The Impact of a Workplace Sleep Program on Employee Well-being: A Pre-post Design Intervention Study
[El efecto de un programa de sueño en el puesto de trabajo en el bienestar de los empleados: un estudio de intervención con diseño pre-post]
Alfredo Rodríguez-Muñoz, Mirko Antino, Alejandro Díaz-Guerra, & Geraldy Sepúlveda Paez
Universidad Complutense de Madrid, Spain
https://doi.org/10.5093/jwop2025a9
Received 30 April 2025, Accepted 7 July 2025
Abstract
This study investigates the impact of a workplace sleep program on employee well-being using a pre-post intervention design. Conducted at a large public university, the program aimed to address sleep-related issues among early-career researchers. A total of 49 participants took part in a series of psychoeducational sessions that focused on sleep hygiene, relaxation techniques, and the relationship between stress and sleep. Participants wore actigraph devices to objectively measure their sleep patterns both before and after the intervention, with follow-up assessments conducted four months later. The results indicated significant improvements in both objective and self-reported sleep, as well as overall well-being. Additionally, participants reported reduced perception of exposure to workplace bullying behaviors. These findings suggest that implementing structured sleep programs can be an effective strategy for organizations seeking to enhance employee well-being and mitigate the adverse effects of sleep deprivation.
Resumen
Este estudio investiga el efecto de un programa de sueño en el trabajo en el bienestar de los empleados, utilizando un diseño de intervención pre-post. Realizado en una gran universidad pública, el programa tuvo como objetivo abordar problemas relacionados con el sueño en investigadores en las primeras etapas de su carrera. Un total de 49 participantes asistieron a sesiones psicoeducativas centradas en la higiene del sueño, técnicas de relajación y la relación entre el estrés y el sueño. Los participantes llevaron actígrafos para medir objetivamente sus patrones de sueño antes y después de la intervención, con una evaluación del seguimiento realizada cuatro meses después. Los resultados dieron cuenta de mejoras significativas en el sueño objetivo como en el autoinformado, así como en el bienestar general. Además, los participantes reconocieron una reducción de la percepción de la exposición a comportamientos de acoso psicológico en el trabajo. Los resultados indican que la puesta en marcha de programas de sueño puede ser una estrategia eficaz en las empresas que buscan aumentar el bienestar de sus empleados y mitigar los efectos negativos de la privación de sueño.
Palabras clave
Intervención sobre el sueño en el trabajo, Bienestar de los empleados, Acoso psicológico en el trabajo, Sueño objetivoKeywords
Workplace sleep intervention, Employee well-being, Workplace bullying, Objective sleepCite this article as: Rodríguez-Muñoz, A., Antino, M., Díaz-Guerra, A., & Sepúlveda Paez, G. (2025). The Impact of a Workplace Sleep Program on Employee Well-being: A Pre-post Design Intervention Study. Journal of Work and Organizational Psychology, 41(2), 85 - 92. https://doi.org/10.5093/jwop2025a9
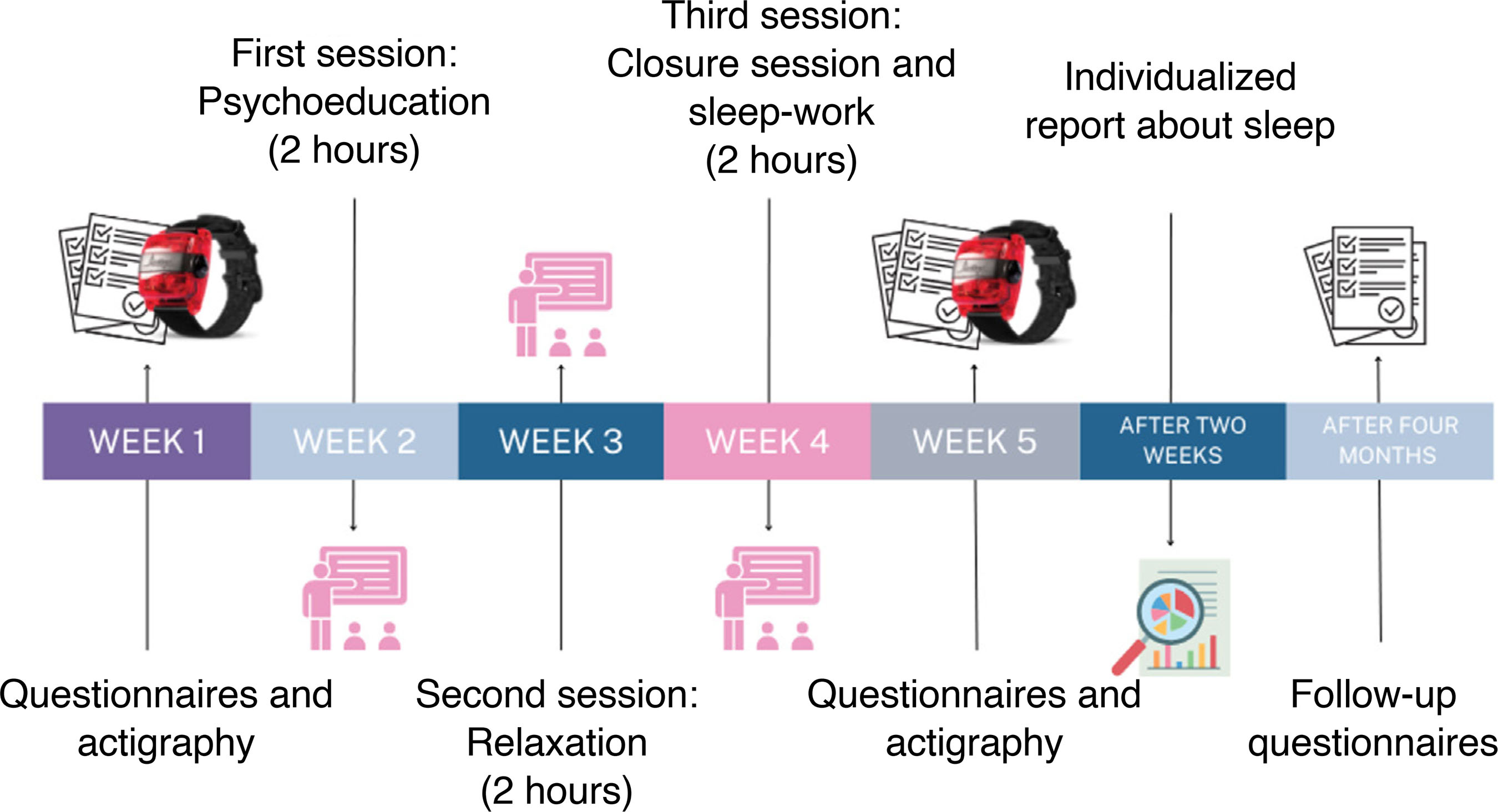
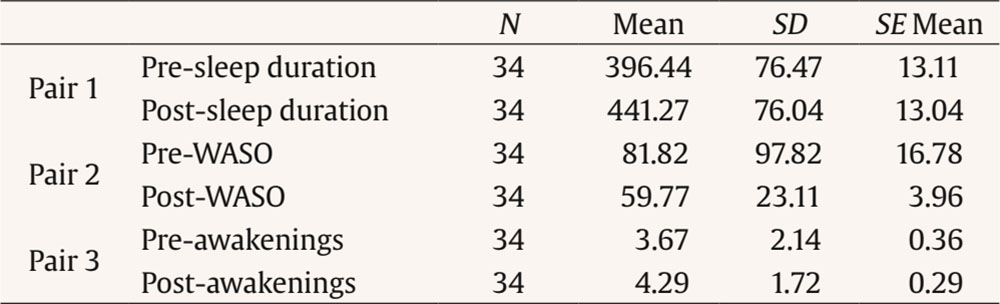
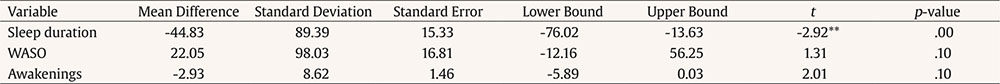
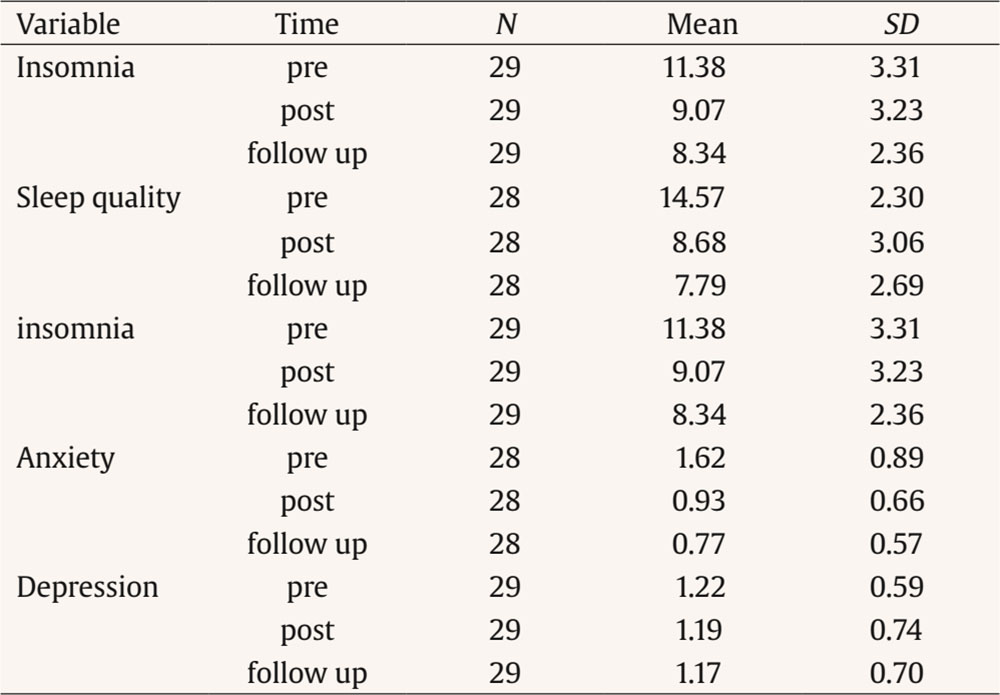
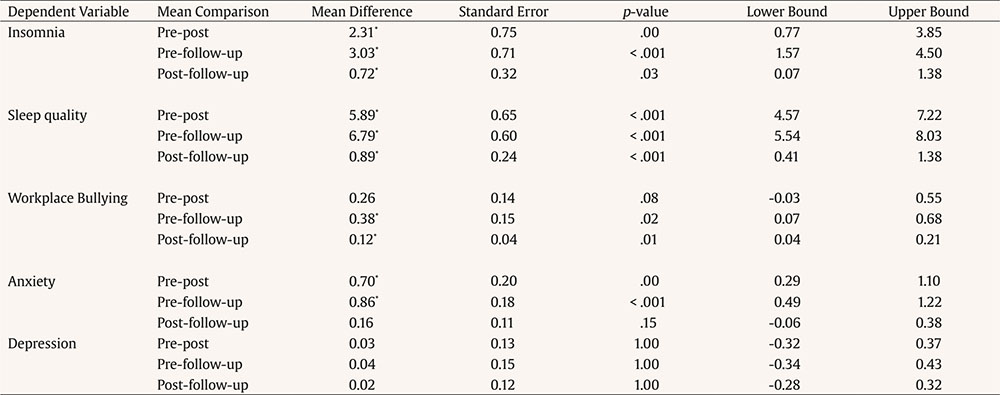
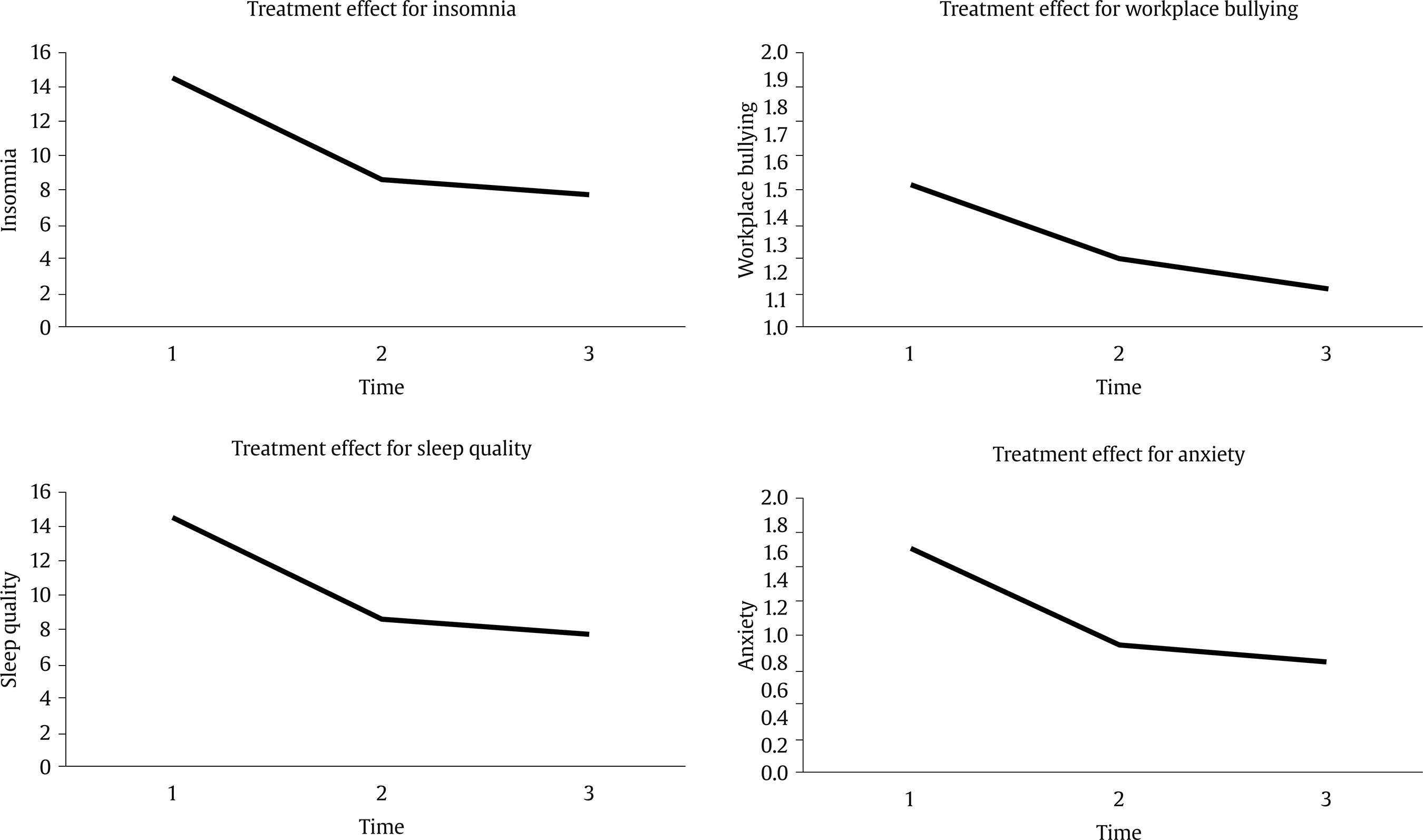
Correspondence: alfredro@ucm.es (A. Rodríguez-Muñoz).Sleep problems have been increasingly associated with various adverse health outcomes, including chronic diseases and early mortality (e.g., Luyster et al., 2012). Evidence suggests that insufficient sleep duration and poor sleep quality are causally linked to heightened risks for conditions such as obesity and diabetes, as well as mental health issues, including anxiety and depression (Freeman et al., 2020; Kurnool et al., 2023). Given that adults spend a substantial portion of their waking hours at work, the workplace is a critical yet underused setting for promoting sleep health. While workplace wellness programs commonly focus on nutrition and exercise, sleep has largely been neglected (Robbins et al., 2019). The bi-directional relationship between work and sleep further underscores the importance of addressing sleep in organisational settings. Work-related factors can influence sleep quality, and in turn sleep impacts employee performance, well-being, and social dynamics (Yap et al., 2020). To address this gap, this study employs a pre-post intervention design to examine how workplace sleep interventions can improve employee well-being by adopting a dual-focus approach. This approach evaluates both primary outcomes directly related to sleep and secondary outcomes reflecting broader aspects of well-being and workplace interactions. The primary outcomes of the study—objective measures such as actigraphy-based sleep quality, sleep duration, and frequency of nighttime awakenings, as well as subjective evaluations like self-reported sleep satisfaction—are directly aligned with the intervention’s main goal: improving sleep. By focusing on these metrics, the study provides a clear evaluation of the intervention’s effectiveness in enhancing sleep patterns. In addition to these primary outcomes, the inclusion of secondary outcomes broadens the research scope. By examining how improvements in sleep influence mental health outcomes like anxiety and depression, as well as social dynamics such as perceptions of workplace bullying, the study investigates the broader impacts of better sleep. This dual-focus approach offers valuable insights into the far-reaching benefits of sleep interventions, emphasizing their potential to enhance both individual well-being and workplace environments. Sleep Interventions in Workplace Settings The growing recognition of sleep as a critical health determinant has led to the development of various workplace interventions aimed at improving sleep. These initiatives range from educational workshops to organizational changes, such as optimizing work schedules, and have gained traction across various industries. Sleep deprivation continues to be a significant issue, with approximately 30% of U.S. employees reporting insufficient sleep (Centers for Disease Control and Prevention, 2016). This sleep deficit is linked to several negative workplace outcomes, including reduced performance, increased absenteeism, and higher disability rates (Bioulac et al., 2017; Trinkoff et al., 2001). Research demonstrates that sleep interventions can yield promising results. For example, individualized sleep hygiene training and personalized sessions incorporating relaxation techniques or sleep restriction have been shown to improve sleep duration and quality (Nishinoue et al., 2012). Similarly, Adler et al. (2017) found that actigraphy feedback interventions enhanced sleep duration and reduced sleep problems among soldiers. Broader workplace interventions have also reported benefits. For example, Crain et al. (2019) demonstrated that a work-family intervention improved both actigraphic measures of sleep quantity and self-reported sleep quality. Despite these advances, there are still gaps in the literature. Most studies on workplace sleep interventions rely on self-reported data (Kaku et al., 2012; Kodsi et al., 2022; Nishinoue et al., 2012; Robbins et al., 2022), or online delivery methods (Hershner & O’Brien, 2018; Linardon et al., 2024; Ong et al., 2023), which may limit validity and generalizability. In-person programs with tailored treatments often yield stronger outcomes (Murawski et al., 2018; Nishinoue et al., 2012). Furthermore, few interventions evaluate secondary outcomes, such as mental health and social dynamics (Redeker et al., 2019). To address these limitations, we hypothesize: Hypothesis 1: The intervention will improve employees’ sleep quantity (i.e., increase objective total sleep time) and sleep quality (i.e., reduce objective WASO, reduce awakenings, subjective sleep quality, and subjective insomnia symptoms) at the immediate post-test (1-week) and 4-month follow-up data collections relative to baseline. The Importance of Sleep for Employee Well-Being The Affective Regulation Model posits that inadequate sleep disrupts emotional functioning, increasing negative emotions and reducing positive ones, which contributes to anxiety and depression (Palmer & Alfano, 2017). Sleep deprivation impairs key brain areas, such as the medial prefrontal cortex and amygdala, which are involved in emotional regulation, resulting in difficulties in managing emotional responses. This creates a cycle, particularly for those already suffering from anxiety or depression, where emotional struggles exacerbate sleep disturbances, further intensifying mental health issues. Sleep disturbances also affect workplace performance and interpersonal relationships, impairing decision-making, emotional control, and social interactions. For individuals with anxiety and depression, these challenges are even more pronounced. Stressful work environments, long hours, and irregular schedules