A Multilevel Model of Compassion in Healthcare Organizations
[Un modelo multinivel de la compasiĂłn en las organizaciones sanitarias]
Mabel San Román-Niaves1, 2, Marco De Angelis2, Susana Llorens1, and Marisa Salanova1
1Universitat Jaume l, CastellĂłn de la Plana, Spain; 2University of Bologna, Bologna, Italy
https://doi.org/10.5093/jwop2024a13
Received 15 October 2024, Accepted 27 November 2024
Abstract
This study investigates compassion’s role in healthcare, examining its relationship between job demands, job social resources, and well-being outcomes (engagement and burnout) across organizational levels. Data from 714 healthcare professionals in 35 Spanish hospital teams were collected using the Brief Compassion Scale and HERO questionnaire. Hierarchical linear modeling showed team-level job social resources positively associated with individual-level compassion (β = .65, p< .01). Compassion positively associated with engagement (β = .88, p< .001) and negatively with burnout (β = -.89, p< .001). Individual-level job demands negatively affected compassion (β = -.60, p< .001). These findings highlight compassion's role in improving engagement and mitigating burnout across organizational levels. The results emphasize the importance of fostering compassion and enhancing team job social resources to improve healthcare professionals’ well-being, offering valuable insights for understanding workforce dynamics in healthcare organizations.
Resumen
Este estudio investiga el papel de la compasión en las organizaciones sanitarias, examinando su relación con las demandas laborales, los recursos sociales del trabajo y los resultados de bienestar (compromiso laboral y agotamiento emocional) desde una perspectiva multinivel. Se recogieron datos de 714 profesionales sanitarios de 35 equipos hospitalarios españoles utilizando la Escala Breve de Compasión y el cuestionario HERO. La modelización lineal jerárquica muestra que los recursos sociales laborales a nivel de equipo se asocian positivamente con la compasión a nivel individual (β = .65, p< .01). La compasión se asocia positivamente con el compromiso (β = .88, p< .001) y negativamente con el agotamiento emocional (β = -.89, p< .001). Las exigencias laborales a nivel individual afectaron negativamente a la compasión (β = -.60, p< .001). Estos resultados ponen de relieve el papel de la compasión en la mejora del compromiso laboral y la disminución del agotamiento emocional en los diferentes niveles de la organización. Los resultados destacan la importancia de fomentar la compasión y mejorar los recursos sociales del trabajo en equipo para mejorar el bienestar de los profesionales sanitarios, ofreciendo claves útiles para comprender la dinámica de la fuerza de trabajo en las organizaciones sanitarias.
Palabras clave
CompasiĂłn, Compromiso laboral, Agotamiento emocional, Organizaciones sanitarias, Estudio multinivelKeywords
Compassion, Engagement, Burnout, Healthcare, Multilevel studyCite this article as: Román-Niaves, M. S., De Angelis, M., Llorens, S., & Salanova, M. (2024). A Multilevel Model of Compassion in Healthcare Organizations. Journal of Work and Organizational Psychology, 40(3), 151 - 163. https://doi.org/10.5093/jwop2024a13
Correspondence: llorgum@uji.es (S. Llorens).In recent years, the concept of compassion has emerged as an important point in organizational research, particularly within the healthcare sector. Compassion, in its essence, involves recognizing suffering in others and oneself, coupled with a genuine motivation to alleviate and prevent that suffering (Gilbert & Choden, 2013). The healthcare sector, known for its high-stress environments and emotional demands, has seen a growing interest in understanding and cultivating compassion (Sinclair et al., 2021). Research indicates that compassion has an important role in improving patient outcomes, enhancing employee well-being, and addressing workplace suffering (McCleland & Vogus, 2021; Trotter, 2021). Healthcare Professionals (HCPs) face significant stressors arising from various sources, including work-life conflicts, irregular working hours, extended shifts, and intense work pressure (Grace & VanHeuvelen, 2019). Additionally, HCPs often experience compassion fatigue due to the emotional demands of patient care (Williams & Lewis, 2020). The healthcare environment also exposes HCPs to various forms of violence, including verbal and physical abuse from colleagues, patients, and patients’ families (World Health Organization & International Labour Organización [WHO & ILO, 2018]). These stressors collectively contribute to high levels of stress and burnout among HCPs, impacting their mental and physical well-being and, consequently, degrading the quality of care they provide. As a result, patient care becomes not only less effective but also less safe (Johnson et al., 2020). To address these challenges, compassion has been identified as a valuable resource for improving social support, resilience, and communication within healthcare teams (San Román-Niaves et al., 2022; Vidman & Strömberg, 2020). Studies show that compassion positively affects mental and physical health and strengthens social relationships (Gilbert, 2020; Neff & Germer, 2013). For example, Jazaieri et al. (2014) found that compassion increases positive emotions, social connectedness, and mindfulness while reducing feelings of isolation and depression. In the context of psychologically healthy workplaces, Salanova et al. (2012) and Salanova et al. (2019) suggested the concept of HEalthy and Resilient Organizations (HEROs). These are defined as “organizations that develop systematic, planned, and proactive efforts to improve their psychosocial and financial health, through healthy practices and resources to improve at the task level, social and organizational environment, especially in crisis situations and sudden changes.” The HERO model suggests that personal and social resources must be deployed in situations of excessive job demands to prevent the deterioration of health, motivation, and performance. Within this model, compassion is categorized as a personal resource, which has been shown to positively affect organizational practices and resources, employee health, and organizational outcomes. Including compassion as a personal resource extends the HERO model, which has previously focused on mental and emotional competencies and beliefs. A recent study in healthcare demonstrated the key role of compassion as a personal resource in improving well-being and healthy organizational outcomes using structural equation modeling analysis (San Román-Niaves et al., 2022). The present study aims to build on this by examining the effect of compassion as a personal resource within a multilevel research design, aligning with the HERO model’s emphasis on the multilevel nature of organizations (individual, group, leader, organization). The compassion’s role in the workplace is further supported by the Job Demands and Resources model (JD-R; Bakker & Demerouti, 2014). This model posits that the presence of job demands and job resources in the work environment significantly impacts employee well-being. High job demands, if not balanced by sufficient job resources, can lead to negative outcomes such as burnout and stress. Conversely, the presence of job resources (e.g., social support, autonomy, communication) can buffer the negative effects of job demands and foster positive outcomes like work engagement and increased job