
Predictors of Treatment Resumption after Discharge in Alcohol and Cocaine Users
[Los predictores de la reanudaciĂłn del tratamiento tras el alta terapĂ©utica en consumidores de alcohol y cocaĂna]
José M. Martínez-González1, Alfonso Caracuel2, Raquel Vilar-López2, Elisardo Becoña3, & Antonio Verdejo-García4
1Centro Provincial de Drogodependencias de Granada, Spain; 2Mind, Brain and Behavior Research Center CIMCYC, University of Granada, Spain; 3Universidad de Santiago de Compostela, Spain; 4Turner Institute for Brain and Mental Health, Monash University, Melbourne, Australia
https://doi.org/10.5093/clh2025a14
Received 24 April 2024, Accepted 31 March 2025
Abstract
Objective: Treatment resumption is common in substance use, highlighting the clinical importance of predicting treatment outcomes. This study aimed to i) determine whether baseline variables previously identified as predictors are associated with treatment resumption and ii) evaluate the predictive value of discharge variables for treatment resumption. Method: Ninety-two outpatients (mean age 39.76, 84.8% male) treated for alcohol (60.9%) or cocaine (39.1%) addiction were assessed at baseline (sociodemographic, addiction history, psychopathology, and treatment-related variables) and discharge (psychological symptoms, impulsivity, irrational beliefs), with a follow-up that lasted nearly ten years. Results: No significant baseline differences were found between patients who resumed treatment and those who did not. However, a logistic regression model incorporating depression and craving-related beliefs at discharge showed a good fit (x2 = 10.030, p = .007, classification accuracy 76.6%). Conclusion: The findings suggest that irrational beliefs about craving and depressive symptoms significantly predict treatment resumption. Therefore, addressing these factors before discharge could reduce the likelihood of resumption.
Resumen
Objetivo: La reanudación del tratamiento es frecuente en el consumo de sustancias, lo que pone de relieve la importancia clínica de predecir los resultados de las intervenciones. Este estudio tiene como objetivos: i) determinar si las variables basales previamente identificadas como predictoras de resultado terapéutico se asocian con la reanudación del tratamiento después de haber recibido el alta terapéutica y ii) calcular el valor predictivo de las variables evaluadas en el momento del alta. Método: Se evaluó a 92 pacientes ambulatorios (edad media 39.76, 84.8% varones) tratados por trastornos por consumo de alcohol (60.9%) o cocaína (39.1%) al inicio del tratamiento (variables sociodemográficas, antecedentes de adicción, psicopatología y variables relacionadas con el tratamiento) y al recibir el alta terapéutica (síntomas psicológicos, impulsividad, creencias irracionales), con un seguimiento de la reanudación de tratamiento que duró casi diez años. Resultados: No se encontraron diferencias basales significativas entre los pacientes que reanudaron el tratamiento y los que no después de haber recibido el alta. Sin embargo, un modelo de regresión logística que incorporaba la depresión y las creencias relacionadas con el deseo intenso en el momento del alta mostró un buen ajuste (x2 =10.030, p = .007, precisión de la clasificación 76.6%). Conclusiones: Los resultados sugieren que las creencias irracionales sobre el deseo intenso y los síntomas depresivos predicen la reanudación del tratamiento. Por tanto, abordar estos factores antes del alta podría reducir la probabilidad de requerir un tratamiento futuro.
Palabras clave
Alcohol, CocaĂna, Alta, RegresiĂłn logĂstica, Predictores, ReanudaciĂłn del tratamientoKeywords
Alcohol, Cocaine, Discharge, Logistic regression, Predictors, Treatment resumptionCite this article as: Martínez-González, J. M., Caracuel, A., Vilar-López, R., Becoña, E., & Verdejo-García, A. (2025). Predictors of Treatment Resumption after Discharge in Alcohol and Cocaine Users. Clinical and Health, 36(3), 153 - 161. https://doi.org/10.5093/clh2025a14
Correspondence: rvilar@ugr.es (R. Vilar López).Alcohol and cocaine are among substances most widely consumed in Europe and are responsible for the highest number of admissions (European Union Drugs Agency, 2024; United Nations Office on Drugs and Crime, 2024). In Spain, 92.9% of the population has used alcohol in their lifetime, and 13% has used cocaine (Observatorio Español de las Drogas y las Adicciones [OEDA, 2024b]). Cocaine is the leading illegal drug for treatment admissions, accounting for 46.8% of cases (OEDA, 2023), while alcohol, the most commonly used psychoactive substance, represents 36.2% of treatment admissions (OEDA, 2024b). Psychosocial interventions remain the primary treatment approach for cocaine, alcohol, and other substance use disorders (SUD) (Ghafouri et al., 2024). However, these treatments continue to face high relapse rates. Studies report that relapse rates post-treatment range from 26% to 94% (Andersson et al., 2023; Betancourt et al., 2022) and most frequently occur within the first 12 months following discharge (McKetin et al., 2018; Schellekens et al., 2015). Empirical studies, reviews, and meta-analyses have yielded mixed findings regarding the variables that reliably predict treatment outcomes for patients with SUD. Recent systematic reviews and meta-analyses on predictors of treatment outcomes in SUD populations suggest that certain sociodemographic factors, such as lower education, as well as clinical variables, such as higher global illness and depressive or substance use symptom severity, are predictors of relapse (Solmi et al., 2023). Focusing specifically on alcohol use disorders, research indicates that psychopathological comorbidities, addiction severity, craving, negative emotions, and concurrent substance use are significant predictors of relapse (Sliedrecht et al., 2019). For individuals with cocaine use disorder, predictors of relapse include age, usage-related variables (such as years of use, craving levels, and withdrawal symptoms), baseline abstinence, neurocognitive function, treatment characteristics, and personality traits, including impulsivity. In contrast, the results are less consistent for factors such as education, employment status, and comorbid conditions (Palazón-Llecha et al., 2024). Other reviews have found that while substance use characteristics at baseline may predict relapse in cocaine users, no clear relationship has been identified between craving and mental health at baseline (del Palazio-Gonzalez et al., 2024). In short, studies on predictors of treatment outcomes in alcohol and cocaine users point to the involvement of various sociodemographic, consumption-related, psychopathological, and psychological factors. Discrepant findings in the literature likely result from differences in how variables are defined and measured and the high risk of bias observed in many studies (e.g., del Palazio-Gonzalez et al., 2024). A major source of inconsistency lies in the varied definitions of treatment outcome, which is most often associated with the term “relapse” but can also include measures of treatment retention, drop-out, or abstinence—terms that are often ambiguous and widely debated (Moe et al., 2022; Sliedrecht et al., 2022). An alternative way of defining treatment outcome is resumption, which has been proposed to overcome some limitations of previous concepts, such as ambiguity or self-reported data (Hansen et al., 2020). Importantly, although the prediction of resumption may facilitate disorder management and reduce social and economic burdens (Ghosh et al., 2022; Morel et al., 2020), few studies have focused on SUD (Morel et al., 2020), and even fewer on outpatients (Hansen et al., 2020). Moreover, given that alcohol and cocaine use account for the highest number of admissions, resumption studies are particularly relevant for these patients. It is also worth noting that most research on predictors of treatment outcomes in SUD has focused on factors assessed at baseline (McKay et al., 2013) and therefore, these are the factors included in the reviews on the subject (e.g. Palazón-Llecha et al., 2024; Solmi et al., 2023). These pretreatment predictors are highly valuable as they ultimately help to determine the appropriate type and intensity of treatment required for success (Loree et al., 2015). However, many of these variables—such as craving, psychiatric symptoms, and psychological variables—can be modified by the treatment itself. As a result, measures taken at treatment completion may offer a more accurate prediction of future relapse. This shift in focus could help explain some of the inconsistencies observed in studies investigating comorbid psychopathology as a predictor of relapse after discharge. For instance, research on personality disorders (PD) has yielded mixed findings regarding their impact on relapse rates in individuals with SUD. While some studies have found that PD comorbidity is associated with a higher likelihood of relapse (Mancheño-Velasco et al., 2024; Stetsiv et al., 2023), others report no significant relationship (Martínez-González, Vilar-López, & Verdejo-García, 2018; Newton-Howes et al., 2017; Pandey et al., 2021). Although PD has historically been associated with a higher (Cacciola et al., 1996; Verheul et al., 1998) and earlier risk of substance relapse after discharge (Thomas et al., 1999), recent systematic reviews and meta-analyses suggest that there is insufficient evidence to support a strong link between PD and treatment relapse in alcohol or cocaine use disorders and that studies that have reported such an association often present low-quality evidence (Adamson et al., 2009; Newton-Howes et al., 2017; Palazón-Llecha et al., 2024). Interestingly, while individuals with PD tend to have lower treatment retention rates, individuals who remain in treatment do not necessarily experience worse outcomes than individuals without comorbid conditions (Newton-Howes & Foulds, 2018). Moreover, several studies have demonstrated a relationship between baseline anxiety disorders (Moradinazar et al., 2020; Schellekens et al., 2015; Sinha, 2024) or depression (Andersson et al., 2019; Yedlapati & Stewart, 2018) and relapse. However, other studies have found no association between these conditions and subsequent relapses (Bauer et al., 2014; Böckmann et al., 2019; Davis et al., 2023; Martínez-González, Vilar-López, & Verdejo-García, 2018). These discrepancies may be related to symptom improvement resulting from the intervention itself. However, no studies have examined the predictive value of clinical or psychological variables assessed at the end of treatment. Such research could provide valuable insights for making more informed discharge decisions and improving long-term treatment outcomes. Another important consideration regarding the potential predictive value of baseline clinical variables is that most studies on individuals diagnosed with an SUD either exclude those with a comorbid mental illness or do not assess these conditions. As a result, much of the research on relapse that includes dual diagnoses has been conducted on individuals initially diagnosed with a mental illness who were subsequently assessed for substance use (Bradizza et al., 2006). This approach may limit the generalizability of findings, as it does not reflect the typical population served in SUD treatment centers. In addition to the factors mentioned above, emerging predictive variables from fields such as neuroimaging and genetics show promise (Palazón-Llecha et al., 2024). However, these methods are not yet widely accessible in clinical practice in many countries. Research identifying new relapse risk factors related to psychological variables could be particularly valuable for clinicians. In this regard, one promising area involves studying individuals’ beliefs about their drug use and craving (Martínez-González & Verdejo-García, 2012; Martínez-González et al., 2012). Based on the classic cognitive model, this line of research links addictive core beliefs to treatment outcomes and relapse (Beck et al., 2011). Finally, while numerous studies have examined predictors of treatment outcomes in SUD, to our knowledge only two have explored resumption based on variables at discharge. Böckman et al. (2019) found that higher symptom severity of mental disorders at discharge—but not baseline—predicted treatment resumption in patients with SUD over a one-year follow-up period. Ghosh et al. (2022) reported that improved clinical status at discharge negatively predicted five-year readmission among patients with alcohol use disorders. In short, very few discharge variables have been studied as predictors of treatment resumption in SUD. In conclusion, findings on relapse or treatment resumption after discharge in individuals with substance addiction highlight a range of inconsistent factors. Some, such as age and age of onset of use, are non-modifiable, while others, like education, are independent of treatment. However, certain factors can be targeted in intervention programs, and their impact can be assessed at discharge—a critical but relatively understudied time point—to predict treatment resumption. Therefore, this study aimed to: i) determine whether baseline variables previously identified as predictors of treatment outcomes (including sociodemographic factors, addictive history, comorbid psychopathology, and treatment-related variables) are associated with treatment resumption after discharge and ii) assess whether treatment resumption can be predicted based on variables assessed at discharge (psychological disorder symptoms, impulsivity, and irrational beliefs about substance use and craving). We hypothesized that all studied variables, both baseline and discharge-related, would predict treatment resumption, with the latter yielding stronger predictive results. Study Design A prospective observational cohort study design was used. Participants The recruitment was conducted at the Provincial Drug Dependence Center (Granada, Spain) between November 2010 and October 2018. This public outpatient center for the treatment of addictions belongs to the network of treatment centers of the regional government of Andalucía. Consecutive sampling included patients with alcohol or cocaine dependence disorder, according to DSM-IV-TR (APA, 2000), who received a therapeutic discharge during this period (N = 231). All discharged patients were invited to participate in the study, and 39.82% (n = 92) completed and returned the questionnaires along with written consent. Thus, the final sample consisted of 92 participants. The study did not include patients who were discharged but did not return the questionnaires and/or informed consent (n = 139; 60.18%). The mean time from discharge to follow-up assessment of treatment resumption was 68.24 months, ranging from 12 to 117 months (one to nearly ten years). Assessment Instruments Information on sociodemographic, addictive history, comorbid psychopathology, and treatment-related variables was obtained by consulting the Andalusian Plan on Drug Addiction and Addictions Information System (Sistema de Información del Plan Andaluz de Drogodependencias y Adicciones [SiPASDA, n.d.]) This centralized database is shared by all public and subsidized addiction treatment centers within the Andalusian addiction treatment network. Through this system, we collected sociodemographic data (age, gender, education, employment status), addictive history (type of substance, age at first consumption, age of onset of abusive use, time between onset of abusive use and start of treatment), comorbid psychopathology (personality disorder, Axis I disorder, dual pathology), and treatment-related data (previous treatment/s and amount, treatment modality, duration of treatment). Additionally, we could track whether patients resumed treatment at any of these centers after discharge. Structured Clinical Interview for DSM IV Axis I (SCID-I; First et al., 1997; Spanish version, First et al., 1999) This was used to diagnose comorbid psychopathology at the beginning of treatment according to DSM-IV-TR diagnostic criteria (APA, 2000). The International Personality Disorder Examination (IPDE; Loranger et al., 1994; Spanish version by López-Ibor, 1996) It was used to diagnose PD, which facilitates the analysis of possible symptom overlap between drug addiction and personality psychopathology. The instrument has demonstrated good reliability, with Kappa indices for schizotypal, compulsive personality, histrionic, borderline, and antisocial personality disorders ranging from .70 to .96 (Loranger et al., 1994). General Health Questionnaire (GHQ-28; Goldberg & Hillier, 1979; Spanish version by Lobo et al., 1986) This self-report screening measure detects psychological disorder symptoms through the scores of its four subscales (somatic symptoms, anxiety/insomnia, social dysfunction, and depression), where lower scores indicate lower levels of symptoms. Analysis of the questionnaire’s psychometric properties revealed adequate reliability of the subscales and the questionnaire (α = .948) (Pérez-Moreno et al., 2010). Impulsive Behavior Scale (UPPS-P; Whiteside & Lynam, 2001; Spanish version by Verdejo-García et al., 2010) This instrument consists of 59 items divided into five subscales: positive urgency and negative urgency (tendency to experience strong impulses under conditions of positive or negative affect, respectively), lack of premeditation (tendency to reflect on the consequences of an act before engaging in that act), lack of perseverance (ability to remain focused on a task that may be boring or difficult), and sensation seeking (tendency to enjoy and engage in exciting activities and openness to novel experiences that may or may not be dangerous). Questionnaire of Core Beliefs related to Drug Use and Craving (BeDRUC; Martínez-González, Vilar-López, Lozano-Rojas, et al., 2018) This instrument consists of 25 Likert-type response items, 17 of which assess the presence of nuclear beliefs related to consumption and eight that assess the experience of craving. Factor analysis has revealed that consumption-related beliefs are grouped into four factors: 1) what the person believes they will not be able to accomplish in the absence of drug consumption, 2) the lack of with-drawal from consumption, 3) the conditions that must be present to relapse into consumption, and 4) the idea that consumption is the only way to feel good. The internal consistency of these factors is highest for the first three (Alpha values of .84, .87, and .87 respectively) and lowest for the fourth (.67). Beliefs about one’s own craving experience were grouped into three factors: 1) negative emotions as precipitants of craving, 2) difficulties attributed to craving coping, and 3) positive emotions. The first factor presents the highest internal consistency (.82), followed by the second (.73) and the third (.62). In the analyses of the present study, the presence (or not) of a risk factor was included in each of the four types of beliefs about consumption and each of the three types of beliefs about craving. The presence of a risk factor for each type of belief was confirmed when the participant obtained a score higher than 1, which indicates that they identified with at least two of the core beliefs of that type. Intervention The essential components of the intervention were described in two books published by the clinical psychologist who administered the treatment (Becoña et al., 2020; Martínez-González & Verdejo-García, 2014). Thus, the intervention, which followed the cognitive-behavioral model, addressed the following critical components: education of patients in the cognitive model, training in cognitive and behavioral strategies, setting realistic and specific goals, management of craving, management of general life problems, crisis intervention, attention to other concomitant Axis I and/or II disorders, and intervention with family members for case follow-up. Patients were specifically trained to improve contingency management, coping skills, stress management, relaxation, social skills and assertiveness, communication skills, life skills, anger management, and relapse prevention. All interventions were conducted according to established clinical guidelines based on scientific evidence for the treatment of alcohol and cocaine addiction (e.g., Pascual-Pastor et al., 2014; Terán-Prieto et al., 2008) and administered according to the essential components of Beck’s model (Beck et al., 2011). Furthermore, clinical individual adaptations were adopted whenever necessary, particularly for patients with comorbid psychopathology. Specific adaptations for treating patients with personality disorders are described extensively in a publication by the authors (Martínez-González & Verdejo-García, 2014). These adaptations account for the irregular and unpredictable progression of such patients in overcoming addictive beliefs, their unique role of drug use, their approach to managing cravings, and their coping strategies throughout treatment. The treatment was carried out at the individual and group level. Patients who underwent group treatment attended a weekly session, while those receiving individual treatment attended sessions every two weeks during the first three months, after which they attended psychotherapy sessions once a month. However, session frequency varied based on individual needs, including patient progress, crisis episodes, or comorbid psychopathology. The therapist held a Ph.D specializing in Clinical Psychology and had over 30 years of experience working in public addiction treatment centers. Procedure Upon admission to treatment, all participants underwent an assessment of addictive behavior and comorbid psychopathology conducted by the same clinical psychologist who later administered their treatment. This initial assessment took place over two sessions, followed by outpatient treatment sessions. All patients discharged from therapy during the study recruitment period (November 2010 to October 2018) were asked to complete evaluation questionnaires. These were distributed during the penultimate session, to be completed at home and returned either at the final session or in the following days. Therapeutic discharge was granted based on the following criteria: maintaining abstinence for at least 12 months, verified through unannounced urine toxicology tests for alcohol or cocaine metabolites; absence of craving for at least three months; demonstrating effective relapse prevention strategies in recent months (Becoña et al., 2020); maintaining healthy habits to prevent relapse; reporting good quality of life; and showing significant improvement in psychopathology when present. These criteria were confirmed with input from the patient’s family. To identify participants who had resumed treatment after discharge at least 12 months before the study, an inquiry was made in the SiPASDA system, with data collected between October 2019 and June 2020. Due to the comprehensive coverage of this system, treatment resumption data was available for all participants. The data supporting this study’s findings are available on request from the corresponding author (RVL). This study was not preregistered. All participants were asked for informed consent for their participation in this research, which has the certificate of authorization from the Human Research Ethics Committee of the University of Granada (no. 295/CEIH/2017). Data Analysis To address the first objective, participants were categorized based on whether they resumed treatment at follow-up (yes/no). Independent t-tests were conducted to determine the differences between those who resumed treatment and those who did not in terms of sociodemographic variables (age, gender, education, employment status), addictive history (type of substance, age at first consumption, age of onset of abusive use, time between onset of abusive use and start of treatment), comorbid psychopathology (personality disorder, Axis I disorder, dual pathology), and treatment-related variables (previous treatment/s and amount, treatment modality, duration of treatment, follow-up period). Additionally, correlation analyses were conducted to explore relationships between baseline variables and treatment resumption after discharge. For the second objective, correlation analyses were conducted between variables assessed at discharge and treatment resumption to identify potential predictors, which were subsequently included in a hierarchical logistic regression analysis. There were no missing data. All statistical analyses were performed using SPSS Version 28. Regarding the characteristics of the sample, 84.8% (n = 78) were men, and 15.2% (n =14) were women. In terms of the substance used, 60.9% (n = 56) had entered treatment for alcohol addiction and 39.1% (n = 36) for cocaine addiction. According to the International Standard Classification of Education (ISCED), most (67.78%) had (low or upper) secondary education, followed by 16.67% with primary education or less and 15.5% with a bachelor’s degree. Concerning employment status, 54.3 % (n = 50) were working at the time of starting treatment. The mean age of the participants at the start of treatment was 39.76 years (range = 20-64, SD = 10.59). The mean age at first use was 18 years (range = 8-32, SD = 3.99), while the mean age at the onset of abusive consumption was 27.35 years (range = 16-46, SD = 7.961). The mean time between initiation of use and the start of treatment was 26.68 years (range = 1-56, SD = 12.54), while the mean number of years between the onset of abusive consumption and the start of treatment was 17.11 years (range = 1-44, SD = 11.19). For 66.3% (n = 61) of the sample, this was the first time they had undergone treatment. The mean duration of treatment received was 16.83 months (range = 5 to 74, SD = 11.28). Of the sample, 51.1% (n = 47) were treated in groups, and the rest individually. The median number of sessions attended by participants was 31 sessions (range = 2 to 118). Over the study period, 31.5% of the sample (n = 29) resumed treatment, with a mean time of 32.48 months after discharge (range = 6-85, SD = 22.85). At the start of treatment, 56.5% (n = 52) had psychopathological comorbidity, of which 37% (n = 34) had a PD and 39.1% (n = 36) had Axis I psychopathology (see Table A1 in Appendix). Concerning the first objective, Student’s t-tests revealed no significant differences in sociodemographic variables, consumption history, comorbid psychopathology, and treatment characteristics between those who resumed treatment and those who did not (see Table 1). Table 1 Sociodemographic, Clinical and Treatment-related Variables of Substance Users with Treatment Resumption and not Resumption after Discharge. Comparisons between Groups and Correlation between These Variables and Treatment  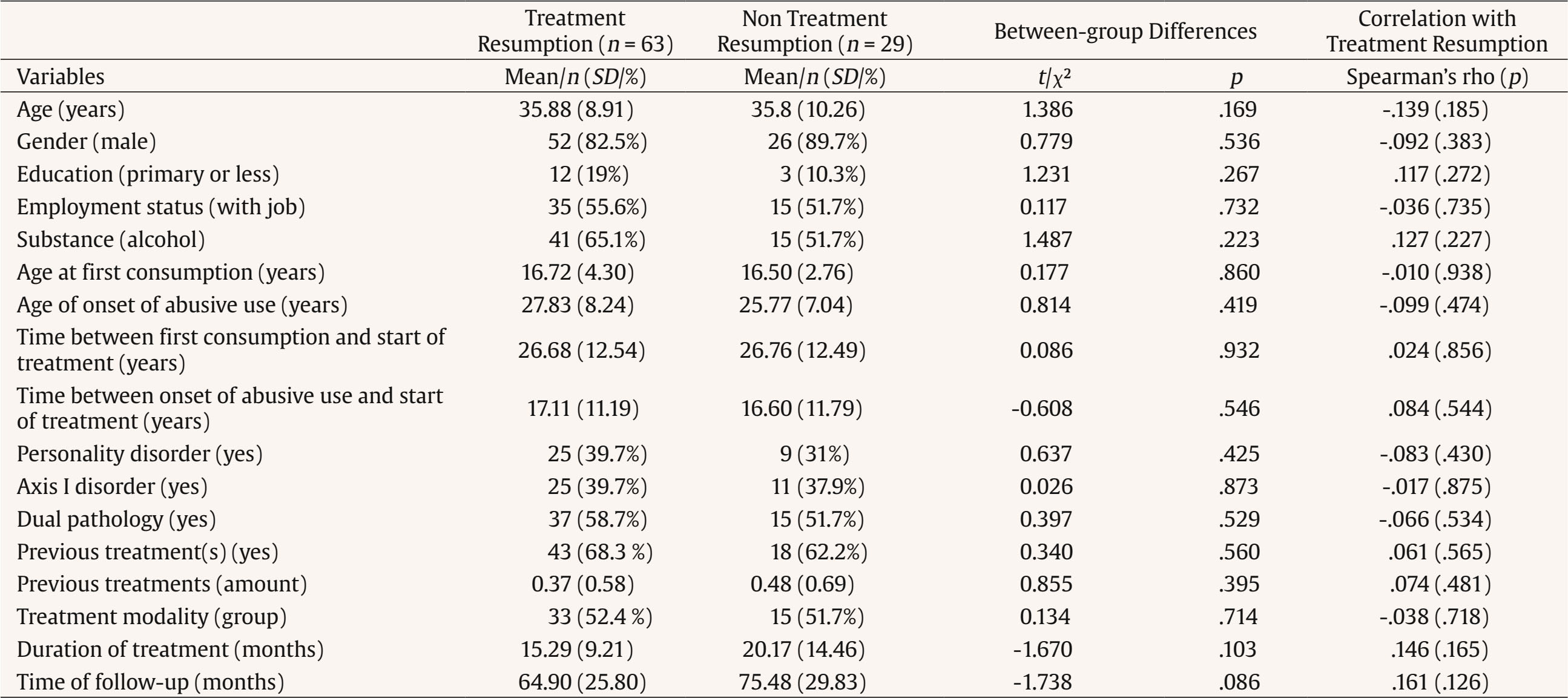 Regarding the second objective, bivariate correlation analyses were conducted between variables measured at discharge and treatment resumption (Table 2). Significant associations were found for the severe depression subscale of the GHQ-28 (ρ = .249, p = .017) and Factor 2 of beliefs about craving from the BeDRUC questionnaire (ρ = .237, p = .027). A logistic regression analysis included these variables as independent factors to predict treatment resumption. The logistic regression model demonstrated a good fit, as indicated by a non-significant Hosmer-Lemeshow test (see Table 3). The model’s overall chi-square test was significant, with Nagelkerke’s R2 indicating that 15.7% of the variance in treatment resumption was explained by the model. The classification accuracy was 75.6%. Statistically significant predictors for explaining treatment restart were the depression score from the GHQ questionnaire (p = .022 for Walt’s statistic) and the second risk factor for beliefs about craving, that is, beliefs about difficulties attributed to craving coping (p = .043). Table 2 Correlation between Variables Measured at Discharge and Resumption of Treatment after Discharge  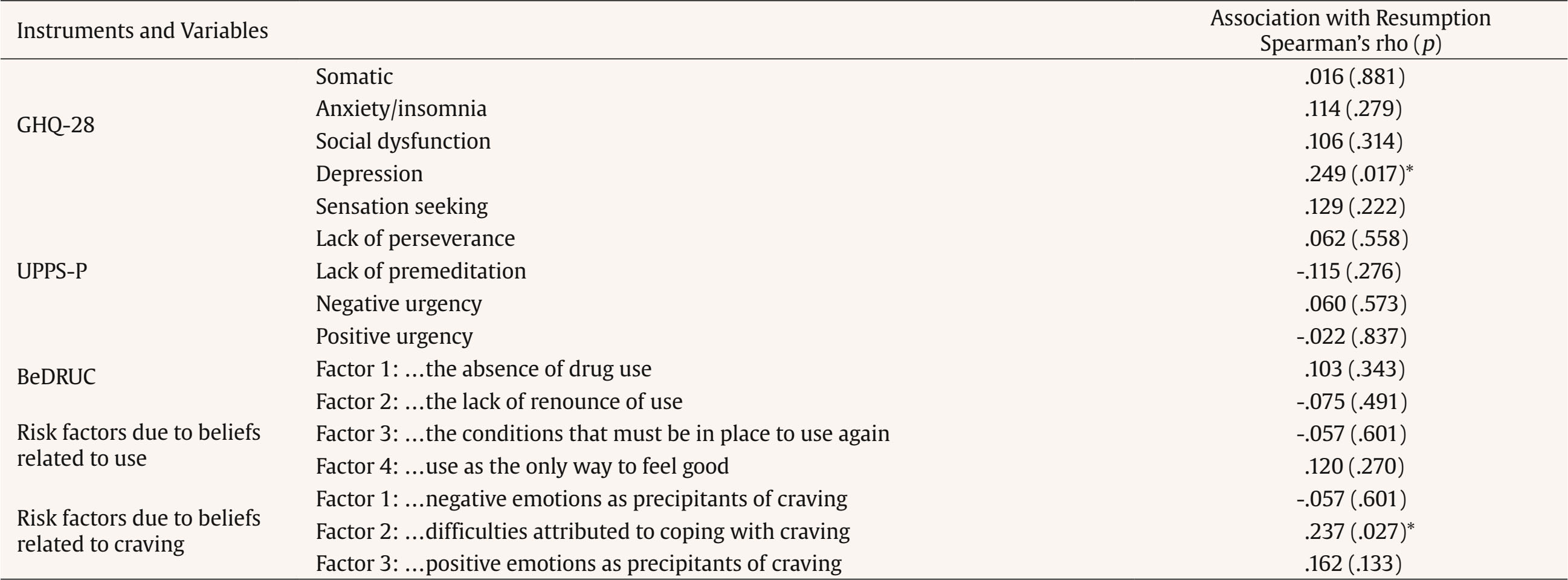 Note. GHQ-28 =General Health Questionnaire-28 (Goldberg & Hillier, 1979); UPPS-P = Impulsive Behaviour Scale (Whiteside & Lynam, 2001); Beliefs about consume and Beliefs about craving: Questionnaire of Core Beliefs related to Drug Use and Craving (Martínez-González, Vilar-López, Lozano-Rojas, et al., 2018). *significant p-value. Table 3 Hierarchical Binary Logistic Regression Predicting Resumption of Treatment Based on Variables Measured at Discharge  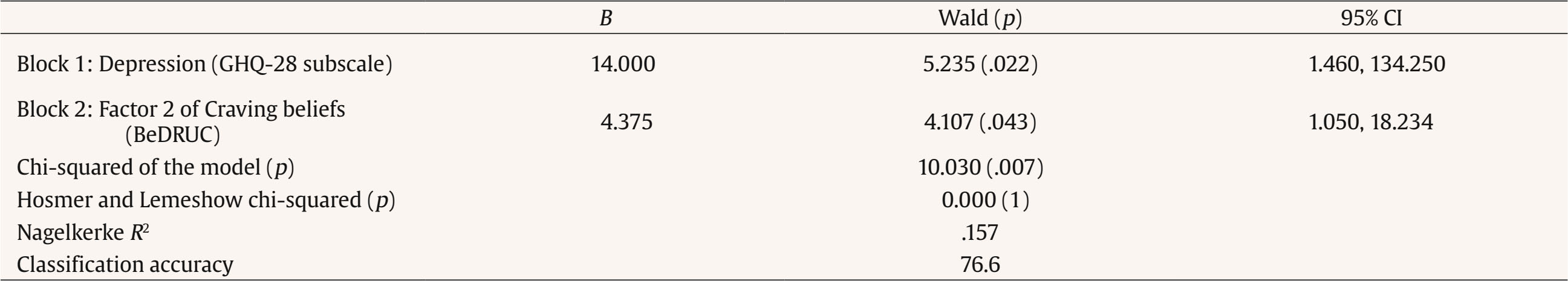 Note. GHQ-28 = General Health Questionnaire-28 (Goldberg & Hillier, 1979); Factor 2 of Craving beliefs = risk factor due to beliefs related to difficulties attributed to coping with craving; BeDRUC = Questionnaire of Core Beliefs related to Drug Use and Craving (Martínez-González et al., 2018). A preliminary multiple linear regression confirmed the independence of errors and the measure of multicollinearity. Satisfactory results were obtained for Durbin-Watson statistics (2.066, within the acceptable range of 0-4), tolerance (T = .993, above the cutoff of .10), and variance inflation factor (VIF = 1.007, below the cutoff of 5.0) for both variables. This study aimed to determine whether baseline variables previously identified as predictors of treatment outcomes are associated with treatment resumption after discharge and to assess whether variables measured at discharge—such as psychological disorder symptoms, impulsivity, and irrational beliefs about substance use and craving—could predict resumption. The findings only partially support our hypotheses. Specifically, depressive symptoms and irrational beliefs related to craving at discharge predicted treatment resumption. However, other psychological symptoms, impulsivity, and core beliefs about drug use showed no significant association with resumption. Furthermore, the results indicate that patients who resumed treatment after discharge were comparable to those who did not in terms of baseline sociodemographic factors, addiction history, comorbid psychopathology, and treatment characteristics. Previous research has shown that both sociodemographic factors and addiction history are significant predictors of treatment outcomes (del Palazio-Gonzalez et al., 2024; Palazón-Llecha et al., 2024; Sliedrecht et al., 2019; Solmi et al., 2023), measured as retention or dropout rates and the maintenance of abstinence during treatment. However, our data suggest that after discharge, variables not modifiable by treatment—such as age, gender, education, employment status, age at first use, age of onset of abusive use, and the time between the onset of abuse and the start of treatment—do not significantly predict treatment resumption, which is consistent with previous research (Böckmann et al., 2019). Furthermore, other modifiable factors, including psychiatric comorbidity, also do not appear to be associated with treatment resumption after discharge. Several studies have identified the presence of psychopathological and personality disorders at the initiation of treatment as predictors of subsequent relapse (Zikos et al., 2010). In contrast, our findings are consistent with studies finding no such direct relationship (Martínez-González, Vilar-López, & Verdejo-García, 2018; Newton-Howes et al., 2017; Pandey et al., 2021). Our results suggest that patients diagnosed at the start of treatment are not at greater risk of post-treatment relapse. This outcome may be related to the fact that the psychopathology identified at the beginning of treatment is addressed using an integrated intervention model (Martínez-González & Verdejo-García, 2014), leading to diminished or resolved symptoms before discharge, which may minimize the risk of relapse. In accordance with this hypothesis, previous research in SUD patients has demonstrated that improved clinical status at discharge reduced the odds of readmission (Ghosh et al., 2022) and that the severity of mental disorders at discharge—but not at baseline—predicted readmission (Böckmann et al., 2019). Regarding treatment characteristics, previous studies found that patients treated over a shorter timeframe (2-4 months) show higher rates of relapse (Andersson et al., 2019) and that the combination of individual and group sessions yielded better retention rates (Siqueland et al., 2002). Nevertheless, neither treatment duration nor modality was associated with treatment resumption in our results, consistent with previous research (Böckman et al., 2019; Ghosh et al., 2022). A possible explanation is that once patients receive the appropriate modality and number of sessions needed for therapeutic discharge, these variables no longer influence the likelihood of relapse or treatment resumption. In short, previous literature has reported mixed results regarding the predictive value of sociodemographic variables, addiction history, comorbid psychopathology, and treatment-related variables in determining therapeutic outcomes. A possible explanation for these discrepancies is the variation in outcome measures used across studies (e.g., relapse, abstinence). In this regard, our results—showing no significant associations between baseline variables and treatment resumption—are consistent with the limited previous research specifically focused on predicting treatment resumption in SUD (Böckmann et al., 2019; Ghosh et al., 2022). Our results also indicate that impulsivity at discharge is not associated with treatment resumption. It is important to note that the mean scores for impulsive behavior at the end of treatment in our sample were similar to those found in the general population (Albein-Urios et al., 2012). Previous studies involving SUD patients have reported high levels of impulsivity at treatment initiation (Albein-Urios et al., 2014). We do not consider our findings to contradict other studies that have identified an association between impulsivity at treatment initiation and treatment outcomes (Albein-Urios et al., 2012; Loree et al., 2015; Sliedrecht et al., 2021). Rather, we suggest that impulsivity is no longer a risk factor for relapse when it does not exceed normative levels at discharge. Previous research on the relationship between depression and relapse has yielded mixed findings. While some studies have found that neither a lifetime nor current diagnosis of depression nor the presence of depressive symptoms predicts relapse (Böckmann et al., 2019; Davis et al., 2023; Mancino et al., 2014; Martin et al., 2010; Sánchez-Hervás et al., 2012), a recent systematic review (Solmi et al., 2023) reported that the severity of depressive symptoms is a transdiagnostic predictor of relapse across various mental disorders. In the context of cocaine use, previous studies have shown that the persistence of depression following treatment is linked to poorer substance use outcomes (Greenfield et al., 1998; Stulz et al., 2011) and a decreased likelihood of remaining abstinent (McKay et al., 2013). Depression also predicts treatment readmission for alcohol use disorder (Yedlapati & Stewart, 2018). Consistent with these findings, our results indicate that the level of depressive symptomatology at the end of treatment is a significant predictor of treatment resumption (McKay et al., 2013). Given the mixed findings on depression and SUD outcomes, researchers have emphasized the need to examine moderators of this relationship (Argyriou et al., 2023). Our findings provide evidence of a synergistic interaction between depression and craving-related beliefs in predicting treatment resumption after discharge. Importantly, the mean score for depressive symptoms among participants at the end of treatment was very similar to that of the general population (Albein-Urios et al., 2012). These results suggest that even when patients maintain adequate emotional symptom levels, holding one or two irrational beliefs about coping with cravings significantly increases the risk of treatment resumption after discharge. The specific beliefs associated with this factor—such as “If it gets into my head, I can’t help doing it” or “It is difficult for me to cope with craving”—highlight the challenges patients face in managing cravings. In turn, more severe depressive symptoms compared to the general population could reinforce these irrational beliefs, making it harder for individuals to resist consumption when experiencing certain levels of craving. Thus, holding active irrational beliefs about the difficulty of coping with cravings may further worsen mood when it is already suboptimal. Similarly, even mild depressive symptoms, acting synergistically with negative beliefs, may prevent the application of coping strategies learned during therapy from dealing with cravings. Consistent with this idea, scores on the GHQ-28 have previously been linked to these beliefs (Martínez-González & Verdejo-García, 2012) and treatment outcomes, including lower treatment effects or non-clinically relevant improvements in SUD (Vergara-Moragues & González-Saiz, 2020). The relationship between substance use and depressive symptoms can be explained by multiple hypotheses that are not mutually exclusive, ranging from bidirectional causality (Lai et al., 2015), to the reward circuit and stress system hypothesis (Koob & Volkow, 2016), or the neurotoxic effect of substances (Brady & Sinha, 2005). The findings of the present study have clinical implications for strategies that could complement the standard discharge procedure. Specifically, while standard discharge protocols are typically applied when cravings are absent, this approach may underestimate the risk of treatment resumption. Our results suggest that assessing irrational beliefs about coping with future cravings at discharge could improve risk evaluation and help identify patients who may benefit from additional post-discharge support. This research has certain limitations. First, the sample size is small, because only around 40% of eligible patients submitted their questionnaires at discharge, limiting statistical power. A larger sample would improve the reliability of findings and reduce the risk of bias. Another potential limitation is the variation in the follow-up period for participants (ranging from 12 months to almost 10 years). However, no significant association was found between treatment resumption and time since discharge. Additionally, a minimum 12-month follow-up period is enough to capture most relapses (i.e., Betancourt et al., 2022; Guliyev et al., 2022). Notably, the sample included very few women (15%), precluding a gender-based analysis. However, this percentage aligns with national treatment rates for cocaine (15%) and alcohol (21%) use (OEDA, 2023b), suggesting that the sample is representative of typical treatment-seeking populations. Nonetheless, treatment resumption predictors may differ between men and women, making it imperative for future studies to explore gender-specific risk factors. Additionally, conducting telephone interviews to assess patients’ status at the time of evaluation would have been beneficial for understanding relapse processes, including the role of social relationships and post-discharge substance use patterns. It is also important to note that all interventions were conducted by the same therapist, which could introduce bias into the results. Additionally, because therapy was adapted to individual needs, some variability in treatment delivery was inevitable. However, all interventions followed standard practices implemented in public drug addiction centers (see Procedure section). Future studies should replicate our findings and further explore the role of irrational beliefs and their impact on mood in relation to therapeutic success and the prevention of relapse or treatment resumption in SUD. This study also has two key strengths. First, some participants were tracked for up to ten years after discharge, providing valuable insights into long-term treatment outcomes. Second, unlike most prior research, this study focused on psychological variables assessed at discharge, making a novel contribution to the literature on predicting therapeutic outcomes in SUD treatment. In conclusion, our findings suggest that depressive symptoms and beliefs about the perceived difficulty of managing cravings could predict the likelihood of treatment resumption, even after a long period has elapsed since discharge. Therefore, from a clinical standpoint, assessing these indicators before making discharge decisions could help identify patients at higher risk of relapse and treatment resumption, allowing for more effective post-treatment interventions. Conflict of Interest The authors of this article declare no conflict of interest. Acknowledgments We wish to thank the professionals of the Andalusian Plan on Drugs and Addictions Information System of the Andalusian Regional Government for allowing us to consult the information related to the patients in the sample. Cite this article as: Martínez-González, J. M., Caracuel, A., Vilar-López, R., Becoña, E., & Verdejo-García, A. (2025). Predictors of treatment resumption after discharge in alcohol and cocaine users. Clinical and Health, 36(3), 153-161. https://doi.org/10.5093/clh2025a14 References |
Cite this article as: Martínez-González, J. M., Caracuel, A., Vilar-López, R., Becoña, E., & Verdejo-García, A. (2025). Predictors of Treatment Resumption after Discharge in Alcohol and Cocaine Users. Clinical and Health, 36(3), 153 - 161. https://doi.org/10.5093/clh2025a14
Correspondence: rvilar@ugr.es (R. Vilar López).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







