
Spanish Adaptation and Validation of the Recovery Process Inventory (RPI) in People with Mental Disorders
[Adaptación y validación de la versión en español del Inventario del Proceso de Recuperación (RPI-S) en población con trastorno mental]
Nekane Balluerka1, Arantxa Gorostiaga1, Hernán María Sampietro2, 3, & Jone Aliri1
1University of the Basque Country UPV/EHU, Spain; 2University of Barcelona, Spain; 3ActivaMent Catalonia Association, Spain
https://doi.org/10.5093/clh2025a12
Received 23 August 2024, Accepted 4 March 2025
Abstract
Backgorund: This study aimed to adapt and obtain validity evidence of the Spanish version of the Recovery Process Inventory (RPI-S) underlining the importance of hope and social support in personal recovery. The RPI-S was developed through a systematic process, ensuring semantic, linguistic, and contextual equivalence to the original instrument. Method: The psychometric properties were tested with 266 participants with severe mental disorders, following STROBE guidelines. Confirmatory factor analysis supported a four dimensions structure for assessing personal recovery. Results: The RPI-S showed evidence based on relations to other variables and evidence based on internal structure. Conclusions:The findings suggest that the RPI-S is a reliable tool for assessing recovery in Spanish-speaking people with severe mental disorders, highlighting the critical roles of hope and social support in recovery.
Resumen
Introducción: El objetivo del estudio fue adaptar y obtener evidencias de validez de la versión en español del Inventario del Proceso de Recuperación (RPI-S) subrayando la importancia de la esperanza y el apoyo social en la recuperación personal. El RPI-S se elaboró a través de un proceso sistemático, asegurando la equivalencia semántica, lingüística y contextual con el instrumento original.Método: Las propiedades psicométricas se comprobaron en 266 participantes con trastornos mentales graves, siguiendo las directrices STROBE. El análisis factorial confirmatorio avaló una estructura de cuatro dimensiones para evaluar la recuperación personal. Resultados: El RPI-S mostró evidencias de validez de relación con otras variables y evidencias basadas en su estructura interna. Conclusiones: Los resultados indican que el RPI-S es una herramienta fiable para evaluar la recuperación en personas hispanohablantes con trastornos mentales graves, destacando el papel crítico que juegan en la recuperación la esperanza y el apoyo social.
Palabras clave
Adaptación transcultural, Propiedades psicométricas, Trastorno mental severo, Recuperación en salud mental, Cuestionario de salud del pacienteKeywords
Cross-cultural adaptation, Psychometric properties, Severe mental disorder, Mental health recovery, Patient health questionnaireCite this article as: Balluerka, N., Gorostiaga, A., Sampietro, H. M., & Aliri, J. (2025). Spanish Adaptation and Validation of the Recovery Process Inventory (RPI) in People with Mental Disorders. Clinical and Health, 36(3), 145 - 152. https://doi.org/10.5093/clh2025a12
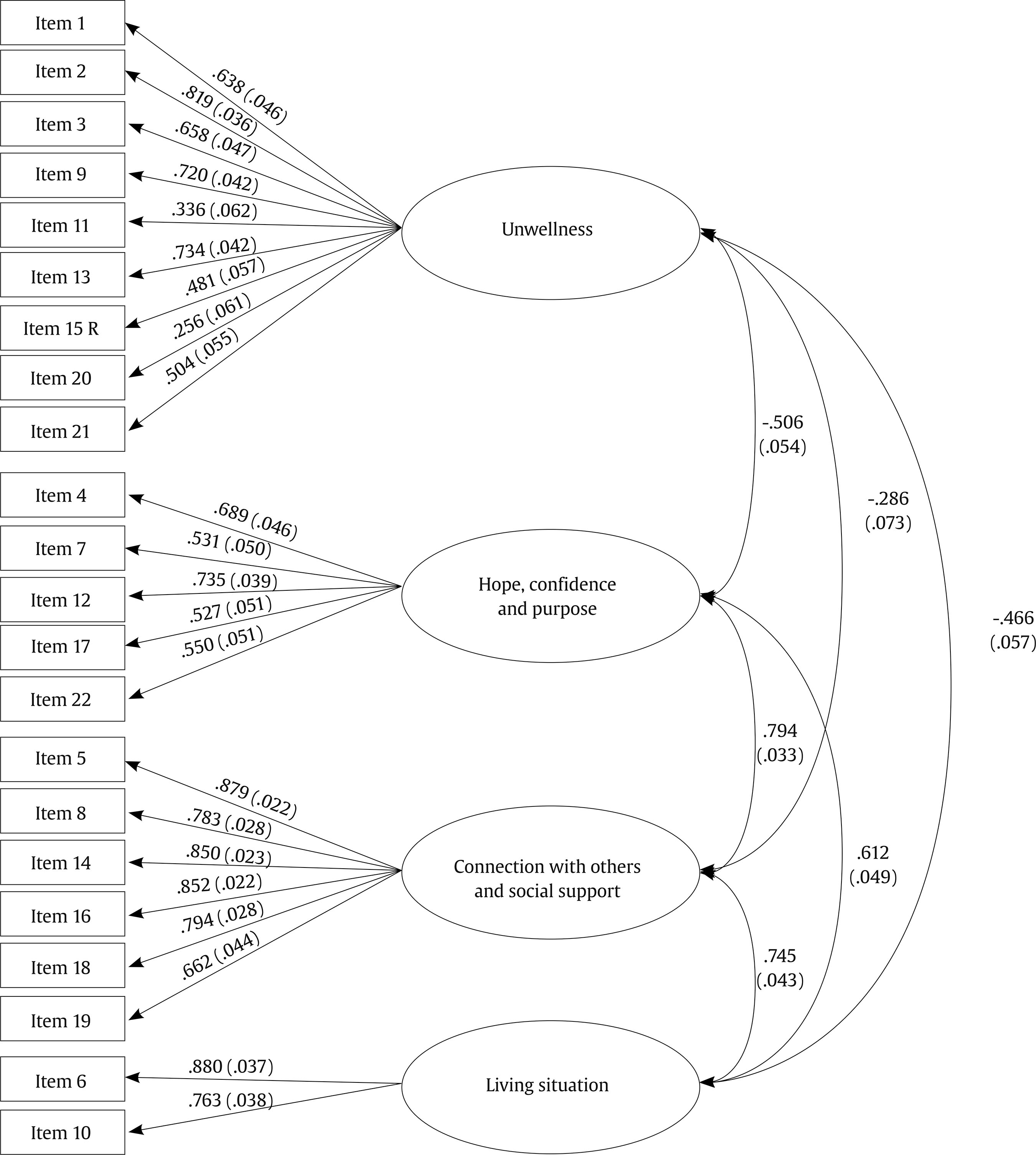
Correspondence: nekane.balluerka@ehu.eus (N. Balluerka).Nowadays, the World Health Organization highlights that mental health services should be recovery-oriented, community-based, person-centred, and compliant with human rights (World Health Organization [WHO, 2021]). From this perspective, recovery-oriented means that rather than focusing only on symptom remission and the restoration of previous levels of functioning, the main goal of the intervention should be to promote well-being and life satisfaction, to foster hope, and to help people have a project of life and make meaningful contributions to society. To address the issue of polysemy surrounding the concept of recovery and establish an empirically based conceptual framework, Leamy et al. (2011) developed a systematic review and narrative synthesis of 97 previous publications that had defined the concept. They identified five key elements, termed the CHIME framework: (a) connections with others and with the Community, (b) Hope and optimism about the future, (c) a positive sense of one’s own Identity, (d) a Meaning and purpose in life, and (e) Empowerment to have control over own life. The CHIME framework has gained increasing international consensus as a reference for setting the goals of recovery-oriented interventions (Penas et al., 2020). This conception of