satisfaction. Among personal resources, compassion has been identified as a crucial factor for HCPs (Bramley & Matiti, 2014; Vogus et al., 2021). Personal resources, including compassion, are psychological characteristics associated with resilience and the ability to control and positively impact one’s own environment. These resources help employees achieve their goals and encourage personal and professional development (Schaufeli & Taris, 2014). Moreover, compassion has been shown to be an important factor in mitigating burnout and empathetic distress, while positively impacting the quality of care and patient health (Klimecki & Singer, 2012). These personal resources often cross among group members when there are actual resources and potential resource losses are conceptualized as key sources of stress in individuals’ lives (Hobfoll et al., 2018). Recent research has highlighted the need to identify resources at different organizational levels, calling for actions to reinforce resources at four levels: individual, group, leader, and the organizational level (the IGLO model). This approach aims to promote employee health, well-being, and performance across all levels of the organization (Day & Nielsen, 2017; Nielsen et al., 2017). Despite the growing body of research on compassion in healthcare, there remains a gap in understanding how compassion works as both individual and team-level resource among members of the same team. This study aims to address this gap by exploring the role of compassion through a multilevel analysis. Specifically, it examines the relationship between job demands and social job resources with compassion, and their impact on psychological well-being (burnout and engagement). By adopting this multilevel approach, our study seeks to provide a more comprehensive understanding of the positive effects of compassion on individuals and the organization as a whole. Therefore, this study aims to investigate compassion’s role in healthcare by examining its relationship with job demands, job social resources, and well-being outcomes (engagement and burnout) across organizational levels. This research has important implications for HCPs, organizational leaders, policymakers, and researchers involved in developing strategies to enhance workforce resilience and performance in healthcare settings. Theoretical Framework Job Social Resources, Job Demands, and Compassion HCPs face numerous stressors that can negatively impact their well-being. These stressors include high workloads, complex patient needs, and dealing with traumatic situations (Adriaenssens et al., 2015; Happell et al., 2013). These factors can be considered job demands, defined as “those physical, psychological, social, or organizational aspects of the job that require sustained physical and/or psychological (cognitive and emotional) effort or skills and are therefore associated with certain physiological and/or psychological costs” (Bakker & Demerouti, 2007). Research has shown that such demands can lead to significant health issues, including sleep disturbances, increased sickness absence, and reduced job performance (Åhlin et al., 2021; Andersen et al., 2021; Huhtala et al., 2021; Jimmieson et al., 2017; Lee et al., 2021; Matick et al., 2021). To counterbalance these demands, job social resources play an important role. Job social resources are “those aspects of the job that are functional in achieving work goals, reduce job demands and the associated physiological and psychological costs, and stimulate personal growth, learning, and development” (Bakker & Demerouti, 2007). In healthcare, these resources include supportive work climates, positive leadership, and effective team coordination, which can help HCPs manage demands more effectively (Cruz-Ortiz et al., 2013; Wang et al., 2020). Compassion can buffer the adverse effects of emotional overload and contributes to overall well-being, reducing perceived stress and improving positive well-being indicators (Andersson et al., 2022; Brito-Pons et al., 2018; Kinman & Grant, 2020; Sinclair et al., 2021). However, the interplay between job demands, job social resources, and compassion is complex. While compassion can serve as a protective factor, excessive demands for compassion can paradoxically increase the risk of burnout and compassion fatigue (Buonomo et al., 2022). This complexity highlights the need to examine these relationships from a multilevel perspective, considering both individual and team-level factors. The JD-R model provides a framework for understanding these dynamics within healthcare settings. According to this model, job social resources can mitigate the negative impact of job demands on individual well-being by providing the support and resources necessary to cope with high demands. Compassion, as a personal resource, can further enhance this coping mechanism, potentially leading to improved psychological well-being and reduced stress. Given the established effects of these factors and the complex interactions between them, this study aims to explore the dynamics between job demands, job social resources, and compassion within healthcare settings. Based on the theoretical framework and existing literature, we propose the following hypotheses: Hypothesis 1 (H1): Group-level job social resources (Level 2) have a direct positive relationship with individual-level compassion, after controlling for individual-level job demands (Level 1). Hypothesis 2 (H2): Group-level job social resources (Level 2) moderate the relationship between individual-level job demands and compassion (Level 1). Figure 1 illustrates the proposed research model, highlighting the relationships and specific hypotheses tested for H1 and H2. The model shows the direct positive relationship between job social resources and compassion (H1) and the moderating effect of job social resources on the relationship between job demands and compassion (H2). Figure 1 Research Model Involving the Relationship between Individual (job demands and compassion) and Group/Team-level (job social resources) Variables.  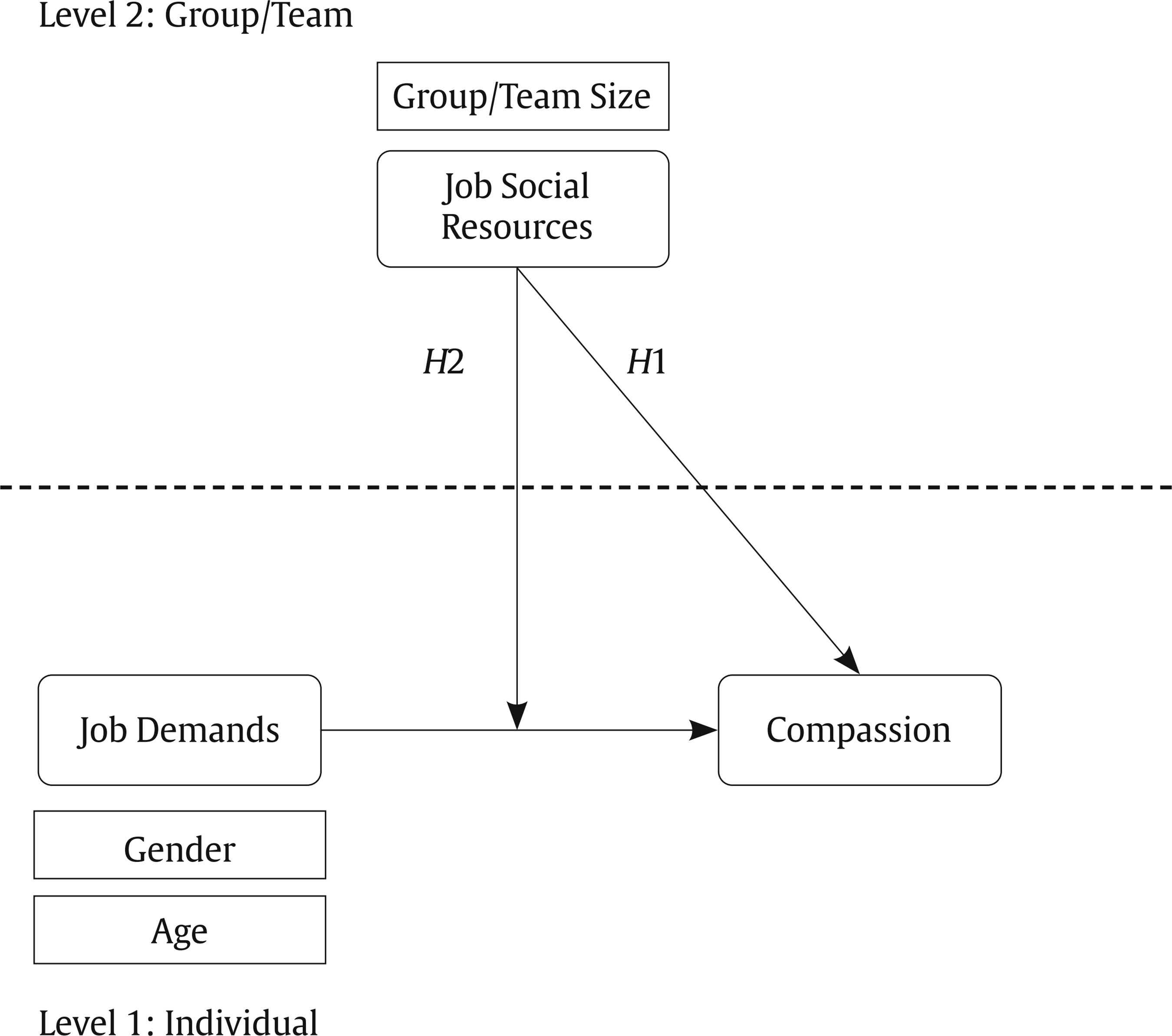 Job Social Resources, Compassion, Engagement and Burnout In the field of organizational psychology, employee well-being is often examined through two distinct but related concepts: work engagement and burnout. These concepts are particularly relevant in healthcare settings, where professionals face high levels of stress and emotional demands. Within the broader field of organizational psychology, two distinct perspectives on employee well-being have emerged. The first perspective highlights the positive aspects of well-being, focusing on work engagement, which is characterized by a high level of energy, dedication, and absorption in work activities (Schaufeli, 2015). Research indicates that improving work engagement is essential for enhancing employee well-being, job satisfaction, and other beneficial workplace outcomes, including productivity and life satisfaction (Demerouti & Bakker, 2022). Alternatively, the opposing perspective centers on the negative aspects, specifically burnout. Burnout refers to a state of emotional exhaustion, depersonalization, and a decrease in personal fulfilment at work, which is prevalent among healthcare professionals due to their chronic exposure to high work stress (Maslach & Jackson, 1981; Romani & Ashkar, 2014). Both engagement and burnout are considered opposites on a continuum, with “activation” and “identification” as the opposing poles (Schaufeli et al., 2008). At the activation pole, elements as fatigue and emotional exhaustion from burnout contrast with vigor from engagement. The identification pole comprises cynicism (associated with burnout) and dedication (associated with engagement; Llorens et al., 2022). This relationship suggests that high levels of engagement can protect against the development of burnout, while a decrease in engagement may increase the risk of burnout (Bakker & Demerouti, 2007, 2014). Building on this understanding, this study explores the role of compassion and job social resources as potential moderators in the dynamics between job demands, engagement and burnout. Compassion, as personal resource, along with job social resources, may improve how HCPs perceive and cope with their job demands, serving as a mechanism that potentially leads to optimal work engagement and reduced burnout levels. Job Social Resources, Compassion, and Engagement The relationship between social resources and engagement is an important aspect for work psychology. Job social resources, such as social support and positive interpersonal relationships, have been consistently shown to enhance work engagement and alleviate job stress (Bakker & Demerouti, 2007; Nappo, 2020; Nasurdin et al., 2018). Compassion, as a personal resource, also plays an important role in this dynamic. It fosters a sense of belonging and meaning within the work environment (Dutton et al., 2014), enriching engagement and improving workplace outcomes (Buonomo et al., 2022; Simpson et al., 2020; Sinclair et al., 2021). HCPs who exhibit compassion often report better patient satisfaction, more effective interaction with patients, and improved patient outcomes (Baguley et al., 2022). However, the relationship between compassion and engagement is complex. In highly stressful environments, the demands of compassion can sometimes outweigh its benefits (Mauno et al., 2016). This suggests that the impact of compassion on engagement is influenced by contextual factors such as workload, support systems, and personal resilience. Figure 2 Research Model Involving the Relationship between Individual (compassion and engagement) and Group/Team-level (job social resources) Variables.  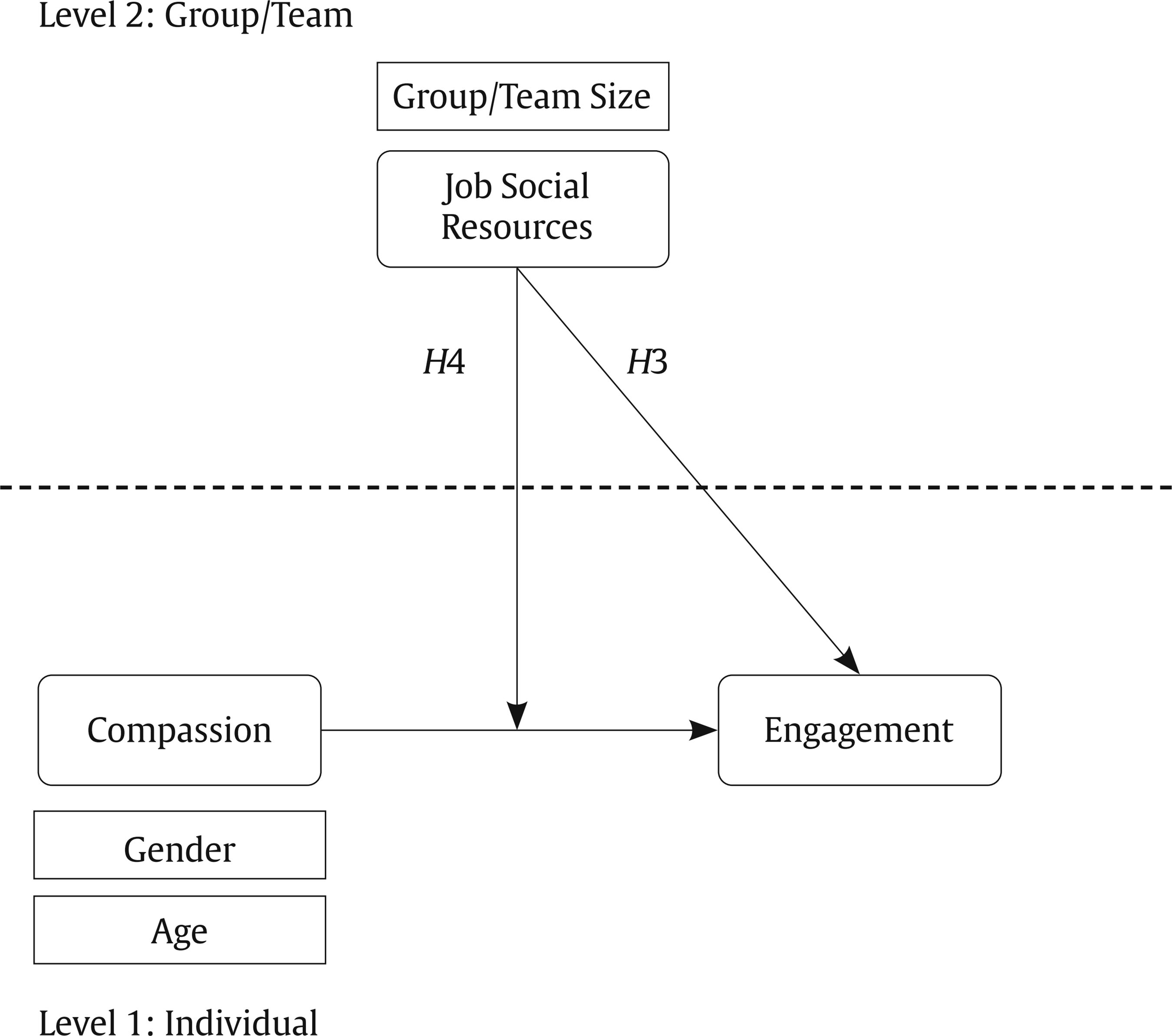 Furthermore, compassion is linked to higher levels of work engagement, especially when employees face challenging tasks (Deao et al., 2017; García-Sierra et al., 2016). This engagement is often mediated by the supportive nature of work environment, which provides meaning, reduces stress, and protects against emotional exhaustion. The JD-R model provides a framework for understanding these dynamics. It posits that job social resources can enhance personal resources like compassion, leading to increased work engagement. Based on this theoretical foundation, we propose the following hypotheses: Hypothesis 3 (H3): Group-level job social resources (Level 2) have a direct positive relationship with individual-level work engagement, after controlling for individual-level compassion (Level 1). Hypothesis 4 (H4): Group-level job social resources (Level 2) moderate the relationship between individual-level compassion work and engagement (Level 1). Figure 2 illustrated the proposed research model, highlighting the relationships and specific hypotheses tested for H3 and H4. The model shows the direct positive relationship between job social resources and engagement (H3) and the moderating effect of job social resources on the relationship between compassion and engagement (H4). Job Social Resources, Compassion and Burnout Burnout is a significant concern in occupational health, particularly among HCPs, it is characterized as a detrimental state of well-being and the negative counterpart of work engagement (Schaufeli et al., 2006). HCPs often face long working hours, emotional burdens of patient care, and inadequate workplace support (West et al., 2016). The consequences of burnout extend beyond individual well-being, as it is associated with reduced quality of patient care and increased medical errors (Mangory et al., 2021). Studies indicate that job social resources have an important role in mitigating burnout. HCPs with access to such resources report lower levels of burnout and higher levels of job satisfaction (Bernales-Turpo et al., 2022; Szwamel et al., 2022). A supportive work environment with sufficient job social resources helps HCPs better manage their job demands, reducing burnout risks and fostering a compassionate approach to patient care (Abraham et al., 2021; Khammissa et al., 2022; Mayra et al., 2023). Compassion, while generally considered a protective factor against burnout, presents a complex relationship with burnout in healthcare settings. Paradoxically, when excessively demanded, compassion can increase the risk of burnout and compassion fatigue (Buonomo et al., 2022; Thapa et al., 2021). This highlights the double-edged nature of compassion in healthcare: it is essential for quality care but can be potentially exhausting when not properly supported. To address these challenges, strengthening job social resources, such as social support from colleagues and supervisors, is crucial. These resources can help HCPs maintain emotional balance amid stressful work conditions, safeguarding their mental health and overall well-being (Blanco-Donoso et al., 2020; Chew et al., 2020; Nowicki et al., 2020). Given this complex interplay, our study seeks to explore how job social resources and compassion together influence burnout levels among HCPs. The JD-R model supports the notion that job social resources can mitigate the negative effects of job demands on burnout, while personal resources like compassion further buffer against burnout, promoting psychological well-being. Based on this theoretical framework, we hypothesize: Hypothesis 5 (H5): Group-level job social resources (Level 2) have a direct negative relationship with individual-level burnout, after controlling for individual-level compassion (Level 1). Hypothesis 6 (H6): Group-level job social resources (Level 2) moderate the relationship between individual-level compassion and burnout (Level 1). Figure 3 illustrates the proposed research model, highlighting the relationships and specific hypotheses tested for H5 and H6. The model shows the direct negative relationship between job social resources and burnout (H5) and the moderating effect of job social resources on the relationship between compassion and burnout (H6). Figure 3 Research Model Involving the Relationship between Individual (compassion and burnout) and Group/Team-level (job social resources) Variables.  