often exacerbate sleep disruptions, creating a self-reinforcing cycle that heightens emotional difficulties and diminishes productivity. Conversely, adequate sleep enhances emotional resilience, allowing individuals to manage stress more effectively, reduce anxiety and depressive symptoms, and maintain better overall well-being. Based on this reasoning, we hypothesize: Hypothesis 2: The intervention will improve employees’ well-being (reduce anxiety and depression symptoms) at the immediate post-test (1-week) and 4-month follow-up data collections relative to baseline. Workplace Bullying and Sleep Problems Stressful social contexts are frequently recognized as significant triggers for sleep disturbances. For instance, one of the most immediate consequences of experiencing bullying is the onset of sleep-related issues (e.g., Nielsen & Einarsen, 2012). Similarly, Magee et al. (2015) demonstrated that workplace bullying is closely linked to poorer sleep quality. Longitudinal studies further support this connection (Niedhammer et al., 2009; Nielsen et al., 2021), highlighting that sleep disturbances are among the persistent effects of bullying (Rodríguez-Muñoz et al., 2020). The relationship between workplace bullying and sleep disturbances may not be strictly unidirectional; emerging evidence suggests that this connection could be reciprocal. For example, Rodríguez-Muñoz et al. (2015) observed a bidirectional relationship over time between anxiety, energy levels, and workplace bullying, suggesting that internal states can influence both the experience and perception of bullying. Workplace bullying, defined as persistent negative acts directed at one or more individuals by colleagues or superiors (Einarsen et al., 2020), is a recognized stressor that both affects and is affected by an individual’s mental and physical state. The Stressor Perception Hypothesis (Lang et al., 2011; Rudolph et al., 2025) provides a useful framework for understanding how sleep may influence perceptions of workplace bullying. This hypothesis suggests that individuals’ interpretations of and responses to stressors depend not only on the external environment but also on their internal conditions, including sleep quality. Poor sleep has been shown to increase sensitivity to negative stimuli, amplifying the perception of threat in the workplace and causing ambiguous or neutral social interactions to seem hostile (Beattie et al., 2015). Conversely, adequate sleep supports emotional regulation and improves the accuracy of social cue interpretation, potentially reducing perceptions of bullying. De Lange et al. (2005), through the gloomy perception mechanism, argue that individuals in poor health—such as those experiencing chronic sleep deprivation—are predisposed to evaluate their surroundings more negatively. Similarly, Lazarus et al. (1985) emphasized the importance of viewing health and stress-related variables as components of a dynamic system. Consequently, sleep and perceptions of workplace bullying interact in complex ways over time. In this context, improving sleep quality could serve as an effective workplace intervention. By addressing sleep-related issues, organizations can help employees reduce hyper-reactivity to social stressors, enhance their ability to manage interpersonal challenges, and potentially decrease perceptions of bullying. Therefore, we hypothesize: Hypothesis 3: The intervention will improve employees’ perceptions of being exposed to workplace bullying behaviours at the immediate post-test (1-week) and 4-month follow-up data collections relative to baseline. Participants and Procedure Participants in this study were researchers from a large public university. To be eligible, individuals had to be researchers within the organization and located at one of the two campuses where data collection took place. Data were collected at two distinct time points: one group in May and another in November 2023. Early-career researchers represent a unique population navigating a critical transitional period as they embark on their academic and professional journeys. This stage often involves numerous challenges, including adapting to demanding work schedules, managing the pressures of publication and grant writing, and balancing personal and professional responsibilities. These factors, combined with the irregular and often extended working hours typical in academic settings, make this group particularly vulnerable to sleep loss. Recruitment was carried out through various social media platforms and advertisements within the organization. Initially, face-to-face meetings were held, where research assistants instructed participants on how to complete the questionnaires, explained the objectives of the intervention, and provided actigraphy devices along with usage instructions. The intervention was conducted in person rather than digitally or online, as in-person programs with individualized treatment tend to show stronger effects (Murawski et al., 2018; Nishinoue et al., 2012). In collaboration with the organization, we opted to include all interested participants in the intervention, without a control group or waitlist. This decision was made to ensure equitable access to potential benefits and to prioritize the well-being of employees. By doing so, we aimed to respect participants’ right to benefit from a potentially positive health intervention, given the immediate relevance of sleep improvement in occupational health. This intervention is based on previous work that incorporates similar elements (e.g., Blake et al., 2016; Crain et al., 2019). This study employed a pre-post design with a follow-up assessment conducted four months later. In addition to the initial informative session with each participant, three group sessions were held, each lasting two hours, for a total of six hours. These sessions included: (1) psychoeducation on general sleep guidelines and sleep hygiene practices to help establish proper bedtime routines; (2) relaxation techniques designed to reduce cognitive activation and alleviate muscle tension, thus promoting better sleep; and (3) a final session addressing the relationship between stress and sleep, followed by a wrap-up to conclude the intervention. Participants were also asked to wear an ActiGraph (wGT3X-BT) on their non-dominant wrist continuously for seven consecutive days, both before and after the intervention. Two weeks after the intervention, participants received a personalized sleep report, and those who requested it were offered an online meeting to discuss their individual results. In addition to the evaluation at the end of the intervention, a follow-up assessment was conducted at the four-month mark, using questionnaire measures only. Figure 1 provides a graphical representation of the research design. Participants diagnosed with sleep or mental health disorders were excluded from the study (n = 4), although they were invited to attend the sleep workshop. The final sample included 49 participants (68% female), with an average age of 29.15 years (SD = 4.18, range: 24-37 years). During the initial evaluation and intervention phase, a total of 49 participants took part in the study. However, at the immediate assessment involving actigraphy measurements, the sample size decreased to 34 participants. By the final follow-up assessment, only 29 participants remained. Data collection was facilitated through Qualtrics.com, and the research protocol was approved by the local ethics committee. Informed consent was obtained from all individual participants included in the study. Measures Self-reported Measures Sleep Quality. This was measured using the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989), a standardized measure that has been widely used in sleep research. The PSQI is composed of 19 items that produce a global sleep quality index and 7 component scores reflecting sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction. Each component is scored from 0 to 3 points. The total index score is between 0 and 21, with higher scores indicating a lower quality of sleep. The scale demonstrated adequate reliability across three waves (α = .79, .80, and .75, respectively). Insomnia. The Insomnia Severity Index (ISI; Bastien et al., 2001) was used for this study. The ISI is a screening tool composed of seven items that evaluate various aspects of insomnia, including difficulties initiating sleep, staying asleep, early morning awakenings, excessive daytime sleepiness, reduced daytime functioning, dissatisfaction with sleep quality, and sleep concerns. Each item is rated on a five-point Likert scale ranging from 0 (none or not at all) to 4 (very severe problem), with higher total scores indicating greater insomnia severity. The scale demonstrated adequate reliability across three waves (α = .83, .84, and .77, respectively). Depression and Anxiety. Symptoms of depression and anxiety were measured using the Patient Health Questionnaire, a brief four items screening tool (Löwe et al., 2010). Participants were asked how frequently they had been “bothered by” specific problems over the past month, including “feeling nervous, anxious, or on edge,” “inability to stop or control worrying,” “reduced interest or pleasure in activities,” and “feeling down, depressed, or hopeless.” Responses were recorded on a 5-point Likert scale ranging from 0 (never or almost never) to 4 (nearly every day). We separated the anxiety and depression scores, with higher scores indicating greater severity of symptoms. The scale showed strong reliability for both depression (α = .71, .75, and .83) and anxiety (α = .74, .80, and .82) across three waves. Workplace Bullying. It was measured with the Short-Negative Acts Questionnaire (S-NAQ; Notelaers et al., 2018). The nine items describe negative acts in terms of personal bullying (e.g., “gossiping”) and work-related bullying (e.g., “being withheld information”). Respondents indicated how frequently they had been exposed to each of these negative acts during the last months on a scale from 1 (never) to 5 (daily). In The scale demonstrated adequate reliability across three waves (α = .81, .80, and .71, respectively). Objective Measures Sleep, Actigraphy Measures. We utilized wGT3X-BT actigraphy to assess objective sleep outcomes. Sleep metrics were calculated using algorithms embedded within the ActiLife 6 software (ActiGraph Ltd), which processes movement data recorded in 60-second intervals. Participants were instructed to wear the accelerometer on their non-dominant wrist during the week preceding and following the intervention. The sleep parameters derived from actigraphy included total sleep duration (the total time spent asleep at night, excluding wake periods), Wake After Sleep Onset (WASO, the number of minutes awake between sleep onset and final awakening), and the frequency of awakenings during the night, all measured in minutes. Control Variables. We adjusted for some control variables in the analyses. First, gender (1 = male, 2 = female) was included, given consistent evidence from the literature indicating a higher prevalence of sleep problems among women (e.g., Kudielka et al., 2004). Additionally, to account for potential seasonal effects, we controlled for the timing of each intervention, as these were conducted in two groups during different periods of the year (May and November). However, analyses including these control variables demonstrated that their inclusion did not influence the results. Therefore, these controls were excluded from the final analyses for reasons of parsimony (Becker, 2005; Becker et al., 2016). Statistical Analysis Different statistical approaches were applied based on the available assessment time points to evaluate the effects of the intervention. For the objective sleep indicators, paired sample t-tests were conducted to assess changes in sleep duration, WASO, and awakenings between pre- and post-intervention measurements. Cohen’s d was calculated to estimate effect sizes, as only two-time points were available for these variables. For the self-reported variables, repeated measures ANOVA was employed to analyse changes over time in insomnia, sleep quality, workplace bullying, anxiety, and depression. These variables were assessed at three-time points: pre-intervention, post-intervention, and follow-up. Partial eta-squared () was calculated as a measure of effect size. Post-hoc pairwise comparisons were performed to identify significant differences across time points, enabling the evaluation of the intervention’s immediate and sustained effects. All analyses were conducted using SPSS version 26. The descriptive statistics for the paired samples analysis of the objective variables are presented in Table 1. Sleep Duration For sleep duration, the paired sample mean comparison t-test revealed a significant pre-post effect, t = -2.19 (df = 33), p = .02, effect size (estimated through Cohen’s d) = 0.22, showing a significant increase of sleep duration after the intervention (see Table 2). WASO For WASO, the paired sample mean comparison t-test revealed no significant pre-post effect, t = 1.31 (df = 33), p = .10, effect size (estimated through Cohen’s d) = 0.50, showing no difference after the intervention (see Table 2). Awakenings For Awakenings, the paired sample mean comparison t-test revealed no significant pre-post effect, t = -1.32 (df = 33), p = .10, effect size (estimated through Cohen’s d) = -0.27, showing no difference after the intervention (see Table 2). Descriptive statistics for the self-reported variables are presented in Table 3. Insomnia For Insomnia, the repeated measures ANOVA revealed a significant effect for time, F(2, 29) = 12.81, p < .001, partial η2 = .31. Pairwise comparisons revealed significant time effects in all three comparisons, from pre- to post-, post- to follow-up and pre- to follow-up-assessment. This suggests that a significant change was achieved not only at post-assessment and maintained at follow-up, but that further improvement occurred from post-assessment to follow-up (see Table 4 and Figure 2). Sleep Quality For sleep quality, the repeated measures ANOVA revealed a significant effect for time, F(2,29) = 97.35, p = .01, partial η2 = .78. Pairwise comparisons revealed significant time effects in all three comparisons, from pre- to post-, post- to follow-up and pre- to follow-up-assessment. This suggests that significant change was not only achieved at post-assessment and maintained at follow-up, but additionally, improvement occurred from post- to follow-up assessment (see Table 4 and Figure 2). Anxiety For the anxiety, the repeated measures ANOVA revealed a significant effect for time, F(2, 29) = 15.04, p = .01, partial η2 = .36. Pairwise comparisons revealed significant time effects comparison, from pre to post, as well as from pre to follow-up-assessment, while no significant effect was found in the post- to follow-up comparison. This suggests that significant change was only achieved at pre-post-assessment and the decrease was maintained in the follow-up, while no additional improvement occurred from post- to follow-up assessment (see Table 4 and Figure 2). Depression For the depression, the repeated measures ANOVA revealed no significant effect for time, F(2, 29) = 0.51, p = .95, partial η2 = .01. Workplace Bullying For workplace bullying, the repeated measures ANOVA revealed a significant effect for time, F(2, 29) = 5.11, p = .01, partial η2 = .16. Pairwise comparisons revealed significant time effects comparison, from pre to post (significant p < .10), pre to follow-up, and post to follow-up comparison. This suggests that a significant change was achieved not only at post-assessment (albeit with a tendency) and maintained at follow-up, but that further improvement also occurred from post-assessment to follow-up (see Table 4 and Figure 2). The present study aimed to evaluate the effectiveness of a workplace sleep intervention program. Our results demonstrate substantial improvements in both sleep parameters and employee well-being outcomes, supporting the value of workplace-based sleep health initiatives. The most immediate outcome of our intervention was the substantial improvement in both objective and subjective measures of sleep duration and quality among participants. Among the objective measures, only sleep duration showed significant improvements, while both sleep quality and insomnia symptoms, which were self-reported, also demonstrated notable improvements. The findings indicate moderate to small effects on objective sleep measures while revealing large effects on self-reported sleep outcomes. These results align with the meta-analysis conducted by Murawski et al. (2018), which found medium to small effects, particularly in general populations compared to clinical populations, where the effects were more pronounced. These findings are consistent with previous research demonstrating that sleep hygiene interventions can effectively enhance sleep patterns in workplace settings. For example, a recent research by Ong et al. (2023) demonstrated that a brief and personalized online sleep education intervention significantly improved sleep behaviors and sleep quality scores among working adults with short sleep. In addition to improvements in sleep, the results revealed a significant increase in the overall well-being of employees, as evidenced by a reduction in symptoms of anxiety, although no corresponding changes in depression were observed. This finding supports the hypothesis that sleep quality is intrinsically linked to mental health, as documented in the literature (Freeman et al., 2020). For instance, Freeman et al. (2017) conducted a randomized controlled trial that demonstrated the positive effects of a 10-week cognitive-behavioral therapy for insomnia (CBT-I) program on young adults attending university. Their study not only showed significant improvements in sleep quality but also highlighted reductions in symptoms of both depression and anxiety at post-treatment follow-up. Similarly, a meta-analysis by Kodsi et al. (2022) highlights that psychological interventions, particularly cognitive-behavioral approaches, positively impact secondary outcomes such as anxiety and depression. These findings underscore the potential of targeted sleep interventions to enhance mental health, reinforcing the idea that improved sleep can contribute to better emotional well-being. The observed pattern of improvement in anxiety symptoms without similar changes in depression can be explained through several theoretical frameworks and mechanisms. First, anxiety and sleep share more immediate and bidirectional neurobiological pathways compared to depression. Sleep disruption activates the hypothalamic-pituitary-adrenal axis (HPA) and increases cortisol levels, which directly influences anxiety responses. When sleep quality improves, there is typically a rapid downregulation of this stress response system, leading to reduced anxiety symptoms (Chrousos, 1998). Second, depression, in contrast, involves more complex and chronic alterations in cognitive processes and neurotransmitter systems, which may require longer-term interventions to modify (Gotlib & Hammen, 2009). The temporal nature of anxiety versus depression also helps explain these differential effects. Anxiety tends to be more state-dependent and situationally reactive, making it more responsive to immediate improvements in sleep quality (Alvaro et al., 2013). In contrast, depression often involves more stable, trait-like characteristics and negative cognitive schemas that may be more resistant to short-term improvements in sleep (Beck & Alford, 2009). The persistent nature of depressive symptoms suggests that while sleep is a contributing factor, it may not be sufficient as a standalone intervention for addressing depression. One noteworthy finding was the improvement in participants’ perceptions of workplace bullying, shedding light on a complex relationship between sleep quality and workplace social dynamics—a topic that has received limited attention in previous research. The results suggest that enhanced sleep quality may positively influence how employees interpret and respond to social interactions at work. This aligns with the Stressor Perception Hypothesis (Lang et al., 2011; Rudolph et al., 2025), which posits that individuals’ internal states, such as sleep quality, shape their appraisals of environmental stressors. Specifically, better sleep may lead to a more balanced evaluation of workplace situations, reducing the likelihood of perceiving interactions as hostile or threatening. Research supports this notion, showing that poor sleep increases emotional sensitivity and hypervigilance to negative stimuli, often causing neutral or ambiguous interactions to be perceived as adversarial (Beattie et al., 2015; Goldstein-Piekarski et al., 2015). This underscores the critical role of sleep in regulating emotional and cognitive processes related to interpersonal dynamics. Strengths and Limitations The methodological approach employed in our study, combining objective actigraphy data with self-reported measures, provides robust evidence for the intervention’s effectiveness. However, we must acknowledge several limitations that should be considered when interpreting our findings. First, a significant limitation is the absence of a control group. Although we opted to include all interested participants in the intervention to ensure equitable access to potential benefits, this decision precludes us from definitively attributing the observed changes in sleep quality and related variables solely to the intervention. Without a control group, we cannot rule out the influence of external factors or confounding variables that may have contributed to the outcomes. In this sense, the study was conducted in two distinct phases, with data collection occurring in May and November 2023. This design choice helps mitigate concerns regarding seasonal effects, allowing for examining potential variations in outcomes across different times of the year. Second, the study did not utilize a randomized design. Randomization is important in experimental research as it helps eliminate selection bias and ensures that the groups being compared are equivalent at baseline. The lack of randomization limits the generalizability of our findings. Future research should consider implementing a randomized controlled trial to strengthen the evidence for the intervention’s effectiveness. Additionally, the focus on researchers from a public university raises questions about the generalizability of our results to other occupational contexts. Different workplace settings, with varying demands and organizational cultures, may yield different outcomes. However, this focus enhances our control over the specific challenges faced by our sample, minimizing exogenous effects on the intervention. Third, although some of the instruments used (e.g., instruments assessing insomnia, depression, anxiety, and workplace bullying) consisted of few items, they are widely validated scales with strong psychometric support. Therefore, their brevity is not considered a substantial threat to construct validity. Finally, we cannot determine whether any specific session of the intervention had a greater effect than others. Each session was designed to address different aspects of sleep and relaxation, but the lack of a detailed analysis of individual session impacts limits our understanding of which components were most beneficial. Notably, some authors argue that providing feedback on participants’ sleep patterns can be regarded as an intervention in itself (e.g., Adler et al., 2017). This perspective suggests that the intervention may consist of four sessions rather than three, as the personalized sleep report and subsequent discussions could significantly influence participants’ awareness and behaviors regarding their sleep. This potential overlap in intervention components complicates the evaluation of the individual effects of each session and underscores the need for further research to disentangle these elements. Practical Implications The results of this study highlight the critical importance of implementing workplace sleep interventions to enhance employee well-being. Given the significant improvements observed in both sleep quality and related mental health outcomes, organizations should prioritize sleep health as a fundamental component of their employee wellness programs. First, the positive impact of the intervention on both objective and subjective measures of sleep indicates that tailored sleep programs can effectively address the sleep challenges faced by employees. Organizations should develop and implement structured sleep workshops that provide employees with practical strategies for improving their sleep hygiene. These workshops could cover topics such as the importance of sleep, relaxation techniques, and guidance on creating a conducive sleep environment. By equipping employees with these tools, organizations can cultivate a culture that values and prioritizes sleep, ultimately leading to enhanced productivity and overall job satisfaction. Moreover, organizations should strive to adopt a holistic approach that encompasses not only individual-level sleep interventions but also addresses systemic factors such as workload management, work-life balance, and organizational culture (Fox et al., 2022). Failing to do so may result in a focus solely on the individual, which risks falling into what is known as “carewashing.” This term refers to superficial care initiatives that employees may perceive as inadequate in addressing the root causes of their issues (Song & Baicker, 2019). By taking a comprehensive approach, organizations can ensure that their efforts to improve sleep health are both meaningful and effective. In summary, this study provides evidence that sleep interventions in the workplace can significantly improve sleep quality, emotional well-being, and perceptions of workplace bullying. These results underscore the need for organizations to implement programs that address sleep health as an integral part of their wellness initiatives. By doing so, not only is the physical and mental health of employees improved, but a more positive and productive work environment is also fostered. Conflict of Interest The authors of this article declare no conflict of interest. Cite this article as: Rodríguez-Muñoz, A., Antino, M., Díaz-Guerra, A., & Sepúlveda Paez, G. (2025). The impact of a workplace sleep program on employee well-being: A pre-post design intervention study. Journal of Work and Organizational Psychology, 41(2), 85-92. https://doi.org/10.5093/jwop2025a9 Funding This research was supported by grants PSI2017-83465-P and PID2020-117249GB-I00 by the Spanish Department of Science and Innovation (Ministerio de Ciencia e Innovación). References |
Cite this article as: Rodríguez-Muñoz, A., Antino, M., Díaz-Guerra, A., & Sepúlveda Paez, G. (2025). The Impact of a Workplace Sleep Program on Employee Well-being: A Pre-post Design Intervention Study. Journal of Work and Organizational Psychology, 41(2), 85 - 92. https://doi.org/10.5093/jwop2025a9
Correspondence: alfredro@ucm.es (A. Rodríguez-Muñoz).Copyright © 2026. Colegio Oficial de la Psicología de Madrid









 e-PUB
e-PUB CrossRef
CrossRef JATS
JATS