recovery has been termed personal recovery (Leamy et al., 2011; Slade et al., 2012) to distinguish it from clinical recovery, which focuses on symptoms and functionality. Considering that they are different constructs, the literature highlights that they need to be assessed independently (Van Eck et al., 2018). Regarding personal recovery, a recent scoping review of recovery planning tools found that hope and social support were among the most commonly evaluated variables (Sampietro et al., 2022). This is because they are seen as both prerequisites for recovery and indicators of recovery. Hope, which is the belief in the possibility of recovery, is one of the guiding principles (Substance Abuse and Mental Health Services Administration [SAMHSA, 2011]) and a subjective outcome of the recovery process (Slade et al., 2014). Some authors argue that hope is central because it acts as a catalyst for change and enables the other factors involved in recovery to take hold (Acharya & Agius, 2017). In addition, a relationship has been found between chronicity, measured by the severity and persistence of symptoms, and hopelessness (Hayes et al., 2017). Social support is also considered a guiding principle (SAMHSA, 2011) and a social outcome of the recovery process (Slade et al., 2014). Individuals do not recover in isolation, but with the support of relationships and social networks. Several systematic reviews have provided evidence of the link between social support and recovery, suggesting that social support acts as a protective element in people’s lives (Bjørlykhaug et al., 2022). Since 2011, various systematic reviews have been published with the aim of identifying psychometric instruments that measure the personal recovery construct, in general (Burgess et al., 2011; Penas et al., 2019; Scheyett et al., 2013; Shanks et al., 2013; Sklar et al., 2013), for a specific diagnosis (Cavelti et al., 2012), or a experience such as psychosis (Law et al., 2012). One of the instruments that appear in all these reviews and that is usually recommended to be used by clinicians and researchers in the discussions of these studies, is the Recovery Process Inventory (RPI) (Jerrell et al., 2006). The RPI is a 22-item scale aimed to facilitate self-assessment of the personal recovery process, and has been described as “a brief, easily administered but psychometrically sound instrument” (Jerrell et al., 2006, p. 472). In these systematic reviews, the RPI appears as one of “the strongest instruments reviewed” (Scheyett et al., 2013, p. 300) for its psychometric properties. In this regard, in both reviews made by Burgess et al. (2011) and more recently by Penas et al. (2019), the authors followed similar steps in the inclusion and exclusion criteria until arriving at the final list of the best instruments to assess personal recovery. Following this selection process, it is highlighted that the RPI explicitly measures domains related to personal recovery, is brief and easy to complete, takes users’ perspectives into account (was created by or with their collaboration), yields quantitative data, has been scientifically tested, and demonstrates sound psychometric properties. Furthermore, the study by Burgess et al. (2011) adds that the RPI is acceptable to consumers and promotes dialogue between consumers and providers. Finally, the review by Penas et al. (2019) highlights that it does not have a Spanish adaptation. Given that the international public mental health policies in Spanish-speaking countries are promoting a paradigm shift towards a recovery approach in which hope and social support are key factors, and that Jerrell et al.’s (2006) instrument has not yet been translated and validated into Spanish, the main purpose of this study has been to develop the Spanish version of the RPI (RPI-S), providing evidence of its validity among users of mental health services in the Spanish cultural context. Linked to validity evidence based on the relationship between the RPI-S measures and other variables, we aimed to demonstrate the relevance of hope and social support to achieve recovery. Regarding evidence based on the internal structure of the RPI, although the only structure that has received empirical support in previous studies has been the six-factor structure proposed by Jerrell et al. (2006), in the present study we also decided to test the fit of a four-factor structure reflecting a more parsimonious proposal consistent with the conceptualization of personal recovery and which included a dimension closely linked to hope and another closely related to social support, that appear to be essential for recovery (Bjørlykhaug et al., 2022; Hayes et al., 2017; Leamy et al., 2011). In this theoretical proposal, the two items (items 18 and 19) that in the original version made up the “Hopeful/Cares for Self” dimension were integrated into a dimension now called Hope, Confidence, and Purpose and the three items that in the original version made up the “others’ care and help” dimension were distributed between the dimensions now called Unwellness (item 15) and Connection with Others and Social Support (items 12 and 17), respectively. Thus, this new structure included four factors, which we called: Unwellness, Hope, Confidence, and Purpose, Connection with Others and Social Support, and Living Situation. We considered that these names more adequately reflected what the items that made up the dimensions were intended to measure. The Unwellness dimension includes items expressing situations that negatively affect a person’s psychological well-being. The Hope, Confidence, and Purpose dimension presents items that reflect the positive psychological traits that facilitate recovery. The Connection with Others and Social Support dimension comprises the items related to personal relationships and others’ support that helps people to stay well or to recover. Finally, the Living Situation dimension encompasses the items that evaluate the appropriateness of a person’s current home (a basic material condition of existence), which is an enabling condition for recovery. Design The design used in the study was a non-experimental cross-sectional design and the recommendations included in the STROBE checklist for cross-sectional studies were followed. The adaptation of the RPI was carried out in accordance with the Standards for Educational and Psychological Testing (AERA, APA, & NCME, 2014; Hernández et al., 2020) and the guidelines of the International Test Commission (International Test Commission [ITC, 2017]). Participants Participants were recruited through convenience sampling from three different sources: associations for families and individuals with severe mental disorders in the Basque Country (northern Spain), psychiatric services in the same region, and community rehabilitation services in Catalonia (north-eastern Spain). The inclusion criteria were: to be 18 years old or over and diagnosed, according to the criteria of the International Statistical Classification of Diseases and Related Health Problems (ICD-10; WHO, 2016), with one or more of the following disorders for at least two years: schizophrenia (F20), schizotypal disorder (F21), delusional disorder (F22), induced delusional disorder (F24), schizoaffective disorders (F25), other nonorganic psychotic disorders (F28), unspecified nonorganic psychosis (F29), bipolar affective disorders (F31), severe depressive episode with psychotic symptoms (F32.3), or recurrent depressive disorder (F33). Participants also had to be users of mental health services, have a good command of Spanish, and be able to complete the instruments alone or with the help of their key worker. These key workers were psychologists, social workers, and social educators and approximately 7% of the participants needed their support to complete the instruments. The final sample included 266 individuals (47% female) aged between 18 and 83 years (M = 44.71, SD = 13.86). In order to obtain different sources of validity evidence, two sub-samples were used. Sample 1 comprised 89 participants (44.9% female) aged between 19 and 83 years (M = 47.58, SD =12.98). Sample 2 comprised 172 participants (47.7% female) aged between 18 and 79 years (M = 43.29, SD = 14.05). Sample 1 was recruited through associations for families and individuals with severe mental disorders in the Basque Country, as well as among psychiatric patients treated at Hospital Santiago, which is part of the Basque Health Service network and belongs to the University Hospital of Álava. Sample 2 was recruited from a psychiatric hospitalization unit and a users’ and survivors’ organization in Catalonia, Spain. In both cases, all individuals who met the inclusion criteria were invited to participate. A service professional, together with a member of the research team, informed them about the study’s objectives. Participation was voluntary, and no financial compensation was provided. The socio-demographic characteristics of the participants are shown in Table 1. Table 1 Sociodemographic Characteristics of the Samples  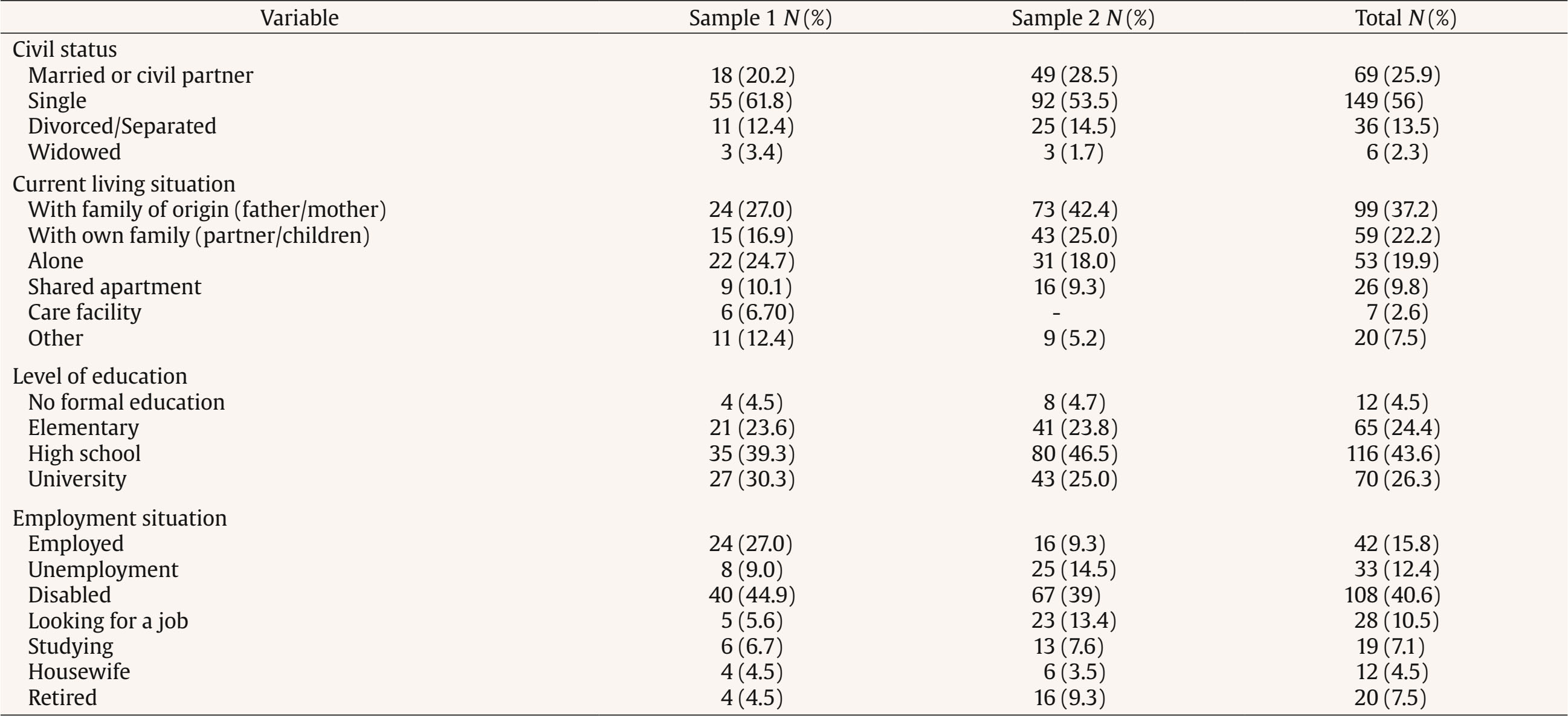 Note. In some variables, the total does not match the sample size due to missing responses. In the Employment Situation variable, the total may exceed the sample size since the categories were not mutually exclusive. Finally, a subsample of sample 2, consisting of 36 participants (36.1% female) aged between 17 and 79 years (M = 46.83, SD = 18.68), was used to analyze temporal stability. The socio-demographic characteristics of this sub-sample are shown in thesupplementary_files_S1. Instruments Spanish version of the RPI (RPI-S) The translation and cultural adaptation of this instrument was developed following the process described in supplementary_files_S2. As a result of this process, we obtained the RPI-S validated in this study. It is a 22-item instrument designed to assess service users’ perceptions of recovery in people with severe mental disorders. Items are rated on a 5-point Likert scale (from 1 = strongly disagree to 5 = strongly agree). Except in 9 items that are reversed, higher scores indicate a higher degree of perceived recovery. The items of the final RPI Spanish version, along with the original English items, are presented in supplementary_files_S3. Spanish version of the 12-item Maryland Assessment of Recovery Scale (MARS-12; Balluerka et al., 2024; Drapalski et al., 2016) The MARS-12 is a unidimensional self-report instrument that assesses recovery from severe mental disorders from the perspective of the service user. Items are rated on a 5-point Likert scale (from 1 = strongly disagree to 5 = strongly agree), so the total score ranges from 12 to 60, with higher scores indicating greater perceived recovery. An example of an item on this scale is “I am hopeful about the future”. The Spanish version has good internal consistency, McDonald’s ω = .97, and good temporal stability, r = .89, as well as high convergent validity (Balluerka et al., 2024). The value of McDonald’s ω in the present sample was .94. Spanish version of the 15-item Questionnaire about the Process of Recovery (QPR-15-SP; Goodman-Casanova et al., 2022; original scale Neil et al., 2009) The QPR-15-SP is a unidimensional self-report instrument that assesses aspects of recovery that are meaningful to people with severe mental disorders. Its items are rated on a 5-point Likert scale (from 0 = strongly disagree to 4 = strongly agree), so the total score ranges from 0 to 60, with higher scores indicating greater perceived recovery. An example of an item on this scale is “I am strongly motivated to get better”. The Spanish version has good internal consistency, McDonald’s ω = .93, and good temporal stability, ICC = .68, as well as high convergent and divergent validity (Goodman-Casanova et al., 2023). In the current sample, the McDonald’s ω value was .95. Spanish version of the Dispositional Hope Scale (DHS; Galiana et al., 2015; original scale Snyder et al., 1991) The DHS is a unidimensional self-report instrument designed to assess an individual’s ability to identify pathways and strategies to achieve their goals, as well as their motivation to pursue these goals. It consists of 12 items, each of which is rated on a 4-point Likert scale (from 1 = definitely false to 4 = definitely true). The total score ranges from 8 to 32, with four items considered as filler and not included in the calculation of the total score. Higher scores on the DHS indicate greater dispositional hope. An example of an item on this scale is “I energetically pursue my goals”. The Spanish version has shown good internal consistency, Cronbach’s α = .83 (Galiana et al., 2015). In the current sample, McDonald’s ω value was .90. Spanish version of the Multidimensional Scale of Perceived Social Support (MSPSS; version adapted by Ruiz Jiménez et al., 2017, in a sample of people with severe mental disorders; original scale Zimet et al., 1990). The MSPSS is a self-report instrument comprising 12 items, each rated on a 7-point Likert scale (from 1 = very strongly disagree to 7 = very strongly agree). These items pertain to three dimensions (4 items per dimension) of perceived support, specifically, support received from friends (e.g., “I can talk about my problems with my friends”), family (e.g., “My family really tries to help me”), and significant others (e.g., “I have a special person who is a real source of comfort to me”). Scores for each dimension range from 4 to 28. The Spanish version has shown good internal consistency, with Cronbach’s alphas ranging from .83 to .94, and good convergent and divergent validity (Ruiz Jiménez et al., 2017). In the current sample, the McDonald’s ω values were .92 for friends, .91 for family, and .87 for significant others, respectively. Questionnaire on socio-demographic variables and mental health diagnosis. It was an ad hoc questionnaire designed to collect data from participants on age, gender, civil status, current living situation, and level of education. Procedure The data were collected between February 2022 and October 2023. All participating service users and their families or legal guardians were informed about the nature and purpose of the study. It was made clear that participation was voluntary and that all data would remain confidential. In all cases the data were collected by a psychologist or a psychiatrist using a paper-and-pencil method. This study was conducted in accordance with the ethical principles of the World Medical Association and the most recent version of the Declaration of Helsinki for research involving human subjects. The study was approved by the Bioethics Committee of the University of Barcelona on 29 November 2021 (CBUB; Institutional Review Board Number: IRB00003099). Responses to all the instruments used were anonymous, and informed consent was obtained from participants after a full explanation of the procedures. In sample 1, participants first completed the questionnaire on socio-demographic variables, followed by the RPI-S, the MARS-12, and the QPR-15-SP. In sample 2, the sociodemographic questionnaire was completed first, followed by the RPI-S, the DHS, and the MSPSS. Finally, the sub-sample of sample 2 completed the RPI a second time, with a one-week interval. Data Analysis In order to obtain validity evidence of the RPI-S measures a number of aspects were analyzed. a) Items. Descriptive statistics (mean, standard deviation, skewness, and kurtosis) of the items were calculated. b) Validity evidence of internal structure. (b1) Dimensionality. In order to examine the internal structure of the RPI-S, three confirmatory factor analysis models were performed. The first tested a unidimensional structure, the second tested the six-factor structure (Anguish; Connected to Others; Confidence and Purpose; Others’ Care/Help, Living Situation; Hopeful/Cares for Self) of the original version of the RPI, and the third one tried to determine whether the RPI-S conformed to a four-factor structure reflecting a more parsimonious proposal consistent with the conceptualization of personal recovery and which included one dimension closely related to hope and another closely related to social support. This structure included four factors: Unwellness; Hope, Confidence, and Purpose; Connection with Others and Social Support; and Living Situation. We used the weighted least squares means and variance adjusted (WLSMV) estimation method, as it is particularly suitable for categorical or ordinal data and provides robust parameter estimates in these cases. Model fit was assessed by calculating the chi-squared statistic, the TLI, the CFI, the RMSEA, and the SMRS goodness-of-fit indices. (b2) Reliability. Internal consistency was assessed through McDonald’s ω coefficient. Temporal stability was estimated by calculating the Pearson correlation coefficient between the scores obtained on each dimension of the Spanish version of the RPI at two time points. c) Validity evidence based on the relationship between the RPI-S measures and other variables. (c1) Convergent validity was assessed by computing the latent correlations between each dimension of the RPI-S and the QPR-15-SP and MARS-12 through structural equation modeling. (c2) Relationship with hope and social support was assessed by computing the latent correlations between each dimension of the RPI-S and the DHS and each dimension of the MSPSS. Data analyses were performed using SPSS 28 and R version 4.2.3 (R Core Team, 2023). The CFAs were performed using the lavaan package (Rosseel, 2012). Given that the percentage of missing values in the dimensions of all instruments ranged between 0% and 3%, pairwise deletion was used for handling such values. Analysis of Items Means, standard deviations, skewness and kurtosis indices for the items of the RPI-S are presented in supplementary_files_S4. Validity Evidence of Internal Structure Dimensionality. As can be seen from the values in Table 2, the unidimensional model showed the worst fit. The original model (Model 2) showed an acceptable fit although the RMSEA and the SMRS values were slightly above the threshold. Finally, the proposed four-factor model (Model 3) showed an adequate fit. Table 2 Results of Confirmatory Factor Analysis for the Three Tested Models  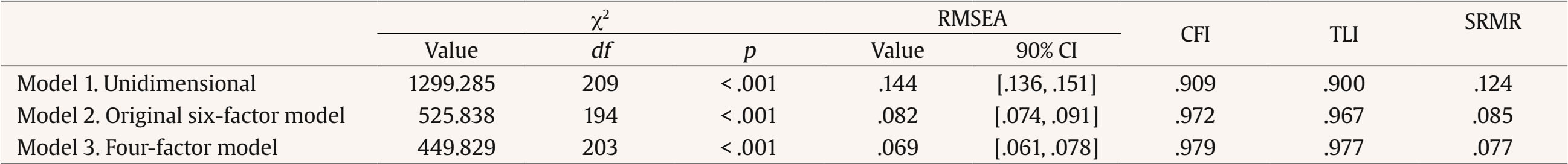 Note. RMSEA = root-mean-square of approximation; CI = confidence interval; CFI = comparative fit index; TLI = Tucker-Lewis Index; SRMR = standardized root mean square residual. Factor loadings were generally adequate in both Models 2 and 3, showing values greater than .45. However, there were 3 items in Model 2 (11, 15, and 20) and 2 in Model 3 (11 and 20) that showed factor loadings below this threshold. In view of the results and considering that Model 3 was more parsimonious, this model was chosen. Furthermore, from a theoretical point of view, the dimensions of Model 3, which included two dimensions closely related to hope and social support, adequately assessed the personal recovery process and could be very useful for users, clinicians, and researchers to assess such process. The standardized factor loadings and between-factor correlations of Model 3 can be seen in Figure 1 (see supplementary_files_S5 for figures of all three models with their corresponding standardized factor loadings and between-factor correlations. Reliability. There was good support for reliability with McDonald’s ω coefficients. Specifically, the values were .79 for Unwellness; .88 for Hope, Confidence and Purpose; .70 for Connection with Others and Social Support; and .74 for Living Situation. In terms of temporal stability, correlation coefficients between component scores over a one-week interval showed adequate values: .73 for Unwellness, .77 for Hope, Confidence and Purpose, .71 for Connection with Others and Social Support, and .75 for Living Situation. Validity Evidence Based on the Relationship between the RPI-S Measures and Other Variables Convergent Validity. As expected, the latent correlations of the RPI-S Unwellness dimension scores with the QPR-15-SP and MARS-12 scores were substantial and negative (r = -.33, r2 = .11 and r = -.35, r2 = .12, respectively), suggesting that 11% and 12% of the variance in these scales is shared with Unwellness. Regarding Living Situation, the correlation values were also substantial but positive (r = .46, r2 = .21 and r = .44, r2 = .19, respectively), indicating that 21% and 19% of the variance in these measures is shared with Living Situation. In the case of Connection with Others and Social Support, both scales showed similar relationships with values of r = .44 and r2 = .19. Finally, Hope, Confidence and Purpose also showed strong positive correlations with QPR-15-SP and MARS-12, with values of r = .68, r2 = .46 and r = .66, r2 = .44, indicating that Hope, Confidence, and Purpose shares 46% and 44% of the variance with these scales. All these correlations indicate that the RPI-S has adequate convergent validity. Relationship with Hope and Social Support Table 3 shows the values of the latent correlations between each dimension of the RPI-S and Dispositional Hope and each dimension of Perceived Social Support. Table 3 Latent correlations of RPI-S dimensions with Dispositional Hope and Perceived Social Support  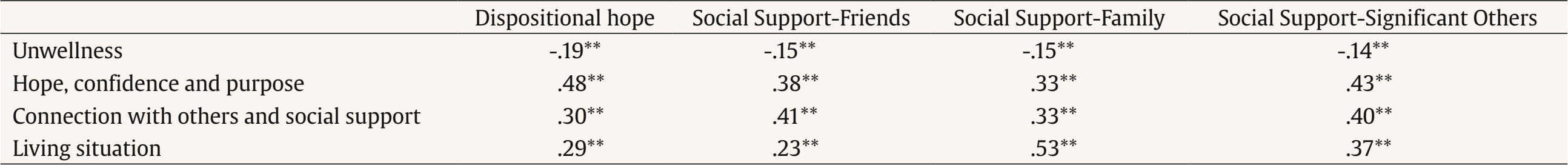 **p < .01. The correlations of Unwellness with Hope and Social Support were negative, although smaller than expected. Regarding Living Situation, the values were positive and moderate, except for Social Support from the Family, where the magnitude was substantial. In the case of Connection with Others and social support, the correlations were moderate and they followed the expected direction for both Hope and Social Support. Finally, regarding Hope, Confidence, and Purpose, the scores showed, as expected, high positive correlations with Hope and moderate correlations with Social Support. The implementation of recovery-oriented mental health interventions requires the development of a solid conceptual framework of recovery and the availability of adequate instruments to evaluate such interventions. In order to respond to these objectives, the present study aims to cross-culturally adapt and validate Spanish version of the Recovery Process Inventory (RPI-S), a short and easy-to-administer instrument that, based on several systematic reviews, shows good psychometric properties. Linked to validity evidence based on the relationship between the RPI-S measures and other variables, we aim to demonstrate the relevance of hope and social support to achieve recovery. The instrument was adapted according to the Standards for Educational and Psychological Testing and the guidelines of the International Test Commission. The results obtained in the translation and cultural adaptation of the instrument were based on the use of an appropriate design for the translation of the items, on the evaluation by experts and on the use of cognitive interviews with the target population, and provided confirmation of semantic, linguistic, and contextual equivalence between the RPI-S and the original instrument, thus providing evidence of content validity. Regarding validity evidence of its internal structure, the RPI-S showed consistency with the four-factor structure proposed in this study. This structure was chosen because it showed a better fit and was more parsimonious than the structure of the original scale. In addition, from a theoretical approach, this structure included two dimensions closely related to hope (Hope, Confidence, and Purpose dimension) and to social support (Connection with Others and Social Support dimension), which are key elements in the conceptual framework of recovery (Bjørlykhaug et al., 2022; Hayes et al., 2017; Leamy et al., 2011). Furthermore, regarding the Unwellness dimension, recovery-oriented care has been defined as a wellness approach (Swarbrick, 2012). This is in line with the current World Health Organization definition of mental health, which is more than the absence of symptoms, and is conceptualized as “a state of well-being in which the individual realizes his or her own abilities and can cope with the normal stresses of life” (WHO, 2021, p. 1). Wellness is therefore highlighted as one of the basic standards that should be used in evaluating recovery-oriented interventions (Davidson et al., 2021). Finally, the Living Situation dimension recognizes that housing is an enabling condition for recovery from a mental health problem (Browne et al., 2008). In this sense, the recognition of the importance of the Living Situation for the recovery process is the basis of the Housing First programmes that have been implemented in different countries around the world (Greenwood et al., 2020). The structure of the RPI-S proposed in this research incorporates these four key dimensions for assessing personal recovery. The reliability coefficients obtained for these four dimensions showed that the RPI-S had good internal consistency and temporal stability. For all these reasons we considered that the four dimensions that make up the internal structure empirically validated in this study could be very useful for users, clinicians, and researchers to assess the personal recovery process. Furthermore, validity evidence based on the relationship between the RPI-S measures and other variables was provided. Specifically, the results showed negative correlations of moderate magnitude of the Unwellness dimension of the RPI-S with the QPR-15-SP and MARS-12 scores, and positive correlations of high magnitude of the other three dimensions of the RPI-S with the QPR-15-SP and MARS-12 scores. These findings can be considered evidence of convergent validity. With regard to the relationship of the RPI-S measures with hope and social support, the results confirmed the central role of hope and social support to achieve recovery. In fact, people with greater hope and social support from family, friends, and significant others, reported better levels of personal recovery in all the aspects assessed by the RPI-S. To the best of our knowledge, this is the first study to provide direct evidence of the importance of hope for the recovery process in the Spanish-speaking population with severe mental disorders. There are recent studies that support this idea, but in an indirect and inverse way. For example, a study developed in Catalonia (Northeastern Spain) found that only people who had participated in spaces of mutual support and activism, that is, who had been given hope by meeting other people who had made or were making a recovery process, believed that they too could recover (Sampietro et al., 2022). On the other hand, although there is an extensive literature on the importance of social support for mental health in the Spanish-speaking population, studies focusing on recovery are less numerous. Among them, there are two recent studies showing positive effects of social support on recovery in people with psychotic symptoms (Guerrero-Jiménez et al., 2022) or adults over 50 years old with a major depressive disorder (Gabarrell-Pascuet et al., 2022). In the same vein, our study shows that there is a high correlation between perceived social support and personal recovery among the Spanish population with severe mental disorders. The main limitation of this study is that participants were recruited through convenience sampling within specific regions of Spain. However, it is important to note that the number of participants was adequate making up a representative sample of service users with severe mental disorders. The results of the validation of the RPI-S suggest that it is a valid and reliable tool for assessing personal recovery among Spanish people with severe mental disorders. The final Spanish version of the RPI, including the instructions and the response options for completing it, can be found in supplementary_files_S6. Furthermore, because it is short and easy to administer, it is a very useful tool for researchers, users, and especially mental health professionals, such as psychiatrists, psychologists, and nurses, who want to adequately assess personal recovery in the Spanish-speaking population. The study has several important strengths. One is that the RPI-S was developed in strict accordance with internationally recognized guidelines for test adaptation. In addition, its psychometric properties have been thoroughly examined in a substantial sample of the target population, namely Spanish adults with severe mental disorders. It also contributes to the conceptualization of the recovery framework by providing additional evidence on the relevance of psychosocial factors, especially hope and social support, as key elements to be promoted in interventions aimed at personal recovery. The availability of this new tool, which is both short and easy to administer, provides mental health professionals with a convenient means of assessing recovery. Indeed, the RPI-S assesses psychosocial aspects that promote or hinder personal recovery. In addition, it facilitates the implementation of evidence-based interventions aimed at promoting recovery, thus contributing positively to the provision of recovery-focused mental health care in Spain. From the perspective of users and families, the instrument may encourage interventions that go beyond the clinical goals that have traditionally focused on symptom control and functionality (Sampietro et al., 2023; Pilgrim, 2008) responding to a long-standing request from organizations representing them. From an international perspective, the RPI-S also provides a platform for further adaptations within the Spanish-speaking world, extending the potential applicability of this tool to populations in over 20 countries.
Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Balluerka, N., Gorostiaga, A., Sampietro, H. M., & Aliri, J. (2025). Spanish adaptation and validation of the Recovery Process Inventory (RPI) in people with mental disorders. Clinical and Health, 36(3), 145-152. https://doi.org/10.5093/clh2025a12 Funding This study was supported by the Spanish Ministry of Science and Innovation (grant PID2019-109887GB-100; ref. MCIN/AEI/10.13039/501100011033), and by the Basque Government (grant IT1493-22). The sources of finding did not participate in the design of the study, the data collection, analysis, or interpretation, the writing of the article, or in the decision to submit it for publication. We thank both institutions for their financial support. References |
Cite this article as: Balluerka, N., Gorostiaga, A., Sampietro, H. M., & Aliri, J. (2025). Spanish Adaptation and Validation of the Recovery Process Inventory (RPI) in People with Mental Disorders. Clinical and Health, 36(3), 145 - 152. https://doi.org/10.5093/clh2025a12
Correspondence: nekane.balluerka@ehu.eus (N. Balluerka).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS