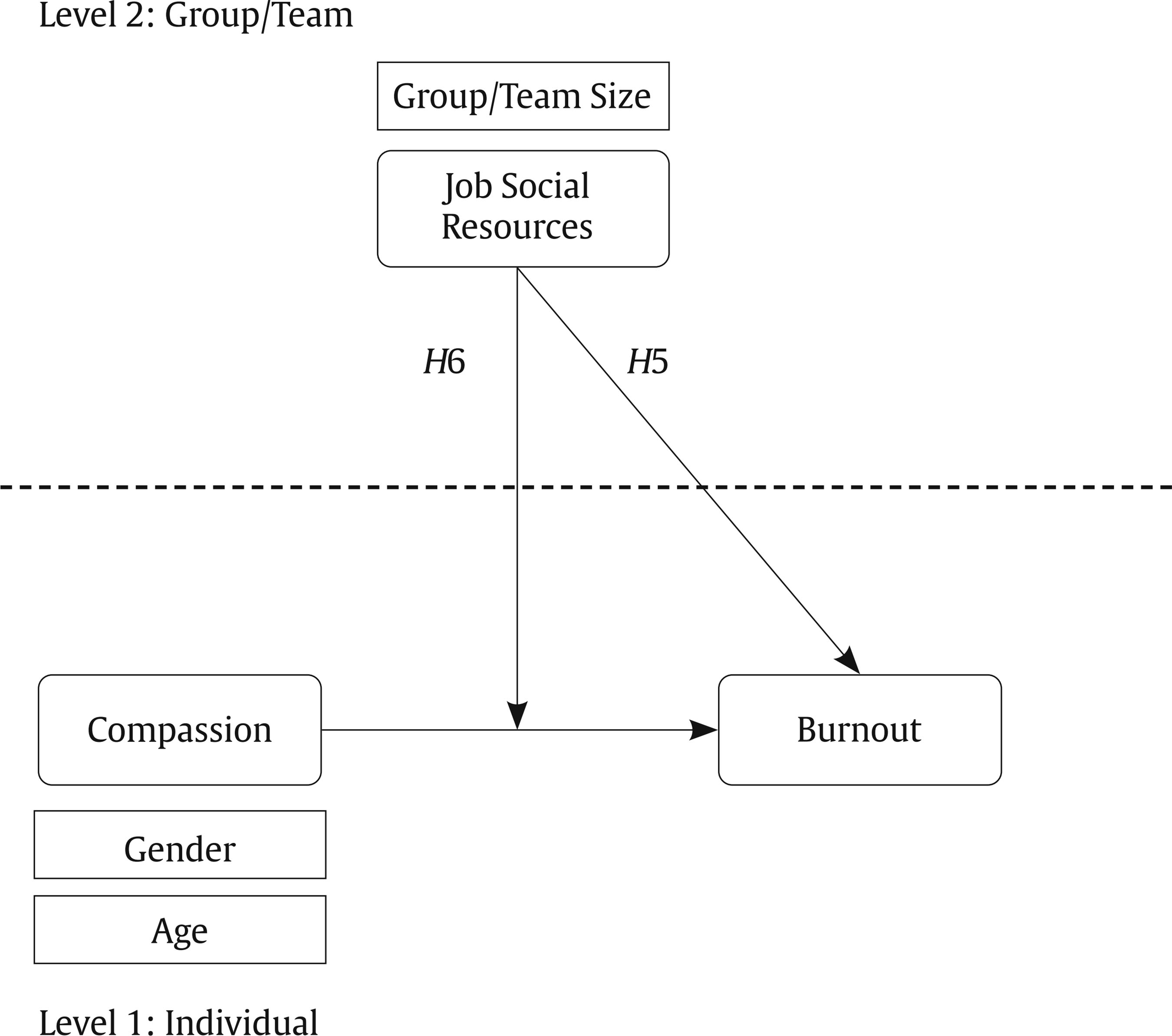 Data Collection The sample consisted of 714 HCPs (81.2% female and 18.8% male) nested within 35 services/care units (ranging from 5 to 81 members) from 30 public and private hospitals in Spain. The mean age was 43.2 (SD = 10.7) and the average tenure time was 12.9 years (SD = 10.2). The selection process for the hospitals and their respective services/care units involved two main parts. Initially, an invitation was extended through a non-profit organization that conducts an annual national contest aimed at recognizing high levels of psychosocial well-being within healthcare settings. This contest was widely advertised on the organization’s website and through social media platforms, encouraging participation from across Spain. Hospitals interested in demonstrating their commitment to psychosocial well-being registered for the contest, adhering to the stipulated rules and obtaining necessary approvals from their administration. From these registrations, 35 services/care units from 30 public and private hospitals, both small regional and large metropolitan, opted to participate, ensuring that they met the contest’s requirement of having at least 5 members per unit. The hospitals that enrolled did so voluntarily, seeking recognition for their efforts in enhancing workplace well-being, which means the selection was based on self-selection criteria rather than random sampling. This method resulted in a convenience sample that, while not randomly chosen, is representative of motivated and engaged healthcare institutions across various types of settings in Spain, reflecting a diverse cross-section of the nation’s hospital systems committed to improving employee psychosocial health. Following the registration deadline, data were collected using the Healthy and Resilient Organizations (HERO) Questionnaire (Salanova et al., 2012; Salanova et al., 2019), which included 5 items of the Brief Compassion Scale (Amutio et al., 2018; Pommier et al., 2020). The questionnaire was distributed via an email containing a Qualtrics online link with all necessary instructions. Participation was voluntary and no incentives were offered. Informed consent was obtained from each participant, who agreed that the data would be used exclusively for research purposes and ensured confidentiality. To ensure confidentiality and anonymity, all responses were collected through Qualtrics in a manner that did not record any personally identifiable information. Additionally, all data were encrypted and stored on secure servers with access restricted to the research team only. The study was conducted in accordance with GDPR regulations (EU 2016/679) on data protection and with the approval of the Jaume l University Ethics Committee (CD/57/2020). Each participant provided informed consent. Measures Measures at Individual Level Compassion. It was assessed using the Brief Compassion Scale (Amutio et al., 2018; Pommier et al., 2020). This scale consists of five items distributed across four dimensions: self-kindness (two items), common humanity (one item), mindfulness (one item), and non-judgement/forgiveness (one item). The selection of these scale is grounded in Pommier et al., (2020), emphasizing the recognition and alleviation of suffering. The specific items are as follows: (1) Self-kindness: “If I see that someone is having difficulties, I try to help”; (2) Common humanity: “I think everyone feel sad sometimes; it is part of being human”; (3) Mindfulness: “I usually listen patiently when people tell me about their problems”; (4) Non-judgement/forgiveness: “I try not to judge other when they make mistakes or are wrong.” The items are scored on a seven-point frequency rating scale from 0 (never) to 7 (always). Cronbach’s alpha (α = .62) and McDonald’s omega (ω = .61) indicate a moderate level of internal consistency. Job Demands. They were assessed using the HERO questionnaire sub-scale by the same name including quantitative overload, qualitative overload, mental overload, emotional overload, role ambiguity, role conflict, routine, mobbing, and emotional dissonance. Each element is represented by a single item, where each of these single items is the mean of the HERO sub-scale (Salanova et al., 2012; Salanova et al., 2019). Each item represents an aspect of the job demands theoretically linked to the HERO model, which integrates comprehensive elements of job demands and resources that impact employee health and organizational outcomes. Sample items for each domain include: (1) Quantitative overload: “Degree to which you are overwhelmed by the amount of work you have to do, either due to lack of time or overloaded with tasks”; (2) Mental overload: “Degree to which work requires a lot of concentration, precision, you have to be aware of different things at the same time and remember them”; (3) Emotional overload: “Degree to which the work requires you to be emotionally involved, either because you have to deal with clients (patients, relatives, accompaniers), or because you have to persuade or convince others”; (4) Role ambiguity: “Degree to which you do not clearly perceive the role and tasks you have to perform in your job. You are not sure about what you have to do, how you have to do it and why you have to do it”; (5) Role conflict: “Degree to which you perceive demands or receive orders that are incompatible and contradictory to each other. That is, in order to do one task, you have to stop doing another”; (6) Routine: “Degree to which the tasks you perform are not innovative, unchallenging, repetitive and unchanging. Moreover, they do not involve the use of different skills”; (7) Mobbing: “Degree to which you are subjected to hostile and unethical communication on a systematic basis, resulting in a position of vulnerability”; and (8) Emotional dissonance: “Degree to which you have to express emotions that you don’t really feel, or you have to suppress the expression of emotions that you really feel”. The items are scored on a seven-point frequency rating scale from 0 (never) to 7 (always). Cronbach’s alpha (α = .81) and McDonald’s omega (ω = .80) indicate a high level of internal consistency. Engagement. It was assessed by the one item included in the HERO questionnaire adapted from the Utrech Work Engagement Scale (UWES; Schaufeli et al., 2006). The item includes “Degree to which you feel immersed, full of energy, dedicated to your work, creating a positive climate of fulfilment and enthusiasm.” The selection of this item is based on the characteristics of engagement: vigor, dedication, and absorption. These dimensions capture the positive, fulfilling work-related state of mind that is important for employee motivation and productivity (Schaufeli et al., 2006). The participants answered using a seven-point frequency type scale with scores from 0 (never) to 7 (always). Burnout. It was assessed by the one item included in the HERO questionnaire adapted from Maslach Burnout Inventory (Maslach et al., 1997). The item includes “Degree to which you feel ineffective in your work, uninterested, uninvolved, physically and emotionally exhausted. In addition, you feel insensitive to the people around you (e.g., users: patients, relatives, companions, colleagues).” This item was selected based in the conceptualization of burnout, which included the three dimensions: emotional exhaustion, depersonalization, and personal accomplishment. These dimensions reflect the core aspects that significantly impact employee well-being and performance (Maslach et al., 1997). The participants answered using a seven-point frequency type scale with scores from 0 (never) to 7 (always). Measures at Group/Team Level Job Social Resources. They were assessed using the HERO questionnaire sub-scale by the same name, which includes social support climate, positive leadership, and coordination. Each of these elements is represented by a single item, with the mean of these items comprising the HERO sub-scale. The items were choose based on the HERO model, which emphasizes the importance of social resources in promoting healthy employees (Salanova et al., 2012; Salanova et al., 2019) Sample items for each domain include: (1) Positive leadership: “Degree to which your supervisor considers the needs of your service/care unit, recognizing the effort and achievement of goals of the service/care unit”; (2) Social support climate: “Degree to which you feel support from your colleagues and supervisor in your personal and professional circumstances”; (3) Coordination: “Degree to which you are coordinated with your work team, to respond to work situations.” The items are scored on a seven-point frequency rating scale from 0 (never) to 7 (always). Cronbach’s alpha (α = .80) and McDonald’s omega (ω = .81) indicate a high level of internal consistency. Control Variables. included group/team size (the total number of members per group/team) at the group/team level. Gender and age were included as demographic variables at individual level. Analytical Strategy In this study, the questionnaire measures four individual-level variables and one group/team-level variable included in the HERO questionnaire (Salanova et al., 2012; Salanova et al., 2019). Using the service/care unit as a reference, HCPs assessed job social resources at the group/team level with questions regarding their service/care unit. Meanwhile, compassion, job demands, burnout, and engagement were assessed at the individual level with the respondents themselves as the referents. To assess the reliability and validity of the constructs several indicators were used. Cronbach’s alpha and McDonald’s omega are both internal consistency coefficients to assess the reliability of scales. Cronbach’s alpha measures the interrelatedness of items in a test, with values ranging from 0 to 1, where higher values indicate greater consistency (Cronbach, 1951). McDonald’s omega is considered a better estimator when assumptions for Cronbach’s alpha, such as tau equivalence, are violated (Dunn et al., 2013). These coefficients are important as they provide insights into the internal consistency and reliability of measurement instruments, ensuring the robustness and validity of research findings. To further assess the constructs’ reliability and both discriminant and convergent validity, we calculated Composite Reliability (CR), Average Variance Extracted (AVE), and Maximum Shared Variance (MSV). CR measures the internal consistency of the items that form each construct. AVE indicates the average amount of variance a construct explains in relation to the variance due to measurement error. MSV represents the highest shared variance between constructs, serving as a key metric for assessing discriminant validity. The analysis adhered to established cutoff points for these indicators as proposed by Hair et al. (2010). The variables of engagement and burnout were not included in the reliability and validity analyses because they are single-item variables, which limits their capacity to measure internal consistency and discriminant validity. Interrater reliability and agreement indices were calculated (LeBreton & Senter, 2008). HCPs agreement was assessed using Interclass Correlation Coefficient (ICC1), calculated by dividing the variance between groups by the total variance (sum of the variance within groups and between groups). Even though there is no fixed threshold for ICC1, a value of .01 can be considered a small effect, .10 a moderate effect, and values greater than .25 a large effect (LeBreton & Senter, 2008). Analyses of Variance (ANOVA) were conducted to determine significant group discrimination on variables at both group/team and individual levels. For ICC1, all the variables had small to moderate effects, and ANOVA analyses revealed significant variable differentiation across groups and individuals (from .04 to .16; see Table 1). Results showed group/team level agreement regarding HCPs’ perceptions of job social resources. Aggregation indices also demonstrated sufficient agreement for compassion, engagement, job demands, and burnout at the individual level. Table 1 Means, standard deviations, aggregation indices, and intercorrelations among the study variables at the individual level and group/team level (n = 714 HCPs, n = 35 services).  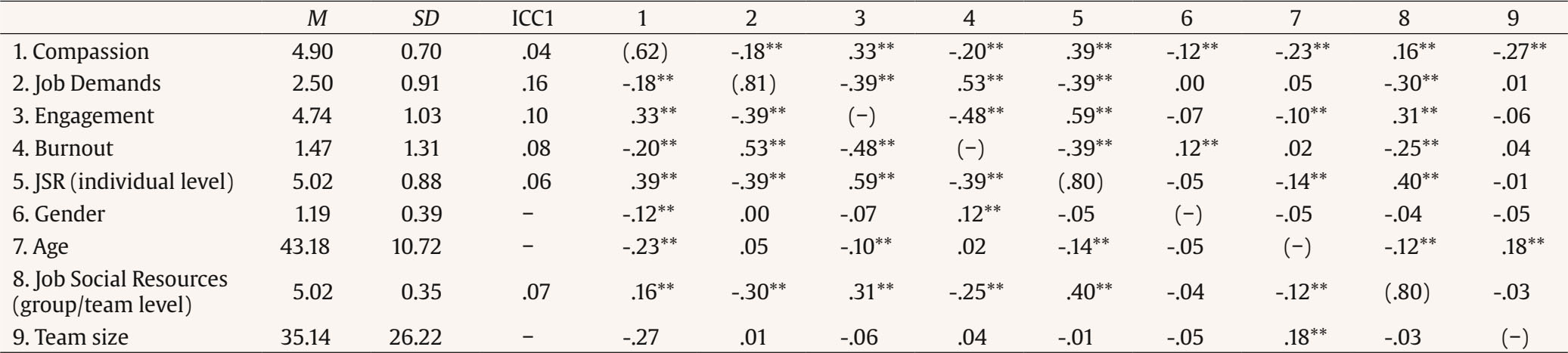 Note. M = Mean, SD = Standard Deviation, ICC1 = Interclass Correlation Coefficient, JSR = Job Social Resources, HCPs = Health Care Professionals, ** p < 0.01. Cronbach’s Alphas are in the main diagonal. Intercorrelations are presented are presented (below the diagonal) and the service/care unit level (above the diagonal). Finally, descriptive and intercorrelations among scales were calculated based on data aggregated at both individual level and group/team level. Data Analyses To examine potential bias due to common method variance, we employed Harman’s single factor test (Podsakoff et al., 2003). This test was conducted on the individual study variables to determine if a single factor could account for most of the variance in the data. Additionally, we utilized the Common Method Factor (CMF) technique, also suggested by Podsakoff et al. (2003), to further control for common method variance. This approach involves adding a latent CMF to the measurement model to capture any common variance among the observed variables. Hypotheses 1-6 were tested by means of hierarchical linear modelling (HLM) and random coefficient modelling (González-Romá & Hernández, 2017; Hox, 2010). HLM is appropriate for data with a nested structure, such as our dataset, which involves individuals nested within teams. Random coefficient modelling, a specific type of HLM, was used to account for random effects at both the individual and group/team levels. The percentage of variance explained by contextual variables is tested using the ICC, a non-independence indicator (Bliese, 2000). A higher the ICC indicates greater variability in the dependent variable explained by a higher-level (i.e., group/team level). A baseline ANOVA model was performed to evaluate non-independence ICC and variance percentages for the levels involved (Hox, 2010). Six additional models were performed using SPSS 28.0’s step-by-step maximum likelihood methodology (Heck et al., 2013; Hox et al., 2017). Models 1, 3, and 5 are random coefficients regression models including group/team level variables and individual level controls (age and gender). Model 1 predicts compassion based on job demands (see Figure 1). Model 3 predicts engagement based on compassion (see Figure 2). Model 5 predicts burnout based on compassion (see Figure 3). Models 2, 4, and 6 are intercepts-as-outcomes models adding cross-level interaction of job social resources. Model 2 examines the interaction effect on the relationship between job demands and compassion (see Figure 1). Model 4 examines the interaction effect on the relationship between compassion and engagement (see Figure 2). Model 6 examines the interaction effect on the relationship between compassion and burnout (see Figure 3). Individual predictors were grand-mean centered, and their intercepts and slopes were allowed to vary between groups/teams. The variance in the intercept term under grand-mean centering adjusts for between-groups variance considering individual predictors (Hofmann et al., 2000). Descriptive Analyses Means, standard deviations, Cronbach’s alphas, McDonald’s omegas among the variables at individual and group/team level are shown in Table 1. Most of the study variables were positively and significantly correlated, instead of the group/team size variable, which is only positively and significantly correlated with age. Also, gender has no correlation with job demands, engagement and with individual and group/team job social resources. Age has no correlation with job demands, burnout, gender, and has a negatively and significantly correlated with group/team level job social resources. To mitigate common method variance bias, following the guidelines of Podsakoff et al. (2003), the questionnaire was designed with distinct sections and different instructions. The results of Harman’s single factor test indicated a poor data fit, with χ2(27) = 193.349, p = .000, RMSEA = .093, CFI = .852, NFI = .835, TLI = .753, and IFI = .854. Additionally, the CMF analysis showed a good model fit, χ2 (85) = 199.270, RMSEA = .044, CFI = .969, TLI = .957, IFI = .969, and SRMR = .031. These results confirm that common method bias does not significantly affect the relationships between the latent variables. Consequently, common method variance is not a serious problem in this study. Lastly, the CR, AVE, and MSV of the constructs were evaluated, and the results are summarized in Table 2. Table 2 Composite Reliability (CR), Average Variance Extracted (AVE), and Maximum Shared Variance (MSV) of the Study Constructs  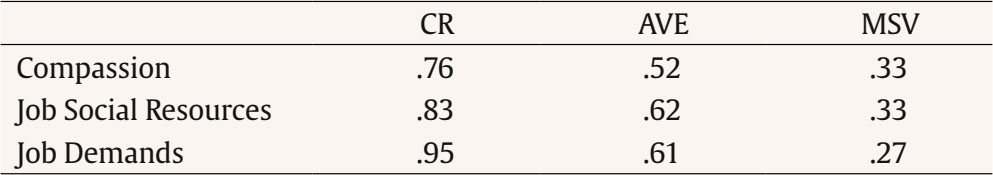 Note. CR = Composite Reliability; AVE = Average Variance Extracted; MSV = Maximum Shared Variance. The results presented in Table 2 emphasize the CR for all constructs, demonstrating strong internal consistency across the scales. AVE values, ranging from .52 to .62, confirm that the constructs meet the criteria for acceptable convergent validity. The constructs of Compassion, Job Social Resources, and Job Demands, with their respective CR values, underscore robust reliability. When comparing their AVEs to the MSV (.52 vs. .33 for compassion, .62 vs. .33 for Job Social Resources, and .61 vs. 0.27 for Job Demands), it is evident that there is good discriminant validity. This indicates that the constructs share a significant degree of variance, suggesting they are related yet sufficiently distinct to maintain conceptual clarity. Therefore, the constructs are both valid and reliable, ensuring the robustness of the measurement model. Hypothesis Testing Table 3 presents the results for the hierarchical linear models predicting compassion, according to Hypothesis 1. Model 1 included group/team level variables to test the cross-level effects, that is, aggregated job social resources, along with control variables (group/team size) and at the individual level variables of job demands and compassion, along with the control variables (age and gender). Results for Model 1 demonstrate that aggregated job social resources are positively and significantly related to compassion (β = .24, p = .07), once the negative (individual-level) relationship between job demands and compassion has been controlled for (β = -.12, p = .001). Therefore, Hypothesis 1 was confirmed. This model investigated how job social resources can moderate the negative impact of job demands on compassion, suggesting that supporting work environments can buffer the adverse effects of high job demands. Table 3 Results of the hierarchical linear models predicting compassion (ICC = 4%).  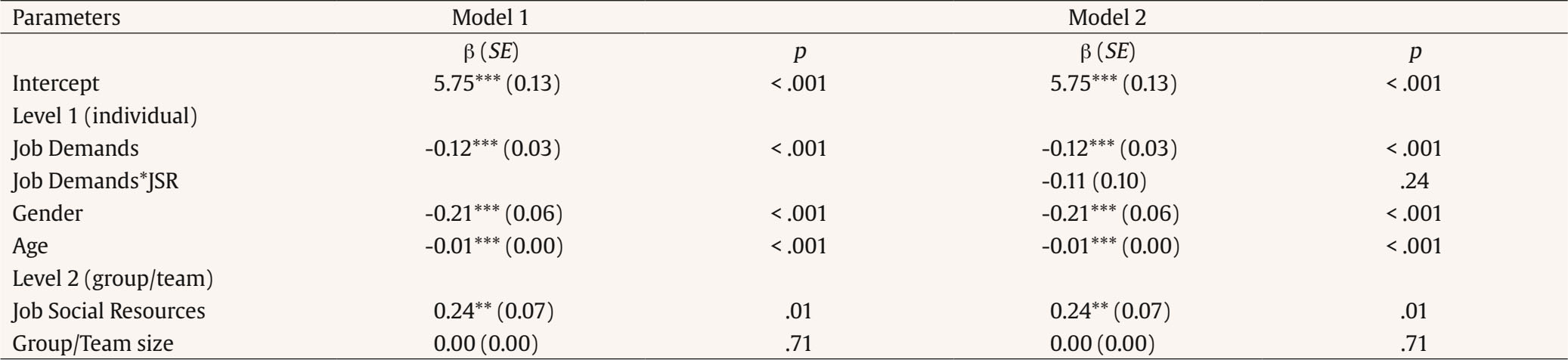 Note. ICC = Intraclass Correlation Coefficient; JSR = Job Social Resources; β = beta, SE = standard errors. **p < .01, ***p < .001. To test Hypothesis 2, Model 2 incorporated the variables of Model 1 while adding the cross-level interaction between team-job social resources and individual-level job demands in predicting compassion. Results revealed no significant cross-level interaction (β = -.11, p = .24), thus failing to support Hypothesis 2 (see Figure 4). Figure 4 Final Model Including the Results of the Cross-level Effects and the Cross-level Interaction for Job Social Resources, Job Demands and Compassion.  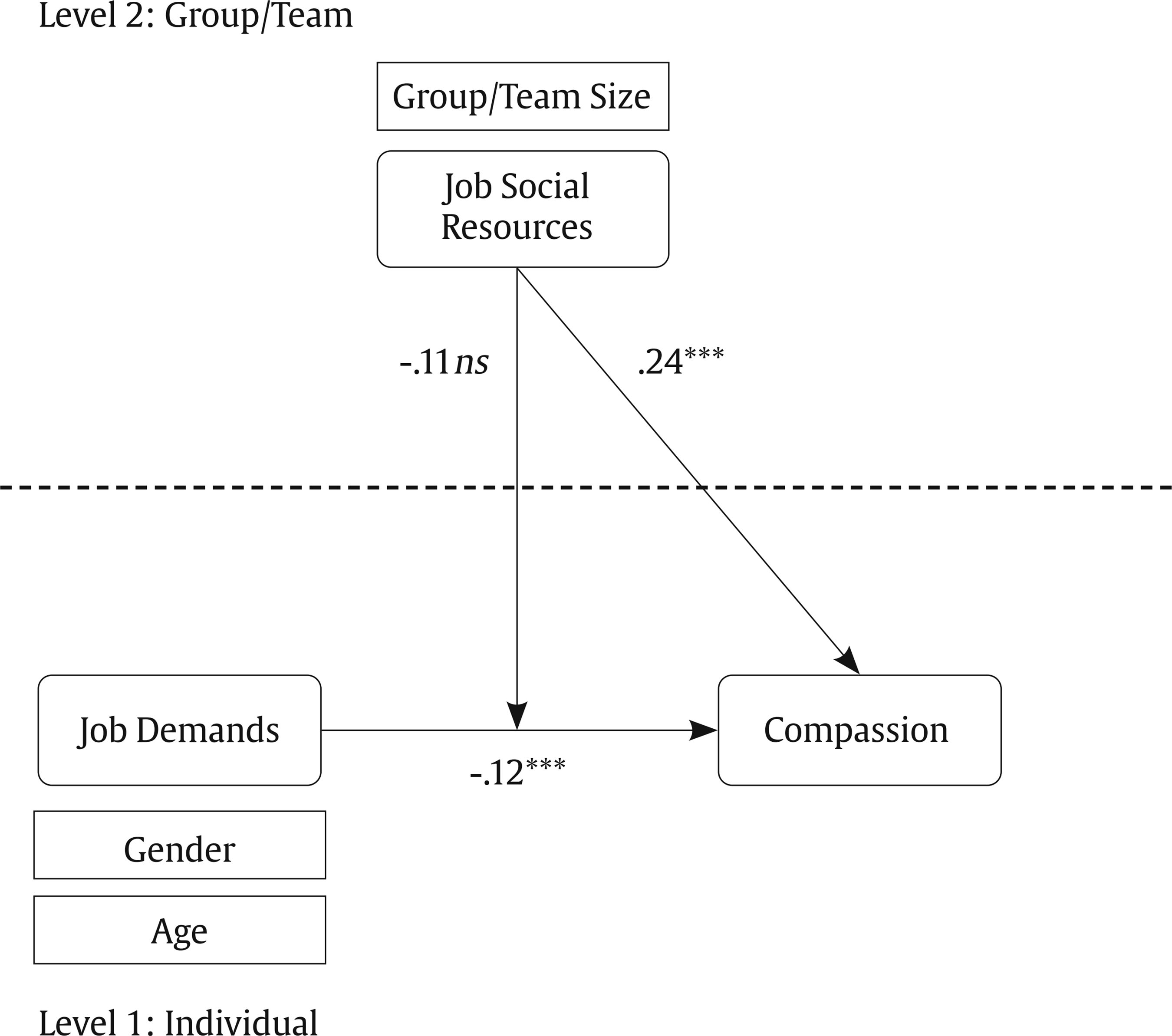 ***p < .001. Table 4 presents the hierarchical linear models predicting engagement, according to Hypothesis 3. Model 3 incorporated both team-level variables to test the cross-level effects, that is, aggregated job social resources, along with control variables (group/team size) and at the individual level variables of compassion and engagement, along with the control variables (age and gender). Results for Model 3 demonstrated that aggregated job social resources are positively and significantly related to engagement (β = .88, p = .001), once the negative (individual-level) relationship between compassion and engagement has been controlled for (β = .41, p = .001). Therefore, Hypothesis 3 was confirmed. This model examined how job social resources can improve the positive effects of compassion on engagement, suggesting also the importance of a supportive work environment. Table 4 Results of the hierarchical linear models predicting engagement (ICC = 10%).  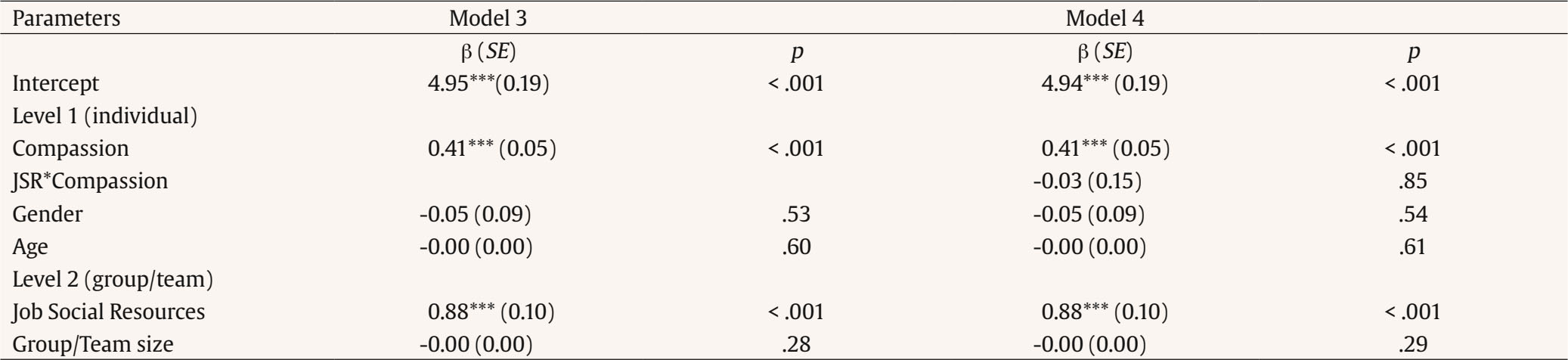 Note. ICC = Intraclass Correlation Coefficient; JSR = Job Social Resources; β = beta, SE = standard errors. **p < .01, ***p < .001. Figure 5 Final Model Including the Results of the Cross-level Effects and the Cross-level Interaction for Job Social Resources, Compassion, and Engagement.  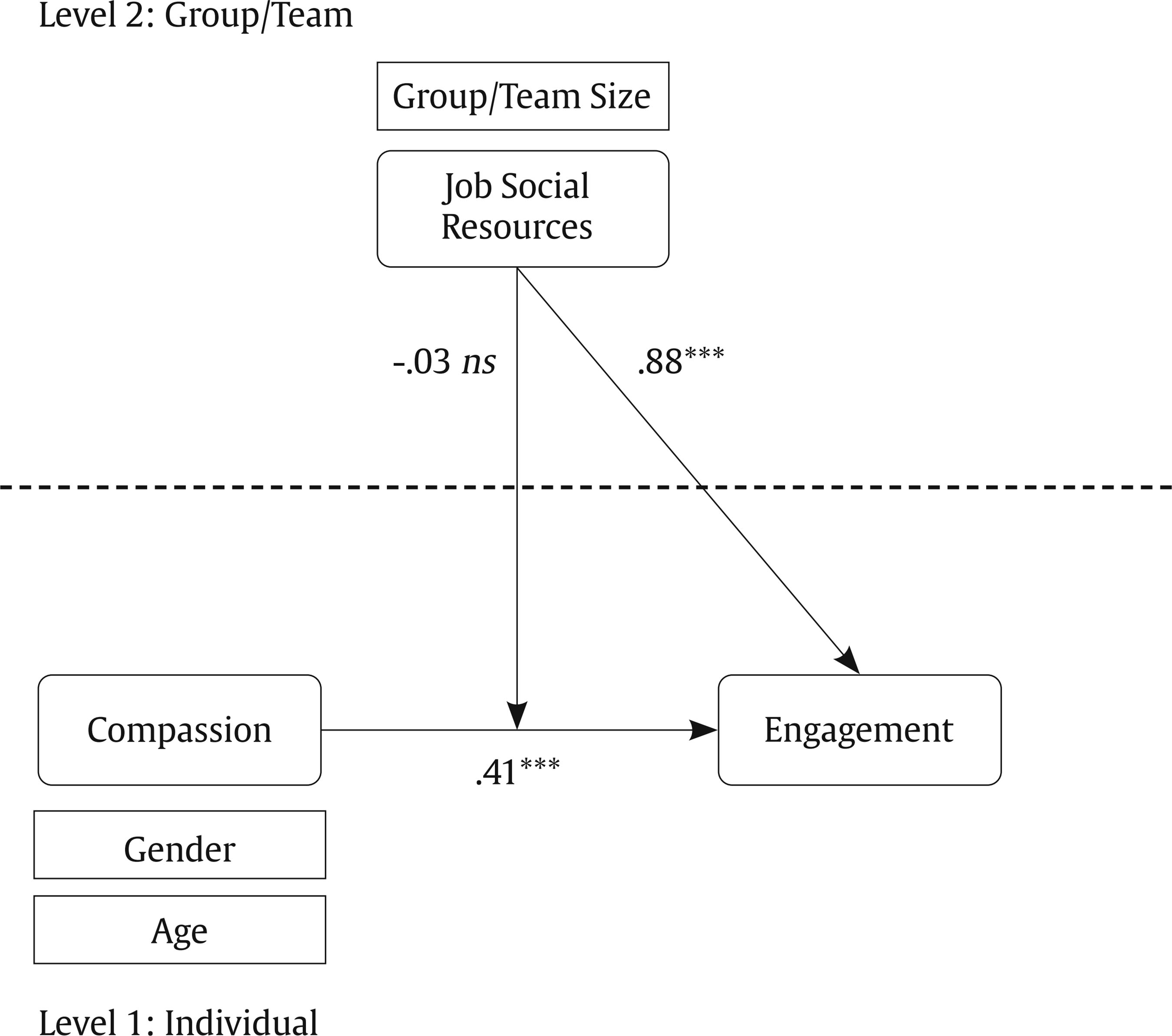 ***p < .001. To test Hypothesis 4, Model 4 included the variables of Model 3 while adding the cross-level interaction between team-level job social resources and individual-level compassion predicting engagement. Results demonstrate that there is not cross-level interaction (β = -.03, p = .09). Thus, Hypothesis 4 was not confirmed (see Figure 5). Table 5 presents the hierarchical linear models predicting burnout, according to Hypothesis 5. Model 5 incorporated both team-level variables to test the cross-level effects, that is, aggregated job social resources, along with control variables (group/team size) and at the individual level variables of compassion and burnout, along with the control variables (age and gender). Results for Model 5 demonstrated that aggregated job social resources are negatively and significantly related to burnout (β = -.89, p = .001), once the negative (individual-level) relationship between compassion and burnout has been controlled for (β = .41, p = .001). Therefore, Hypothesis 5 was confirmed. This model explored how job social resources can mitigate the negative impact of compassion on burnout, emphasizing the importance of the protective role of supportive work environments. Table 5 Results of the hierarchical linear models predicting burnout (ICC = 8%).  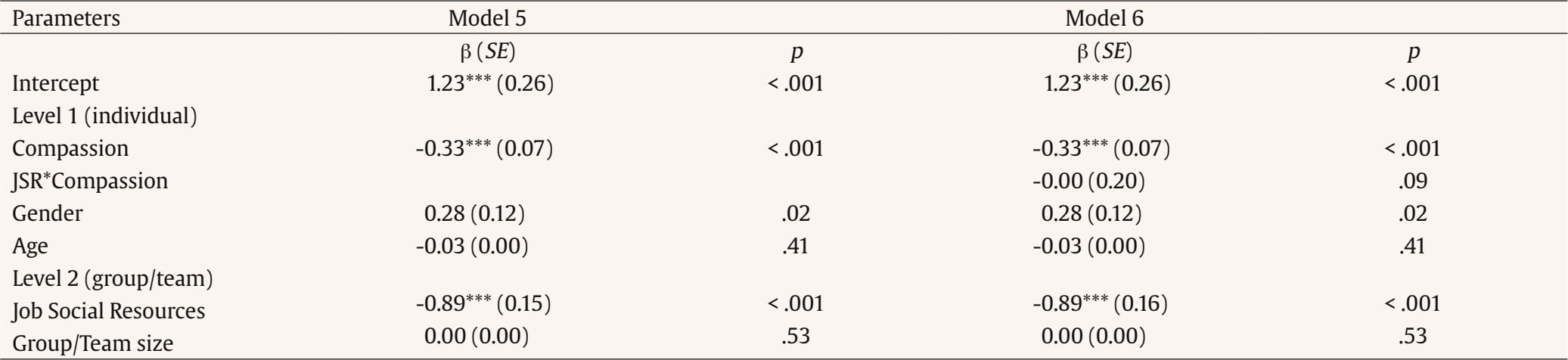 Note. ICC = Intraclass Correlation Coefficient; JSR = Job Social Resources; β = beta, + = standard errors. **p < .01, ***p < .001. Figure 6 Final Model Including the Results of the Cross-level Effects and the Cross-level Interaction for Job Social Resources, Compassion, and Burnout.  