline questionnaires after delivery in the maternity ward and the follow-up questionnaires online at six weeks postpartum. Depressive Symptoms. We used the EPDS as a measure of depressive symptomatology; the primary outcome of our trial (Cox et al., 1987). The EPDS is a self-report questionnaire and is the gold standard for identifying women at risk of developing depression in the perinatal period. It is a validated instrument for measuring symptoms of perinatal depression and has recently undergone psychometric validation in the Czech setting (Horáková et al., 2022). The EPDS is a 10-item self-report instrument, with items scored on a 4-point scale, producing a summative score ranging from 0 to 30. Higher scores indicate lower mood. In the present study, the internal consistency (Cronbach’s alpha = .89) was good. Anxiety Symptoms. This outcome was measured using the Perinatal Anxiety Screening Scale (PASS). The PASS is a self-report questionnaire used to measure anxiety symptoms in the perinatal period, with well-validated psychometric properties; Cronbach’s a = .96 (Somerville et al., 2014). The PASS is a 31-item self-report instrument developed to assess different aspects of perinatal anxiety symptoms. Items are rated on Likert-type scale producing a summative score ranging from 0 to 93 with higher scores indicating greater levels of anxiety symptoms. In the present study, the internal consistency (Cronbach’s alpha = .94) was excellent. Health-Related Quality of Life. Health-related quality of life was assessed using the Assessment of Quality of Life - Eight Dimension scale (AQoL-8D) (Richardson et al., 2014). This scale covers eight dimensions of quality of life that form two super-dimensions: Physical (independent living, senses, and pain) and Psychosocial (mental health, relationships, coping, self-worth, and happiness). The AQoL-8D provides a utility score ranging from 1.00 (full health) to .00 (death-equivalent health states) (Hawthorne & Osborne, 2005). The AQoL-8D has previously been used in the Czech mental health research within an international context (Nordstroem et al., 2017). In the present study, the internal consistency (Cronbach’s alpha = .95) was excellent. Presence of Psychiatric Diagnoses. At six weeks postpartum, women were contacted by telephone and administered the Mini-International Neuropsychiatric Interview 5 (MINI5) (Sheehan et al., 1998). The MINI5 is a brief structured diagnostic interview developed to provide a rapid but accurate psychiatric assessment according to the International Classification of Diseases 10 for research purposes as well as part of clinical practice. It takes approximately 15 minutes to administer and it is a widely used and psychometrically validated instrument. The MINI5 was administered by two trained clinical psychiatrists. Sample Size Based on previously published studies indicating that the effect of peer support in reducing self-assessed depressive symptoms is moderate (Shorey et al., 2018), we calculated the sample size needed to detect a medium-sized intergroup difference on the Edinburgh Postnatal Depression Scale (effect size = 0.60) with a power of 80% and a significance level of 5% (two-tailed). Thus, with the power analysis set in this way and a potential drop out rate of 30%, the minimum file size required for the intervention part of the study was 120 women (60 for each group). Statistical Analysis Using descriptive statistics (means, SDs, or proportions), we calculated the difference between baseline and follow up data as follows for all study outcomes: ΔEPDS = EPDS score at week six – EPDS score at baseline. The distribution of each variable was tested by kurtosis and skewness analysis, using interval -1 to +1 as indicator of approximate normal distribution (Mishra et al., 2019). For categorical data, we used Pearson’s chi-square test to examine differences between the two study groups. Independent two-sample t-tests were conducted for data at the interval level of measurement. We conducted one way ANCOVAs to determine a statistically significant difference between the intervention and the control group on the Δ scores controlling for the baseline scores and age. The statistical significance for all tests was set at p < .05. The standardized effect size for each significant intergroup difference was calculated as Cohen’s d. The reliability of the scales used in our study was estimated using Cronbach’s alpha (Tavakol & Dennick, 2011). The analyses were performed using the SPSS software package, version 23. Of the 8,463 participants initially assessed for eligibility, 6,571 were excluded for having an EPDS total score >10, and 37 were excluded because they did not meet the age inclusion criteria. Further, 51 participants were excluded as they were assessed for eligibility for the second time during the enrollment period and 10 participants were excluded due to missing data in the initial screening. Participant flow is shown in Figure 1. A total of 1,892 participants met eligibility criteria, with 966 participants randomized to the intervention group and 926 participants to the control group. A total of 443 participants from the intervention group were excluded as they did not receive allocated intervention (unrealized peer contact). Further, 611 participants from the control group and 249 participants from the intervention group were lost to follow-up. The final study sample consisted of 315 participants in the control group, and 173 participants in the intervention group. Table 1 presents characteristics of trial participants. There were no statistically significant differences between the two groups as regards baseline levels of depressive and anxious symptomatology, health related quality of life, and marital status. The two groups differ statistically in age (intervention group: mean 32.5, SD = 4.7; control group: mean 31.5, SD = 4.8; t(486) = -2.266, p = .02. The median number of reciprocal peer contacts in the intervention group was 1 with range one to 6 contacts. Table 2 presents examples of peer contacts. Table 1 Characteristics of Study Participants  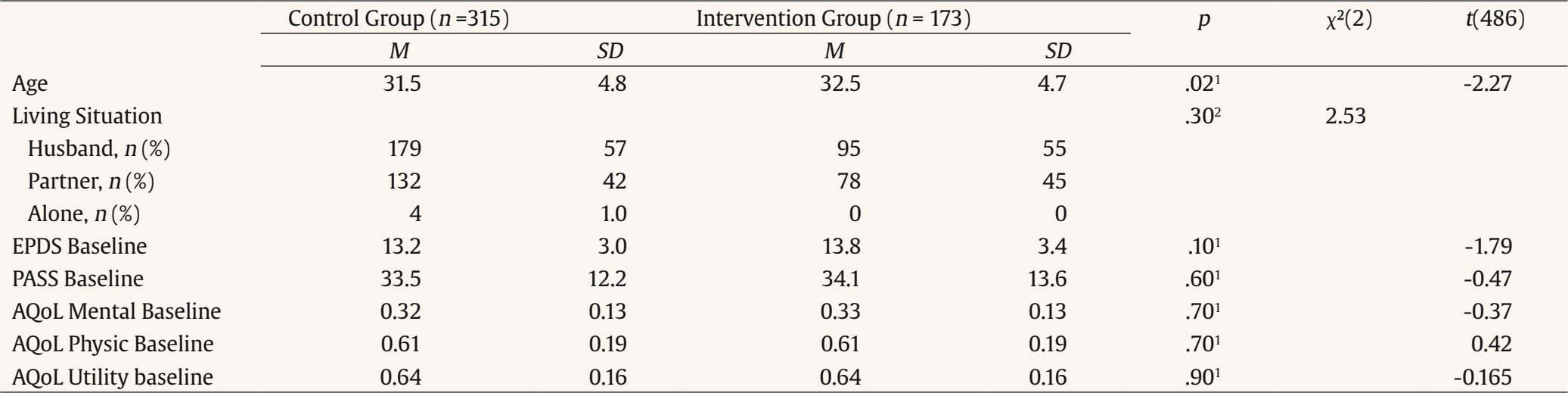 Note. AQoL = assessment of quality of life; EPDS = Edinburgh Postnatal Depression Scale; n = number; PASS = Perinatal Anxiety Screening Scale; SD = standard deviation 1Independent two-sample t-test; 2Pearson’s chi square test. Study Outcomes The Mom Supports Mom intervention was associated with a decrease in depressive symptomatology at six weeks postpartum, compared to the control group (Cohen’s d = 0.30; 95% CI = 0.10-0.48, p = .003). The effect remained significant after controlling for participants’ baseline depressive symptomatology and age, F(1, 484) = 4.979, p = .026. Further, it was associated with decreased anxiety symptomatology at six weeks postpartum, compared to the control group (Cohen’s d = 0.29; 95% CI = 0.10-0.47, p = .003). The effect also remained significant after controlling for covariates, F(1, 484) = 6.177, p =.013. Finally, the Mom Supports Mom intervention was associated with increased health related quality of life at six weeks postpartum as compared to the control group (Cohen’s d = 0.27; 95% CI = 0.08-0.45, p = .008), and the effect also remained significant after controlling for covariates, F(1, 484) = 7.072, p = .008. However, we found no statistical difference between the groups in the presence of psychiatric diagnoses at the sixth week postpartum. For detailed results, see Table 3 and 4. Table 3 Outcome Measures of Self-Assessment Scales  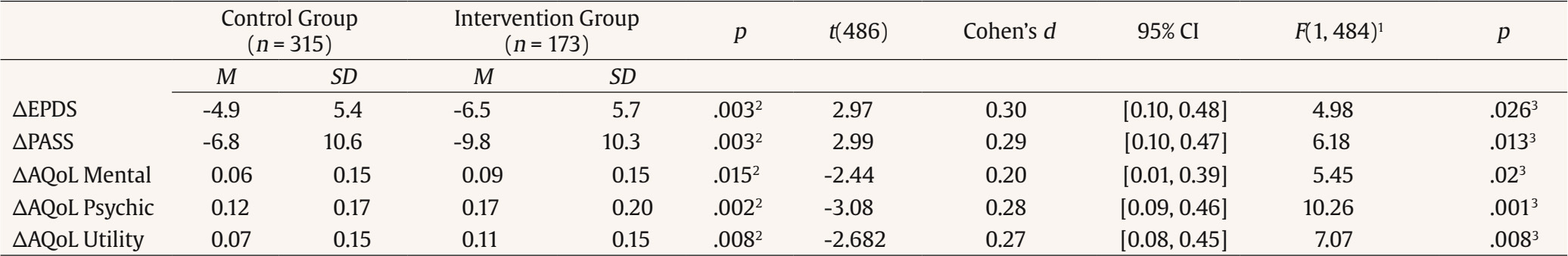 Note. ΔAQoL = assessment of quality of life score at week six – assessment of quality of life score at baseline; ΔEPDS = EPDS score at week six – EPDS score at baseline; ΔPASS = Perinatal Anxiety Screening Scale at week six - Perinatal Anxiety Screening Scale score at baseline. 1Adjusted Age, Baseline Score, 2Independent two-sample t-test; 3One way ANCOVA. Table 4 Presence of Psychiatric Diagnoses at Week 6 (MINI)  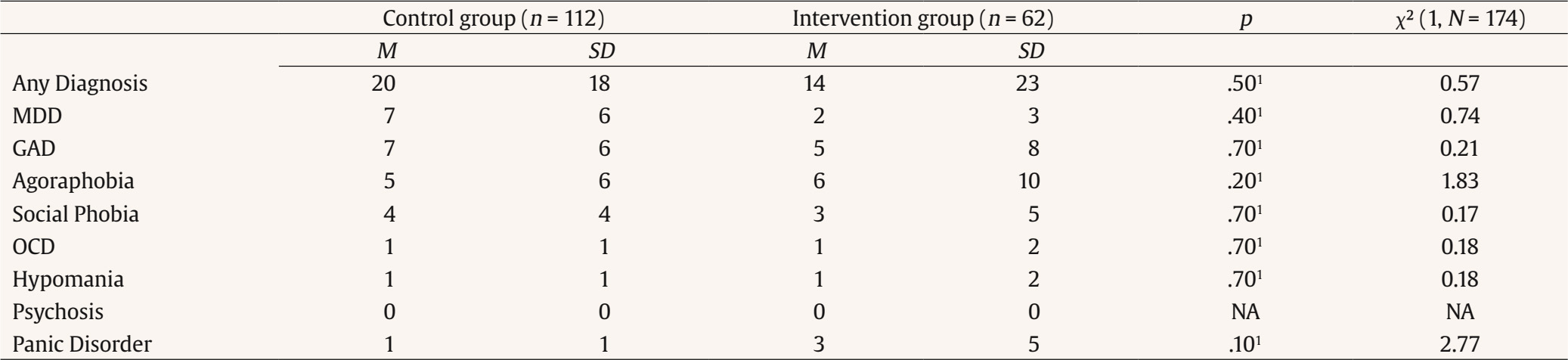 Note. GAD = generalized anxiety disorder; MDD = major depressive disorder; OCD = obsessive compulsive disorder. 1Pearson's chi square test. Mom Supports Mom is a remote peer support intervention designed for women experiencing psychological distress after delivery. We found that it was associated with significant improvements in depressive symptomatology, anxiety symptomatology, and health-related quality of life at six weeks postpartum compared to those who did not receive the intervention. Our trial suggests that early detection and intervention for psychological distress in postpartum women is viable and improves symptoms within the Czech setting. However, it is important to mention that even in the group without the intervention, we found a decrease in the rate of reported symptoms. We cannot attribute the entire effect on the improvement of the mental state of women in the intervention group to the Mom supports Mom intervention, but we must also take into account the natural improvement as a normal consequence of adjustment to parenthood (Akman et al., 2008; Jia et al., 2016). The results of our trial are consistent with those of a meta-analysis of studies assessing the effectiveness of peer support interventions for perinatal depression (Huang et al., 2020). In our study we did not show that the Mom Supports Mom intervention was able to reduce the risk of developing a mental disorder at six weeks postpartum. This finding may be explained by the fact that our study involved low-frequency peer support, where the median number of peer contacts with the participant was only one session, while in other studies participants had higher frequency of peer support contacts. This may be due to the fact that in the Czech Republic the position of peer consultant in mental health is not as traditional as in other countries (Balková, 2022). Thus, participants may not have had sufficient trust in peer consultants to establish regular contact. To explore this further, follow-up qualitative research is needed. The strength of our work is that, to avoid overestimating the prevalence of postpartum mental health disorders, we assessed the presence of mental disorders at six weeks postpartum using a structured psychiatric interview, in contrast to studies that relied on cutoff scores from self-rating scales (Levis et al., 2020; Thombs et al., 2020). Furthermore, other studies examing the effect of peer support on reducing the risk of developing a mental disorder in perinatal women have found no effect. However, these studies cannot be directly compared to our, because they differ both in the peer intervention itself and in the person of the peer or the target group of intervention users. Sikander et al. (2019) tested the Thinking Healthy Programme for perinatal depression delivered by laywomen (without self-experience with perinatal mental health distress) in Pakistan (without self-experience with perinatal mental health distress) and did not find any effects on reducing depressive symptoms or the risk of developing depression. Similarly, Gjerdingen et al. (2013) found no benefits of postpartum peer support for women experiencing postpartum mental distress when the peer supporters had no self-experience with perinatal mental distress. Recently, there has been increasing emphasis on the large global gap between service needed and provided for mental disorders (Evans-Lacko et al., 2018; Keynejad et al., 2021). In perinatal mental health, the excess of demand for care over its supply is even more alarming given the impact of untreated perinatal mental disorders (Baron et al., 2016; Howard & Khalifeh, 2020). Possible solutions to the problem of inadequate care supply include involving non-health professionals and integrating professionals from fields outside of psychiatry or psychology into perinatal mental health treatment pathways (Lomonaco-Haycraft et al., 2018; Manolova et al., 2023; Moore Simas et al., 2018; Prom et al., 2022). The WHO currently recommends stepped care approaches that integrate somatic and mental health care for women within primary somatic health care settings in its implementation guideline (World Health Organization, 2022). Our study provides evidence that integrating mental health care with maternity care for postpartum women can be effective, even in a country where such integrated care is not yet a common practice. Limitations of the Study Our findings must be interpreted in the context of several limitations. First of all, we must mention the relatively high dropout rate among the study participants. This fact may affect the possible generalization of our result (Bell et al., 2013). The high dropout rate in our study can be explained by several reasons. Firstly, all contact between the research team and participants was remote, via email communication or telephone call, and study participants were not financially or otherwise motivated to complete the follow-up questionnaires or undergo research telephone calls. Finally, recruitment to the study began in 2020, at the beginning of the COVID pandemic, which may have also influenced participants’ willingness to participate in the study (Bagiella et al., 2020). Another limitation is the high number of unrealized peer contacts in the intervention group. Thus, we have an opportunity to improve the delivery process of our intervention before its wider implementation. However, peer contact was initiated with all participants randomized to the intervention group. In the future, we aim to offer the Mom Supports Mom intervention universally in Czech maternity hospitals, but peer contact will only be initiated with women who express an interest. Further, The study design did not involve blinding of participants and peer consultants, as it was clear to the participants which group they belonged to. Only the outcomes raters were blinded. This is a limitation of the study design, given the nature of the intervention (peer support vs. care as usual). In our study, participants were randomly assigned to either the intervention or control group using a computer-generated randomization process, ensuring true randomization. However, allocation to treatment groups was not concealed, as participants were aware of their group assignment based on the intervention they received. While peer consultants knew which participants were assigned to the intervention group (since only this group received peer support), they also provided support to women outside the study. Therefore, they were unsure whether they were providing support to a participant in the study or not, which helps mitigate potential biases in the delivery of support. Both the intervention and control groups received treatment in line with their respective assignments, but aside from the peer support in the intervention group, no other differences were introduced in the treatment approach. We conducted a per-protocol analysis, including only participants who fully adhered to the intervention they were assigned to. Specifically, only participants who received peer support were included in the intervention group analysis. Another limitation of our work is that our peer counsellors did not sufficiently record information about the peer contacts as their main focus was on working with support users. Thus, we lacked information on the length of telephone contacts or detailed information on the support they provided. Therefore, we could not specifically analyse the effect of the amount of support provided, but we analysed all intervened participants in one group. Based on this experience, we recommend future researchers in the field of peer interventions to keep a detailed record of the support sessions that took place. Conclusion Peer intervention Mom Supports Mom, which follows up on screening for presence of symptoms of mental disorders after childbirth in maternity hospital, is effective in reducing depressive and anxiety symptomatology in postpartum women. It is also effective in increasing their health-related quality of life. As these effects can already be found at low-frequency peer support, our study has actual public health implications for Czech republic. The Mom Supports Mom can serve as a low intensity approach that is effective for mild illness and has potential to be scalable. Our current treatment approach often involves referring women for therapy and medical treatment; however, Mom Supports Mom offers a way to address mild illness that is both easily accessible and inexpensive. Our results can also help other non-western countries at a similar economic level as the Czech Republic to implement similar approaches. Peer intervention, following the screening for symptoms of mental disorders in maternity hospital, is effective in reducing depressive and anxiety symptomatology in postpartum women. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Sebela, A., Horakova, A., Nemcova, H., Kuklova, M., Noskova, E., Svancer, P., Byatt, N., Janovska, A., Hrdlickova, K. (2025). Mom supporting mom: Effective peer support intervention for women with postpartum psychological distress. Psychosocial Intervention, 34(3), 151-160. https://doi.org/10.5093/pi2025a12 Funding The research leading to this paper received funding from Czech Health Research Council under Grant Agreement No. NU21J-09-00064. Dr. Byatt has received salary and/or funding support from Massachusetts Department of Mental Health via the Massachusetts Child Psychiatry Access Program for Moms (MCPAP for Moms). Appendix "Mom Supports Mom" Peer Support Intervention – Methodology The target group for this method consists of women in the perinatal period (i.e., from pregnancy up to one year after birth) who are at risk of developing psychological difficulties, as identified through a positive result in a psychosocial stress screening. Fundamental Principles of Peer Support Peer consultants are individuals with personal lived experiences, which they can use to support individuals facing similar challenges. The principle of peer support assumes that a peer consultant can provide this support after training without being a professional expert in the field. During conversations with clients, they can help articulate their difficulties, identify risk factors, and suggest appropriate professional help. The relationship between peer consultants and clients is based on mutual understanding, reducing the perceived barrier between professionals and patients. Clients particularly appreciate the trustworthiness they perceive in relation to the lived experience of peer consultants, making them more likely to open up about their struggles. In mental health care, peer support is increasingly used as a valuable complement to primary professional care and both primary and secondary prevention. In practice, a peer consultant:
A peer consultant in the “Mom Supports Mom” intervention is a woman with experience of psychological difficulties during pregnancy or the first year after childbirth. Methods Used by Peer Consultants The primary tool of is an unstructured counseling conversation, conducted by phone. During interactions with clients, the peer consultant:
Step 1: Identifying Women at Risk of Developing Psychological Difficulties This step precedes the actual “Mom Supports Mom” intervention. Women at risk of psychological difficulties are actively identified through the screening conducted in maternity hospitals. Each woman who consents to completing the screening questionnaire is given a tablet to complete the questionnaire online. Woman is considered at risk if her score on the Edinburg Postnatal Depression scale is above 9. Within 10 minutes, the woman receives an email result indicating whether her responses suggest an increased risk of developing psychological difficulties. At-risk women in the intervention group are automatically contacted by a peer consultant. Step 2: Contacting Women at Risk of Developing Psychological Difficulties If a woman is automatically identified as at risk through the screening, she is contacted by phone within three working days. The caller is a peer consultant, who informs the woman of her screening results, asks about her current condition, and offers further support if needed. If the woman states during the call that she feels fine and/or declines further support, the peer consultant informs her about the possibility of reaching out in the future if her situation changes. If the woman accepts the offer of support, the peer consultant conducts an initial semi-structured interview to assess the severity of her difficulties. Step 3: Initial Semi-Structured Interview The initial semi-structured interview, along with the psychosocial screening results, helps assess the severity of the woman’s current condition. It identifies risk factors that indicate the need for immediate professional help and monitors commonly occurring difficulties that may lead to more severe mental health issues. Key components of the interview include:
If the woman wishes to continue receiving support, the peer consultant provides ongoing guidance based on sharing their own processed experience. The frequency of further consultations are determined through mutual agreement. The peer consultant ensures that the woman knows she can seek support at any time, even if she initially declines assistance. As part of the consultations, the peer consultant provides each woman with general recommendations regarding mental well-being during the perinatal period. They emphasize the importance of rest and relaxation, self-care, setting personal boundaries in childcare, and encourage the woman not to hesitate to ask for help from her surroundings. Step 5: Recording Contact with the Client The peer consultant maintains a simple database of clients which can be shared among multiple peer consultants in a given region. Clients are identified using an identification number assigned after completing the psychosocial screening. Each contact is recorded in the table, including the date and format of the consultation, the time spent, and the main topic discussed. Referral to Professional Support A key part of the peer consultant’s role is monitoring the availability of professional care in their region. Each peer consultant maintains contact with at least three professionals (psychologists and psychiatrists) who are familiar with the peer support initiative and with whom they have a long-term collaboration. If needed, the peer consultant provides the at-risk woman with contact information for these pre-selected professionals, which often facilitates faster access to professional care compared to women seeking support independently. Since seeking psychological or psychiatric help is often stigmatized, the peer consultant also plays a role in normalizing professional mental health care. They address doubts about seeking help, ease feelings of failure associated with reaching out for support and inform the woman about the effectiveness of professional treatment. The peer consultant facilitates contact with verified and accessible healthcare or psychological services if the woman reports:
Additional indications for referral to professional care include situations where:
A peer consultant also provides professional contact information if the woman explicitly requests it. Depending on the situation, they may refer her to a clinical psychologist, psychiatrist, crisis center, or another relevant service. In cases involving physical health concerns, they may also recommend contacting a general practitioner or gynecologist. For some women, psychological difficulties can become severe and life-threatening. Therefore, peer consultants must be trained in the basics of crisis intervention. If a peer consultant identifies acute and potentially life-threatening issues, they strive to sensitively guide the woman toward professional crisis support. Professional crisis intervention is recommended in the presence of the following risk factors:
| IntroductionMethodResultsDiscussionTarget GroupFundamental Principles of Peer SupportMethods Used by Peer ConsultantsStep 1: Identifying Women at Risk of Developing Psychological DifficultiesStep 2: Contacting Women at Risk of Developing Psychological DifficultiesStep 3: Initial Semi-Structured InterviewStep 4: Ongoing Peer SupportStep 5: Recording Contact with the ClientReferral to Professional SupportCrisis Intervention |
Cite this article as: Sebela, A., Horakova, A., Nemcova, H., Kuklova, M., Noskova, E., Svancer, P., Byatt, N., Janovska, A., & Hrdlickova, K. (2025). Mom Supporting Mom: Effective Peer Support Intervention for Women with Postpartum Psychological Distress. Psychosocial Intervention, 34(3), 151 - 160. https://doi.org/10.5093/pi2025a12
Correspondence: antonin.sebela@nudz.cz (A. Sebela).
Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS