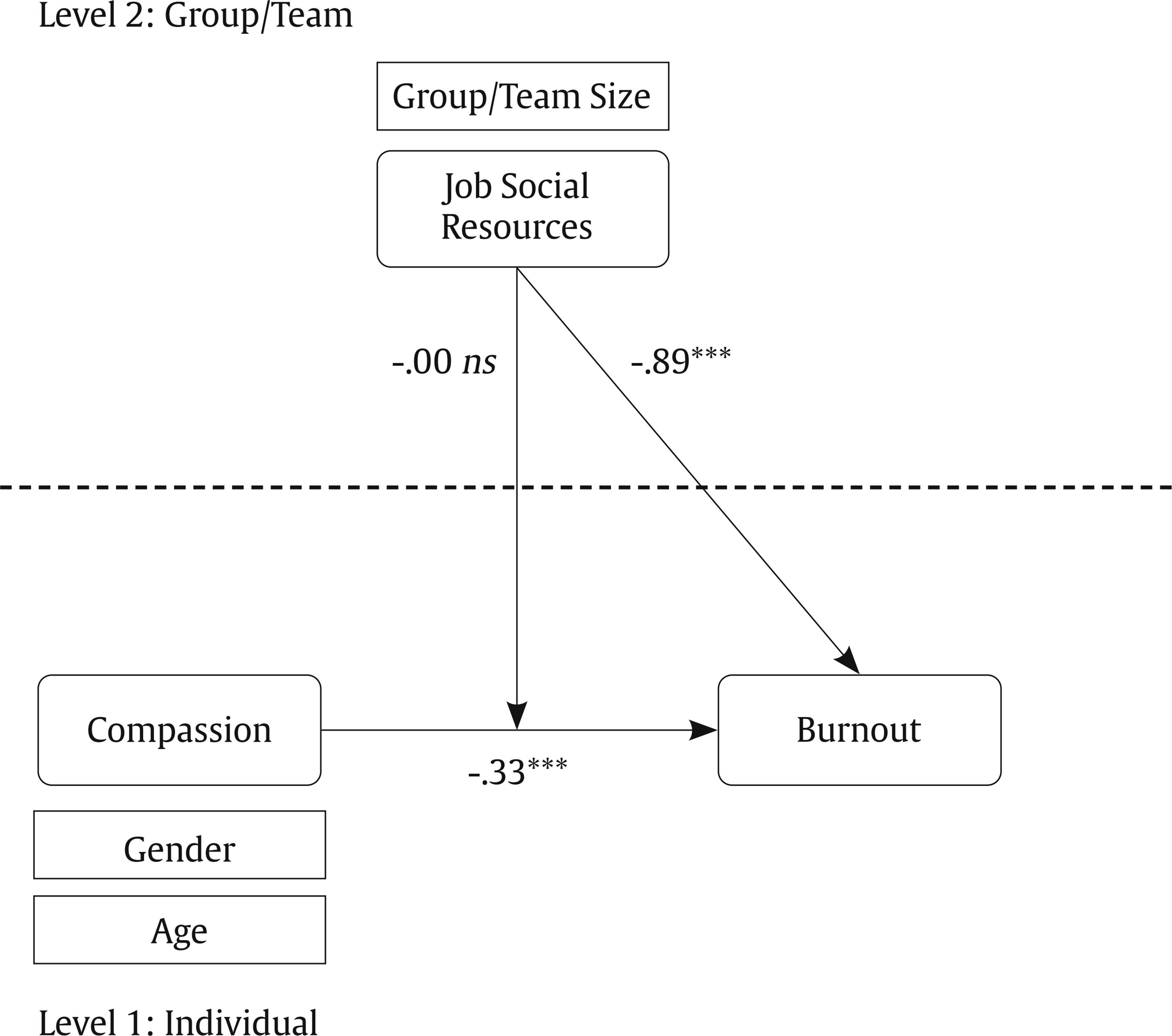 ***p < .001. To test Hypothesis 6, Model 6 incorporated the variables from Model 5 while adding the cross-level interaction between team-level job social resources and individual level-compassion in predicting burnout. Results revealed no significant cross-level interaction (β = -.00, p = .09), thus, failing to support Hypothesis 6 (see Figure 6). The present study examined the effects of job demands, compassion, and job social resources on employee engagement and burnout at both individual and group/team levels in Spain healthcare settings. Our findings offer valuable insights into the complex interplay of these factors and their impact on healthcare professionals’ well-being. The following discussion will delve into relevant literature with the aim of clarifying these findings, considering the direct relationships first and the hypothesized moderating effects afterwards to ease the rationale behind our interpretation. Our study found support for Hypothesis 1, revealing the positive association between team-level job social resources and individual compassion, even when considering the challenges posed by individual job demands. This aligns with previous research suggesting that supportive work environments can buffer the negative effects of job stress on compassionate behaviors (Cosley et al., 2010; Desveaux et al., 2023). The relationship between team-level resources and individual compassion highlights the importance of fostering a supportive team climate in healthcare settings. Hypothesis 3 was confirmed, pointing that job social resources at the team level have a positive association with employee engagement, a link that remains significant even when accounting for the individual-level relationship between compassion and engagement. These findings are consistent with recent studies highlighting the important role of team-level factors in promoting employee well-being in high-stress occupations (Cao et al., 2023; Van den Broeck et al., 2010; Wolter et al., 2018). Our results extend this understanding to the specific context of Spanish healthcare professionals. Additionally, Hypothesis 5 was confirmed, demonstrating the negative relationship between aggregated job social resources and burnout, controlling for the individual-level relationship between compassion and burnout. This finding highlights the multilevel dynamic at play, where team-level job social resources not only enhance personal resources like compassion but also play an important role in preventing negative outcomes like burnout (Kamphuis et al., 2021). However, the study did not find support for the hypothesized moderating effects of team-level job social resources (H2, H4, and H6). Contrary to our expectations, these resources did not significantly moderate the relationships between job demands and compassion, compassion and engagement, or compassion and burnout. These unexpected findings suggest that the influence of team-level resources on individual outcomes may be more direct than previously theorized (Kamphuis et al., 2021; Mazzetti & Schaufeli, 2022). The lack of support for these moderation hypotheses is particularly intriguing. It suggests that while team resources directly affect individual outcomes, they may not significantly alter the relationships between individual-level variables as initially suggested. Recent research has begun to explore the complexities of multilevel dynamics in healthcare organizations (Olvera et al., 2024; Ramšak et al., 2023) and our results contribute to this emerging area of study. This unexpected outcome highlights the need for more nuanced models of workplace interactions in high-stress healthcare environments. Furthermore, our findings underscore the importance of considering the multidimensional nature of work settings, particularly in healthcare (Braithwaite et al., 2017; De Angelis et al., 2022). The complex interplay between individual and team-level resources in our study suggests that the JD-R model could benefit from a more comprehensive multilevel perspective. This approach could help explain why we observed direct effects of team-level resources on individual outcomes, but not the expected moderating effects. One plausible explanation for these results is that the moderating influence of job social resources at the team level may operate through different mechanisms or on different timescales than initially hypothesized. As Kozlowski and Bell (2003) suggest, team-level processes often evolve more slowly than individual-level processes. Additionally, the healthcare context itself might play a role in these findings. The intense and often unpredictable nature of healthcare work, as described by Braithwaite et al. (2017) and Rosen et al. (2018), might create an environment where individual-level factors and immediate experiences have a more pronounced impact on outcomes than team-level factors. It may be possible to assume, therefore, that the immediate effects of individual experiences and perceptions overshadow any moderating influence of team-level resources in the short term. This temporal mismatch might explain why we observed direct effects but not moderating effects of team-level resources. Our study has several important implications for existing theoretical frameworks and contributes to advancing our understanding of occupational health in healthcare settings. Firstly, our findings extend the JD-R model (Bakker & Demerouti, 2014) by highlighting the importance of team-level resources in healthcare contexts. While the JD-R model traditionally focuses on individual-level processes, our results suggest that team-level factors play a crucial role in shaping individual outcomes. This calls for a more nuanced, multilevel approach to the JD-R model in healthcare settings (Katou et al., 2022; Li et al., 2023). Moreover, our results align with and further refine the HERO model (Salanova et al., 2012; Salanova et al., 2019) by demonstrating the direct effects of team-level resources on individual outcomes, providing empirical support for the model’s emphasis on organizational resources and practices. Our study indicates that the pathways through which these resources influence employee well-being may function more directly than previously conceptualized. This observation encourages a reconsideration of current understandings regarding resource-outcome relationships in healthcare settings. Our study’s conceptualization and empirical support of compassion as a personal resource contributes to the growing body of literature on personal resources in occupational health models. This approach enhances our understanding of the psychological mechanisms that help maintain employee well-being in demanding work environments (San Román-Niaves et al., 2022; San Román-Niaves et al., 2024). Additionally, our findings also highlight the relevance of considering cross-level effects in healthcare organizational research. The direct effects of team-level resources on individual outcomes, coupled with the lack of moderating effects, suggest that the dynamics between team and individual factors may be more complex than previously thought. The absence of moderating effects of team-level resources raises questions about the temporal dynamics of team processes in healthcare settings. Our results suggest that the impact of team-level factors may unfold differently over time compared to individual-level processes. Lastly, our study underscores the importance of considering the unique context of healthcare work when applying and developing organizational theories. The intense and often unpredictable nature of healthcare work may shape the way team and individual factors interact, calling for context-specific theoretical refinements. Our findings suggest that interventions aimed at increasing job social resources at the team level can foster a more compassionate and supportive work environment, which in turn enhances employee engagement and reduces burnout. Promoting supportive leadership might represent a key strategy. Leaders should adopt a supportive and compassionate leadership style, and organizations can facilitate this by designing training programs that help leaders understand the importance of compassion and how to model compassionate behavior. For instance, supportive leadership can create an atmosphere among team members of trust and safety, which is crucial for fostering compassion among team members (Brohi et al., 2021; Lown et al., 2019). Based on our results, enhancing team cohesion can be seen as another important line to consider. Implementing team-building activities and interventions that promote team cohesion and mutual support can build strong interpersonal relationships among team members, essential for creating a supportive work environment. It is widely documented that team cohesion enhances emotional resilience and provides the psychological resources needed to express compassion, even under stressful conditions (Hartwig et al., 2020; Meneghel et al., 2016; Neff & Germer, 2013; Salanova et al., 2012). In that direction, comprehensive assessments of job social resources are essential to identify areas needing improvement. Regular assessments using comprehensive tools that capture various aspects of the team’s social environment, such as social support climate, positive leadership, and coordination, can help organizations tailor their interventions to meet the specific needs of their teams. Finally, developing compassion-focused interventions is also vital. Introducing compassion and mindfulness-based interventions for HCPs can improve well-being by helping them manage their stress and cultivate compassion. Creating a compassionate work environment involves fostering a culture that values and promotes compassion. Healthcare organizations should recognize and reward compassionate behaviors, provide opportunities for peer support, and ensure that job-related social resources are readily available. However, this can be challenging in a work setting characterized by complex, dynamic, and changing regulatory environments (Rosen et al., 2018). Limitations and Research Directions First, as a cross-sectional study, we cannot establish predictive conclusions about the causal relationships among the variables studied. Although we collected data from multiple services across different hospitals, future research should employ longitudinal or experimental designs to provide more robust evidence for the causal relationships among job demands, compassion, job social resources, engagement, and burnout. Longitudinal studies, in particular, can help elucidate the temporal dynamics and potential bidirectional influences between these variables. Second, the use of self-report measures introduces the potential for common method variance bias. We mitigated this limitation by employing Harman’s single-factor test, which indicated no substantial common method variance in our data. Also, the CMF analysis showed a good model fit, confirming that common method bias does not significantly affect the relationships between the latent variables. Nonetheless, future studies could benefit from incorporating multi-method approaches, including objective measures and third-party evaluations, to validate self-reported data. Third, the non-confirmation of some hypotheses could be explained by the cross-sectional design of the study, which may not adequately capture the temporal dynamics of team-level processes, as well as by the particularities of the healthcare context, where individual-level factors tend to dominate. Additionally, the observed effects of team resources might primarily be direct rather than moderating, as suggested by recent research. Fourth, our data collection was conducted before the COVID-19 pandemic, which significantly altered job demands and working conditions in healthcare. The dramatic changes in workload and uncertainty during the pandemic may limit the generalizability of our findings to post-pandemic contexts. However, our results provide a valuable foundation for developing interventions aimed at promoting compassion and engagement and reducing burnout in healthcare professionals, especially considering the heightened emotional distress experienced by frontline workers during the pandemic. Fifth, some variables in our study were measured using single-item scales, which, while efficient, may not capture the full complexity of the constructs. Single-item scales were chosen based on evidence supporting their validity for specific constructs like engagement (Schaufeli et al., 2017) and burnout (Houdmont et al., 2022), while they save time for respondents and companies to answer the questionnaire (Gil-Beltrán et al., 2020). Future research should employ multi-item scales to enhance the reliability and validity of these measures. Lastly, from a methodological perspective, our study suggests further future research direction. The Brief Compassion Scale used in this study demonstrated only moderate internal consistency. Future studies should consider employing more comprehensive, multi-item scales to measure compassion. These longer scales could provide a more nuanced and psychometrically robust assessment of the construct, potentially capturing its full complexity and improving the overall reliability of the measurements. Additionally, exploring potential non-linear relationships and threshold effects could yield a more comprehensive understanding of how team-level factors influence individual outcomes in healthcare settings. This study provides important insights into the multilevel dynamics of compassion, job social resources, and well-being in healthcare settings. Our findings highlight the importance of team-level job social resources in improving individual compassion, engagement, and reducing burnout among healthcare professionals, even when job demands are high. The direct positive effects of team-level job social resources, together with the unexpected absence of moderating effects, point to a more nuanced relationship between organizational levels than previously thought. These results expand on both the JD-R and HERO models, emphasizing the complex interplay between individual and team factors in healthcare organizations. This research lays the groundwork for developing targeted interventions to cultivate compassionate, engaged, and resilient healthcare workforces, ultimately improving both employee well-being and patient care. Conflict of Interest The authors of this article declare no conflict of interest. ACKNOWLEDGEMENTS We would like to thank Cristian Coo in the first phases of the article as well as to Alyona Mezentseva, Antonio Ortiz Vázquez, and Juan José Reyes Luján for their support in performing the statistical analyses. Cite this article as: San Román-Niaves, M., De Angelis, M., Llorens, S., Salanova, M. (2024). A multilevel model of compassion in healthcare organizations. Journal of Work and Organizational Psychology, 40(3), 151-163. https://doi.org/10.5093/jwop2024a13 Funding This research was supported by the Ministry of Science and Innovation from Spain (MCIN/AEI/10.13039/501100011033), project xxxPID2020-119993RB-I00, and Generalitat Valenciana (ACIF/2020/343). References |
Cite this article as: Román-Niaves, M. S., De Angelis, M., Llorens, S., & Salanova, M. (2024). A Multilevel Model of Compassion in Healthcare Organizations. Journal of Work and Organizational Psychology, 40(3), 151 - 163. https://doi.org/10.5093/jwop2024a13
Correspondence: llorgum@uji.es (S. Llorens).Copyright © 2026. Colegio Oficial de la Psicología de Madrid








 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS